Abstract
Atorvastatin therapy in chronic subdural hematoma patients has attracted more and more clinical attention. To evaluate the efficacy of atorvastatin in the treatment of chronic subdural hematoma. A systematic literature search was performed in the PubMed, Embase, and Cochrane Library databases; related controlled trials comparing the efficacy of atorvastatin in the treatment of chronic subdural hematoma published from inception to December 2018 were collected. We used Cochrane risk of bias method to evaluate the quality of the included studies. Meta-analysis was used to analyze the included data by RevMan 5.3 software. Of the 53 retrieved studies, 6 trials were included. Results of meta-analysis showed that compared with chronic subdural hematoma patients without atorvastatin treatment, both in patients who have had surgery and those who have not, atorvastatin were effective in reducing the incidence of recurrence requires surgery (OR = 0.30, 95% CI 0.19–0.48, P < 0.00001). And improve the recovery rate of neurological function of patients (OR = 1.75, 95% CI 1.08–2.83, P = 0.02). This meta-analysis suggests that patients with chronic subdural hematoma can improve their prognosis after receiving atorvastatin. Additionally, the neurological function recovery appears to be improving by atorvastatin.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic subdural hematoma (CSDH) is one of the common diseases in neurosurgery, which is more common in the elderly with a history of mild trauma, and occurs in patients with trauma of 3 weeks or more. However, the therapeutic effect of CSDH is still not satisfactory. A long-term follow-up study of CSDH in the elderly found that the mortality rate of this disease can reach 32% even 1 year after the standard treatment [1]. With the proportion of elderly structure increasing year by year, the number of patients with cardiovascular and cerebrovascular diseases is also increasing. The use of anticoagulants is very common, and the number of refractory or recurrent CSDH is increasing; therefore, the cure rate of surgery is not ideal. Based on the results of literature studies in recent years, the formation of CSDH mainly includes the theories of local inflammatory hemorrhage in the dura, local hyperfibrinolysis, high osmotic pressure in the hematoma cavity, and repeated re-hemorrhage in the hematoma capsule [2]. Therefore, more and more studies tend to focus on increasing the hematoma absorption rate of subdural hematoma and hematoma capsule angiogenesis to reduce the recurrence rate of CSDH [2,3,4]. In recent years, statins have been used to regulate angiogenesis and repair nerve injury [5, 6]. Atorvastatin can activate Akt pathway, Notchl pathway, and endothelial nitric oxide synthase to improve the level of peripheral blood endothelial progenitor cells and angiogenic factors, and promote angiogenesis and the formation of functional blood vessels [6, 7]. Therefore, some medical centers have attempted to use atorvastatin to treat CSDH. Their results have demonstrated the efficacy of atorvastatin in the treatment of CSDH. This meta-analysis summarizes the data onto several comparative studies and comprehensively evaluates the efficacy of atorvastatin in the treatment of CSDH patients.
Materials and methods
Search strategy
A comprehensive review of the literature was searched on PubMed, EMBASE, and The Cochrane Library without language restrictions and the search time was from inception date until December 31, 2018. The following keywords were used: (Atorvastatin OR (3R,5R)-7-(2-(4-Fluorophenyl)-5-isopropyl-3-phenyl-4-(phenylcarbamoyl)-1H-pyrrol-1-yl)-3,5-di OR hydroxyheptanoic acid OR Atorvastatin Calcium OR Atorvastatin, Calcium Salt OR Liptonorm OR Lipitor OR Atorvastatin Calcium Hydrate OR Atorvastatin Calcium Anhydrous OR CI 981 OR CI-981 OR CI981 OR Atorvastatin Calcium Trihydrate) AND (Hematoma, Subdural, Chronic OR Subdural Hematoma, Chronic OR Chronic Subdural Hematoma OR Chronic Subdural Hematomas OR Hematoma, Chronic Subdural OR Hematomas, Chronic Subdural OR Subdural Hematomas, Chronic OR Hemorrhage, Subdural, Chronic).
Inclusion and exclusion criteria
The inclusion criteria are as follows: (1) Comparative studies include randomized controlled trials (RCTs) and retrospective studies; (2) At least one group of the CSDH patients had received the treatment of atorvastatin; (3) A minimum of 10 patients should be included in each trial. (4) There were no duplicated data in the experiment.
The exclusion criteria are as follows: (1) Case reports, review articles, letters, guidelines, technical notes, and congresses. (2) Single-arm studies.
