Abstract
Both mild hypothermia (MH) and decompressive craniectomy (CE) have been shown to have neuroprotective effects in brain ischemia. We investigated a possible effect of MH and a combination of CE and MH (CE+MH) on the changes of infarction size, DNA fragmentation, and immunoreactivities for Bcl-2 and Bax after 24 h of permanent middle cerebral artery occlusion (MCAO) in rats. For the estimation of ischemic brain injury, we calculated the infarct size of the MCA region at 24 h after the MCAO. Terminal deoxynucleotidyl transferase-mediated dUTP–biotin in situ nick labeling (TUNEL) staining was performed for the detection of DNA fragmentation. Immunoreactivities for Bcl-2 and Bax were stained. Infarction size after permanent MCAO was significantly reduced by CE+MH treatment (P<0.01). Infarction size did not change significantly by application of MH alone (P>0.05). TUNEL staining was remarkably reduced both in MH-treated animals and in CE+MH-treated animals. Immunoreactivity for Bcl-2 was greatly induced both in MH-treated animals and in CE+MH-treated animals. Induction of immunoreactivity for Bcl-2 was obviously inhibited both in MH-treated animals and in CE+MH-treated animals. It suggests that temporary MH delays infarct evolution and ameliorates neuron apoptosis but does not significantly reduce definite infarction size. CE+MH not only ameliorates neuron apoptosis but also remarkably reduces infarction size.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Massive unilateral hemispheric infarction occurs in 10–15% of stroke patients and can lead to edema, increased intracranial pressure (ICP), and death. Prognosis for such patients is poor. In recent several years, the combined use of aggressive therapies for ischemic stroke, such as thrombolysis, hypothermia or decompressive hemicraniectomy, could potentially benefit such patients. The combined use of mild (and moderate) hypothermia (MH) and hemicraniectomy (CE) has been reported to improve outcome in both experimental research and clinical work [13]. In such cases, MH may be able to increase the therapeutic benefit of CE or expand the time window. Multiple mechanisms for decompression and hypothermia-induced neuroprotection have been identified [2, 8]. There are no data available in regard to the combined treatment of MH and decompressive CE on the effect of apoptosis. The present study was designed to evaluate the singular and combined effects of MH and CE on infarction size, and potential roles of MH and CE for attenuation of apoptosis were assessed by detection of DNA fragmentation, and immunostaining of the proapoptotic protein Bax and the antiapoptotic protein Bcl-2 in a rat model of middle cerebral artery occlusion (MCAO).
Materials and methods
Animal preparation
Thirty-six male Wistar rats (weight, 280–320 g) were allocated to three treatment groups: an MH )group, an MH+CE group, and a normothermia (NT) group, of 12 animals each (n=8, staining; n=4, histology). The study was approved by the animal committee of the Suzhou university. Animals were allowed free access to food and water before the procedure and were anesthetized with ketamine (4 mg/100 g) and xylazine (1.5 mg/100 g) by intramuscular injection. Monitoring of pH, PO2, PCO2, and blood pressure during anesthesia was performed with the use of a femoral artery catheter. Focal cerebral ischemia was induced with 4–0 nylon suture in all animals by endovascular occlusion of the MCA, as described by Koizumi et al. [20]. MH was induced as follows. In the MH group and the MH+CE group, 1 h after MCAO the whole-body was induced with the use of ice packs until a target temperature of 32°C in the temporalis muscle was reached and thereafter was maintained at 32°C until 67 h after MCAO. Cooling was performed at an average rate of 0.2°C/min; target temperature was obtained in roughly 25 min. After 5 h of hypothermia while under general anesthesia, rewarming to 37°C was performed gradually within 30 min Contralateral temporalis muscle and rectal probes were used to monitor temperature. Measurement of rectal temperature was performed throughout the anesthetic condition (before and during MCAO and hypothermia). Measurement of temporalis muscle temperature was started immediately after endovascular occlusion and monitored throughout the anesthetic condition. Contralateral temporalis muscle temperature has been reported to approximate closelyto the intraparenchymal brain temperature [24]. CE was performed in the animals according to Doerfler et al. [9] by creating a bone flap (10–5 mm) in the temporal and parietal bone with the use of a dental drill; additional bone was removed under microscopy. The dura was then opened in a cruciate incision. The effects of MH and MH+CE on infarction size, cell apoptosis and expression of the Bcl-2 and Bax proteins 24 h after MCAO were evaluated. MH was performed 1 h after MCAO and maintained for 5 h, till 24 h of survival. In the MH+CE group, MH was performed 1 h after MCAO and maintained for 5 h, After that, CE was performed till 24 h of survival. In the NH group, MCAO was performed and the animals’ temperature kept at 37°C till 24 h of survival.
