Abstract
Hemifacial spasm (HFS) is an involuntary paroxysmal contractions of the facial musculature, caused generally by vascular compression of the seventh cranial nerve at its root exit zone from the brain stem. The case of an adult man harbouring brain stem glioma (BSG) whose only neurological signs were left HFS and mild facial weakness is reported. Radiological and neurophysiological findings are described. No responsible vessel could be identified during surgery, but the causative lesion was found to be an astrocytic tumour encasing the facial nerve at its root exit zone from the brain stem. The rarity of such a condition prompted us to review the literature. Nine cases, including our patient presenting with HFS caused by BSG, are reviewed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hemifacial spasm (HFS) is a movement disorder characterised by intermittent painless, involuntary, spasmodic contractions of muscles innervated by the facial nerve in one side of the face only [7].
The theory of vascular compression by aberrant artery or vein loops, as championed by Jannetta et al. [8], has been widely accepted, with microvascular decompression (MVD) being the favoured treatment. However, there have been reports that the disease is associated with etiological factors other than compression merely by a vessel, and many authors have warned that a compressive mass lesion may be the underlying disease; thus, appropriate investigation is required before surgery [1–3, 7, 12].
Brain stem gliomas are among the rare tumours reported in association with HFS.
We present a patient with HFS due to pontine fibrillary astrocytoma. Magnetic resonance imaging (MRI) findings are demonstrated, and the pathophysiological mechanisms possibly involved are discussed.
Case report
A 52-year-old male patient presented with a 5-year history of progressive HFS beginning with left orbicularis oculi spasms, and often triggered by eating or drinking. He described the spasms as progressing from the eye, down to the face to eventually involve platysma, which is the characteristic pattern seen in typical HFS. However, with time the spasms became more tonic and also became associated with mild facial weakness, House-Brackmann grade II. The patient’s hearing was normal and he had no other cranial nerve palsy or neurological deficits.
Electrophysiological examination showed partial left lower motor neuron facial palsy. The left nasalis compound muscle action potential (CMAP) was markedly attenuated when compared with that on the right side (0.3 mV versus 2.8 mV). Concentric needle electromyography examination of the left orbicularis oculi and orbicularis oris revealed near continuous motor unit activity, which was of low voltage, and recruited to reduce interface patterns; although it was difficult to identify fibrillation or fasciculation, there was evidence of synkinesis.
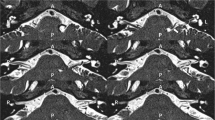
Cranial computerised tomography (CT) scan was carried out in another clinic, soon after the onset of symptoms, and failed to demonstrate any abnormality. In addition, serological tests for Lyme disease were positive and confounded the diagnosis. Following referral to our hospital, MRI revealed a non-enhancing, partly exophytic lesion growing from the left pons and adjacent medulla (Figs. 1, 2).
At operation, the exit zone of the facial nerve was found to be displaced caudally and was markedly distorted and flattened by the tumour, and no vascular compression of the facial nerve at its root exit zone was seen. The tumour extended down the origin of the glossopharyngeal nerve and up to the trigeminal sensory root, but did not involve these structures. The exophytic portion of the tumour was encountered first, and resection was performed by entering the centre of the lesion and gradually working toward the margins by using an ultrasonic aspirator. Resection was terminated when the tissue colour and texture began to look normal. We did not attempt dissection outside the tumour at the tumour-brainstem interface. The patient made a straightforward recovery and he was symptom free on the following day. Histologically, the tumour was reported as a fibrillary astrocytoma grade II, with areas of cellular pleomorphism.
After 18 months of follow-up, the tumour has expanded as shown on MRI, although the patient remains neurologically stable. He was offered radiotherapy for tumour control.
Discussion
Hemifacial spasm is a benign condition, characterised by unilateral paroxysmal chaotic and clonic spasms of the orbicularis occuli, paranasal, perioral and platysma muscles [14]. The aetiological factor could be contact between the facial nerve; an abnormal vascular loop is the most widely accepted hypothesis, and treatment by MVD proved to be effective in more than 80% of cases [3, 11].
Hemifacial spasm is not usually expected to be associated with neoplasm, although it is assumed to be a sign of large cerebello-pontine angle tumour. If associated with small tumour size, additional pathology, such as typical vascular compression, must be suspected and has to be explored at surgery. However, when HFS is the only sign, it cannot be distinguished from the idiopathic type. In exceptional cases, HFS has also been reported in the presence of brain stem gliomas [6, 12].
We believe the hypothesis that intrinsic pontine tumours typically grow to push the facial nuclei to around the edge of the tumour, and the close proximity of the tumour with the facial nucleus could generate abnormal impulses (presumably due to some direct pressure effect on the nucleus) and could be responsible for episodic contraction of facial muscles [2].
Our patient was offered surgical exploration in an attempt to cure his HFS and to obtain a good tissue biopsy from the tumour, knowing that his HFS could be due to direct facial nerve irritation by a vessel or the tumour (compressing or wrapping the nerve root or infiltrating the nerve nucleus or causing chemical irritation by neoplastic factor). However, considering the close relationship between the sixth and seventh cranial nerves in the lower pons, the absence of sixth nerve dysfunction, and improvement of the patient’s HFS after tumour debulking, strongly suggested that the mass effect of the lesion could be the cause of his symptoms, and makes a gross destructive effect by the tumour unlikely.