Data extraction and quality assessment
Two researchers respectively performed title and abstract screening from the search query results, the full text of controlled trials were obtained, to determine whether inclusion criteria were met. Any discordance was settled by a third researcher. To extract data from the included studies, data of interest were extracted as follows: (1) Basic information included in the study, including the first author, year of publication, etc.; (2) Basic characteristics of the subjects, including the number of patients in the experimental group and the control group, and details of the intervention measures; (3) Outcome indicators and outcome measurement data concerned by the research; (4) Study design types and key factors for risk assessment of bias.
The methodological quality of all eligible studies was evaluated independently, in duplicate by 2 of the researchers was assessed by using the domain-based Cochrane Collaboration’s tool.
Statistical methods
This meta-analysis was completed based on the Review Manager Version 5.3 software provided by the Cochrane Collaboration (The Cochrane Collaboration, Oxford, UK). Odds ratio (OR) was selected as the index of dichotomy variables, and mean difference (MD) was used for measurement of continuous variables. 95% confidence interval (CI) was calculated. Heterogeneity between studies was analyzed by chi-squared value test (χ2) and evaluated by inconsistency index (I2), and a random-effects model was chosen to account for clinical diversity and methodologic variations among studies. If at least 8 trials were available for meta-analysis, funnel plots were drawn to analyze whether publication bias existed. Sensitivity analysis can be performed if the number of trials included in the study is sufficient.
Results
System literature review
Preliminary searches of PubMed, EMBASE, and The Cochrane Library identified 16, 27, and 9 citations, respectively. An additional study was obtained from the reference list of eligible studies. After eliminated the duplicate literature, read the title and abstract, excluded the obviously unrelated, non-clinical studies and reviews, a total of 19 clinical studies of atorvastatin for CSDH were collected, and the full text was further read to exclude the non-compliance with the inclusion criteria. Finally, a total of 6 studies were included, all of which were published. The PRISMA flow diagram of the study selection process of the literatures is shown in Fig. 1.
Study characteristics
Of these included studies, 3 [8,9,10] were RCT and the remaining 3 [11,12,13] were retrospective trials which were considered to be low risk. A total of 759 CSCD patients were included in all the analysis, including 122 patients treated with atorvastatin in 3 simple conservative treatment control trials and 256 patients treated with atorvastatin in 3 surgery combined medication control trials. All 6 trials included whether recurrence requires surgery in the outcome evaluation, 4 trials included neurologic scores. The characteristics of studies included in the meta-analysis are displayed in Table 1. The standard Cochrane Collaborations tools to make qualitative judgments on the quality testing of each study (Fig. 2). The main patient characteristics (age, gender, hematoma volume, etc.) showed no significant differences among these studies.
Efficacy
There are 6 studies enrolled in recurrence that requires surgery rate analyses (Fig. 3). NO heterogeneity (χ2 = 2.83, P = 0.73, I2 = 0%) was observed in these studies. The risk of recurrence that requires surgery was lower in the Atorvastatin group than in the control group, and the random-effects meta-analysis showed that difference was statistically significant (OR = 0.30, 95% CI 0.19–0.48, P < 0.00001). Further subgroup analysis showed that, the risk of recurrence that requires surgery rate with Atorvastatin was lower in both 3 simple conservative treatment trials (OR = 0.32, 95% CI 0.16–0.62, P = 0.0008) and 3 surgery combined medication trials (OR = 0.29, 95% CI 0.16–0.55, P = 0.0001).
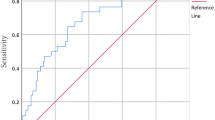
Four studies were enrolled in the neurological function recovery analyses. No heterogeneity (χ2 = 3.21, P = 0.36, I2 = 7%) was observed in these 6 studies (Fig. 4). The rate of neurological function recovery was lower in the control group than in the Atorvastatin group, and the random-effects meta-analysis showed that difference was statistically significant (OR = 1.75, 95% CI 1.08–2.83, P = 0.02).
Discussion
Most patients with CSDH suffer from subdural space hemorrhage due to damage of bridging vein or venous sinus and arachnoid granule caused by head trauma. When bleeding lasts for more than 3 weeks, hematoma will be surrounded by capsule to form hematocele [14]. Subsequent inflammation and the formation of hematoma outer membrane angiogenesis and repeated re-bleeding are key factors in the occurrence and development of CSDH. The subdural accumulation of the hematoma activates a local inflammatory response, causing fibroblasts to coat the new membrane surface of the hematoma. In addition, the rupture of fragile new blood vessels and immature blood vessels leads to repeated hemorrhage of hematomas, increasing membrane extravasation, and gradually increasing chronic subdural hematomas [15].
Atorvastatin is a statin that inhibits 3-hydroxy-3-methyl glutaryl coenzyme A reductase and acts by lowering LDL cholesterol levels. Atorvastatin has been proven that it is not only the local inflammation inhibitor, and angiogenesis mature agent [16, 17], and is based on a similar mechanism; through the atorvastatin treatment in the rat model of a subdural hematoma, it was found that a low dose atorvastatin can increase angiogenin and the expression of vascular endothelial growth factor, which could enhance blood vessels mature [18]. It has been confirmed that the level of endothelial progenitor cells (EPC) in peripheral blood of patients with CSDH is significantly lower than that of normal people [4], and the level of EPC in peripheral blood of relapsed patients is significantly lower than that of non-relapsed patients. EPC is the precursor of mature endothelial cells, which accumulate and form mature endothelial cells at the site of damaged vascular endothelium, so as to repair damaged vascular endothelium [19]. The study found that atorvastatin treatment for chronic subdural hematoma for 1–6 months can accelerate the absorption of hematoma and reduce the risk of borehole drainage [11]; therefore, it is recommended for the treatment of chronic subdural hematoma.
Although the general clinical conditions of some patients, such as age, hematoma volume, and whether there is brain atrophy, can bias the outcome of treatment, five [9,10,11,12,13] of them showed no difference in the age of patients between groups, so the effect of age on the prognosis of CSDH cannot be compared. Two [10, 13] of the three experiments providing admission hematoma volume showed no difference, and the other one [11] showed significantly higher average hematoma volume in the atorvastatin group than in the control group, but significantly improved the prognosis of the patients. Although some studies have suggested that glucocorticoid therapy and endovascular embolization therapy can improve the prognosis of CSDH patients, none of the 6 studies included in this paper involved this treatment regimen, which is also our future research direction.
This meta-analysis has enrolled 6 studies comprising 759 CSDH patients in the pooled analysis. All the 6 included studies collected the recurrence that requires surgery rate, and only 4 collected the neurological function recovery analysis; treatment modalities included both surgical and conservative treatment. In the documented trials, atorvastatin was treated for a low dose of 20 mg per day; the duration of medication ranged from 2 to 6 months. It was found in the comparison of the main prognostic indicators whether recurrence requires surgery, Atorvastatin can effectively reduce the risk of recurrence requiring surgery, both in patients that have undergone surgery and those who have not. In the secondary evaluation criteria, neurological function recovery, it can also be seen that the atorvastatin group can significantly improve the neurological function recovery of patients with CSDH compared with the control group.
In addition to the experimental control studies included in this meta-analysis, some single-arm studies also demonstrated the role of atorvastatin in improving the prognosis of patients with CSDH [13, 20]. Some studies even suggest that atorvastatin is as effective as surgery in patients with mild CSDH [21, 22]. Based on the limitation of the study, future trials are suggested to paying more attention to the information about patients’ life quality and prognosis. And samples, multi-center, double-blind, randomized, controlled clinical trials are still further needed to confirming the clinical effectiveness and safety of CSDH patients treatment atorvastatin.
Conclusions
The present study reports the results of a systematic review and meta-analysis of the atorvastatin in the treatment of CSDH patients. The results of our meta-analysis of 6 studies comprising 756 patients with CSDH revealed a decreased recurrence requires surgery rate after treatment of atorvastatin. Additionally, the neurological function recovery appeared to be improving by atorvastatin. Therefore, atorvastatin is effective in both conservative and surgical treatment of CSDH patients.