Re-growth of the tumour was very slow and was picked up before it caused recurrence of symptoms. Clearly it would be dangerous to attempt resection of this recurrent tumour, and partial removal would be of doubtful benefit, and might also present a risk for neurological deficit. Therefore, it was decided to treat the patient with fractionated stereotactic-guided radiation, or alternatively standard external beam radiotherapy.
It was thought initially that although unusual, it is possible that Lyme disease caused progressive infiltration of the left seventh nerve trunk, which then resulted in the gradual onset of synkinesis. In fact, cranial neuropathy is a common finding in neuroborreliosis and the vast majority of patients show unilateral or bilateral palsy of the seventh cranial nerve [5]. To the best of our knowledge, HFS caused by Lyme disease has not yet been reported in the English literature.
Eight similar cases have been reported in the literature, three of which occurred in patients who were not known to suffer from typical HFS. Among them, there were two cases with fourth ventricular gangliogliomas [2, 10], one pilocytic astrocytoma [13], one anaplastic astrocytoma [9], and one ependymoma of the fourth ventricle [11]. No tissue biopsy was obtained in two patients [4, 14], and histology was negative for tumour in one patient [6]. Four out of the nine patients diagnosed to have HFS associated with brain stem glioma were children, and two were due to ganglioglioma. These tumours are nearly always benign and are considered by some authors to be hamartomas [10].
For those cases of HFS where MVD is planned, MRI is important to demonstrate compressing vessels [3]. Other patients who prefer botulinum toxin injection treatment should also be screened with MRI to exclude unexpected pathology. It had been our practice to screen all patients with the diagnosis of HFS using MRI, regardless of the age at onset, duration and stability of symptoms.
In conclusion, hemifacial spasm is probably caused by a lesion almost anywhere along the course of the seventh nerve, including the nucleus within the pons. This case demonstrated that the facial nucleus can be the site of electrical dysfunction in HFS.
Although pathological facial nerve motor neurography is always suggestive of symptomatic or secondary form of HFS, clinical and electrophysiological examination do not allow differentiation between symptomatic and idiopathic HFS with any degree of certainty. Therefore we believe that investigation by MRI is mandatory in all patients who present with HFS, even if surgery is not contemplated.
References
Auger RG, Piepgras DG, Laws ER Jr (1986) Hemifacial spasm: results of microvascular decompression of the facial nerve in 54 patients. Mayo Clin Proc 61:640–644
Bills DC, Hanieh A (1991) Hemifacial spasm in an infant due to fourth ventricular ganglioglioma: case report. J Neurosurg 75:134–137
Coakham HB (2000) The microvascular treatment of trigeminal neuralgia, hemifacial spasm and glossopharyngeal neuralgia. In: Robertson JT, Coakham HB, Robertson JH (eds) Cranial base surgery. Churchill Livingston, New York, pp 543–564
Flueler U, Taylor D, Hing S, Kendall B, Finn JP, Brett E (1990) Hemifacial spasm in infancy. Arch Ophthalmol 108(6):812–815
Fritz C, Rosler A, Heyden B, Braune HJ (1996) Trigeminal neuralgia as a clinical manifestation of Lyme neuroborreliosis (Letter). J Neurol 243(4):367–381
Glocker FX, Krauss JK, Deuschl G, Seeger W, Lucking CH (1998) Hemifacial spasm due to posterior fossa tumours: the impact of tumour location on electrophysiological findings. Clin Neurol Neurosurg 100:104–111
Greenberg MS (1997) Neurovascular compression syndrome. In: Greenberg MS (ed) Handbook of neurosurgery, vol 1. Greenberg Graphics, Florida, pp 140–142
Jannetta PJ, Abbacy M, Maroon JC, Morales-Ramos F (1977) Aetiology and definitive microsurgical treatment of hemifacial spasm. Operative techniques and results in forty-seven patients. J Neurosurg 47:321–328
Krauss JK, Wahoo AK, Cerement R, Seeker W (1993) Facial myokymia and spastic paretic facial contracture as the result of anaplastic pontocerebellar glioma. Neurosurgery 32:1031–1034
Langston JW, Tharp BR (1976) Infantile hemifacial spasm. Arch Neurol 33:302–303
Rapana A, Guida F, Conti C, Rizzo G, Trincia G (1999) Ependymoma of the fourth ventricle presenting with hemifacial spasm: report of a case. Rev Neurol (Paris) 155(4):309–311
Samii M, Matthies C (1995) Acoustic neuromas associated with vascular compression syndromes. Acta Neurochir (Wien) 134:148–154
Sandberg DI, Souweidane MM (1999) Hemifacial spasm caused by pilocytic astrocytoma of the fourth ventricle. Paediatr Neurol 21(4):754–756
Westra I, Drummond GT (1991) Occult pontine glioma in a patient with hemifacial spasm. Can J Ophthalmol 26(3):148–151
Acknowledgements
We would like to acknowledge Dr. Abdul-Salam Al-Saleh, Specialist Registrar, Neurophysiology Department, Frenchay Hospital, Bristol, UK, for his valuable comments and assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Elgamal, E.A., Coakham, H.B. Hemifacial spasm caused by pontine glioma: case report and review of the literature. Neurosurg Rev 28, 330–332 (2005). https://doi.org/10.1007/s10143-005-0392-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-005-0392-7