References
Miranda LB, Braxton E, Hobbs J, Quigley MR (2011) Chronic subdural hematoma in the elderly: not a benign disease. J Neurosurg 114(1):72–76
Wang D, Jiang R, Liu L, Dong JF, Zhang JN (2010) Membrane neovascularization and drainage of subdural hematoma in a rat model. J Neurotrauma 27(8):1489–1498
Liu L, Wei H, Chen F, Wang J, Dong JF, Zhang J (2011) Endothelial progenitor cells correlate with clinical outcome of traumatic brain injury. Crit Care Med 39(7):1760–1765
Song Y, Wang Z, Liu L, Wang D, Zhang J (2013) The level of circulating endothelial progenitor cells may be associated with the occurrence and recurrence of chronic subdural hematoma. Clinics (Sao Paulo) 68(8):1084–1088
Chen J, Cui X, Zacharek A, Chopp M (2009) Increasing Ang1/Tie2 expression by simvastatin treatment induces vascular stabilization and neuroblast migration after stroke. J Cell Mol Med 13(7):1348–1357
Chen J, Zacharek A, Li A, Cui X, Roberts C, Lu M, Chopp M (2008) Atorvastatin promotes presenilin-1 expression and Notch1 activity and increases neural progenitor cell proliferation after stroke. Stroke 39(1):220–226
Ma Y, Chen Z, Zou Y et al (2014) Atorvastatin represses the angiotensin 2-induced oxidative stress and inflammatory response in dendritic cells via the PI3K/Akt/Nrf 2 pathway. Oxidative Med Cell Longev 2014:148798
Chan DYC, Sun DTF, Chan DTM et al (2016) A prospective pilot study on the efficacy of Atorvastatin on chronic subdural haematoma. Surg Pract 20:10–11
Liu H, Luo Z, Liu Z et al (2016) Atorvastatin may attenuate recurrence of chronic subdural hematoma. Front Neurosci 10(6):1–6
Jiang R, Zhao S, Wang R, Feng H, Zhang J, Li X, Mao Y, Yuan X, Fei Z, Zhao Y, Yu X, Poon WS, Zhu X, Liu N, Kang D, Sun T, Jiao B, Liu X, Yu R, Zhang J, Gao G, Hao J, Su N, Yin G, Zhu X, Lu Y, Wei J, Hu J, Hu R, Li J, Wang D, Wei H, Tian Y, Lei P, Dong JF, Zhang J (2018) Safety and efficacy of atorvastatin for chronic subdural hematoma in Chinese patients: a randomized clinicaltrial. JAMA Neurol 75(11):1338–1346
Chan DYC, Chan DTM, Sun TFD et al (2017) The use of atorvastatin for chronic subdural haematoma: a retrospective cohort comparison study. Br J Neurosurg 31(1):72–77
Tang R, Shi J, Li X et al (2018) Effects of atorvastatin on surgical treatments of chronic subdural hematoma. World Neurosurg 117:e425–e429
Xu M, Chen P, Zhu X, Wang C, Shi X, Yu B (2016) Effects of atorvastatin on conservative and surgical treatments of chronic subdural hematoma in patients. World Neurosurg 91:23–28
Weigel R, Hohenstein A, Schilling L (2014) Vascular endothelial growth factor concentration in chronic subdural hematoma fluid is related to computed tomography appearance and exudation rate. J Neurotrauma 31(7):670–673
Lee KS, Bae WK, Bae HG, Yun IG (2000) The fate of traumatic subdural hygroma in serial computed tomographic scans. J Korean Med Sci 15(5):560–568
Wang B, Sun L, Tian Y, Li Z, Wei H, Wang D, Yang Z, Chen J, Zhang J, Jiang R (2012) Effects of atorvastatin in the regulation of circulating EPCs and angiogenesis in traumatic brain injury in rats. J Neurol Sci 319(1–2):117–123
Araujo FA, Rocha MA, Mendes JB et al (2010) Atorvastatin inhibits inflammatory angiogenesis in mice through down regulation of VEGF, TNF-alpha and TGF-beta1. Biomed Pharmacother 64(1):29–34
Wang D, Li T, Wei H, Wang Y, Yang G, Tian Y, Zhao Z, Wang L, Yu S, Zhang Y, Chen J, Jiang R, Zhang JN (2016) Atorvastatin enhances angiogenesis to reduce subdural hematoma in a rat model. J Neurol Sci 362:91–99
Liu HF, Qi XW, Ma LL, Yao DK, Wang L (2013) Atorvastatin improves endothelial progenitor cell function and reduces pulmonary hypertension in patients with chronic pulmonary heart disease. Exp Clin Cardiol 18(1):e40–e43
Wang D, Li T, Tian Y, Wang S, Jin C, Wei H, Quan W, Wang J, Chen J, Dong J, Jiang R, Zhang J (2014) Effects of atorvastatin on chronic subdural hematoma: a preliminary report from three medical centers. J Neurol Sci 336(1–2):237–242
Shofty B, Grossman R (2016) Treatment options for chronic subdural hematoma. World Neurosurgery 87:529–530
Soleman J, Nocera F, Mariani L (2017) The conservative and pharmacological management of chronic subdural haematoma. Swiss Med Wkly 147:w14398
Funding
This work was supported by the National Natural Science Foundation of China (81660734).
Author information
Authors and Affiliations
Contributions
Author contributions to the study and manuscript preparation include the following: conception and design: Chang He; analysis and interpretation of data: Pengfei Xia and Chang He; statistical analysis: Chang He; drafting the article: Chang He and Lanlan Chen; critically revising the article: all authors; reviewed submitted version of manuscript: all authors; supervision: Qiuli Zhang.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval is not required for this study.
Informed consent
Informed consent is not required for this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
He, C., Xia, P., Xu, J. et al. Evaluation of the efficacy of atorvastatin in the treatment for chronic subdural hematoma: a meta-analysis. Neurosurg Rev 44, 479–484 (2021). https://doi.org/10.1007/s10143-019-01218-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-019-01218-w