Analysis of cerebral infarct volume
Rats were given an overdose of thiopental sodium and decapitated, and then the brain was quickly removed and frozen in liquid nitrogen. The brain was cut into a 2–mm thick coronal block. The brain slices were immersed in a 2% solution of 2,3,5–triphenyltetrazolium chloride in normal saline at 37°C for 30 min and then fixed in 10% phosphate-buffered formalin at 4°C. The brain slices were photographed using a charge-coupled device video camera, and the infarct volume was calculated according to a technique reported previously [4]. The infarct area of each section was measured using NIH Image software, version 1.62, and the infarct areas on each slice were summed and multiplied by slice thickness to give the infarct volume. Statistical analyses were performed using Student’s t-test.
Detection of DNA fragmentation and immunohistochemical study
For detection of DNA fragmentation and for histochemical stainings of Bcl-2/Bax, the rat forebrains were removed and quickly frozen at 24 h of occlusion. Coronal sections at the caudate and dorsal hippocampal levels were cut on a cryostat at −18°C to a 10-µm thickness and collected on glass slides coated with poly–L–lysine. NT group control sections were also obtained. Histochemical staining for TUNEL was performed with a kit (TACS TdT in situ apoptosis detection kit, no. 80–4625–00, Genzyme). After a detection of double-strand breaks in genomic DNA with 2,39–diaminobenzidine tetrahydrochloride (0.5 mg/ml in 50 mmol/l Tris–HCl buffer, pH 7.4), the sections were counterstained with methyl green according to the manufacturer’s protocol. Immunostaining for Bcl-2 and Bax were performed by the avidin–biotin peroxidase method (ABC) using a kit (Sigma). The freshly frozen sections were fixed for 10 min in ice-cold acetone and air-dried. Then the sections were rinsed three times in PBS (pH 7.4). After blocking with 10% normal rabbit serum for 2 h, the slides were incubated for 16 h at 4°C with the first antibody: a goat polyclonal antibody against Bcl-2 or Bax (Santa Cruz Biotechnology), diluted in PBS (1:200) containing 10% normal rabbit serum and 0.3% Triton X–100. Some sections were treated simultaneously without the first antibody. Endogenous peroxidase was blocked for 20 min with PBS containing 0.3% H2O2 and 10% methanol. The sections were then washed and incubated for 3 h with the second antibody (1:200), biotinylated rabbit anti-goat IgG, in the buffer, followed by incubation for 30 min with avidin-biotin-horseradish peroxidase complex. Staining was developed with 2,39-diaminobenzidine tetrahydrochloride (0.5 mg/ml in 50 mmol/l Tris–HCL buffer, pH 7.4), and counterstained with methyl green. The sections were examined by light microscope, and the stained cells in 0.25 mm2 of three random MCA areas were counted, summed, and categorized into four grades in the following manner: no staining, or a small (2–50), moderate (50–200), or large (200–500 or more) number of stained cells into –, +, 2+, and 3+, respectively.
Results
There was no significant difference in physiological parameters among the NT, MH, and MH+CE groups before MCAO (mean blood pressure: 89.4±12.6, 86.7±13. 1 and 87.8±9.8 mm Hg, respectively; PO2: 135.1±16.4, 133.6±24.0 and 138.0±21.0 mm Hg; PCO2: 43.21±2.7, 44.0±3.9 and 44.5±2.0 mm Hg; pH: 7.46±0.03, 7.44±0.05 and 7.45±0.02) or 12 h after MCAO (mean blood pressure: 97.4±14.0 mm Hg, 96.8±12.1 mm Hg and 97.8±11.7 mm Hg; PO2: 141.3±32.7,141.3±21.8 and 142.8±18.4 mm Hg; PCO2: 35.7±2.7, 34.5±3.1 and 36.7±2.4 mm Hg; pH: 7.47±0.02, 7.51±0.05 and 7.53±0.04).
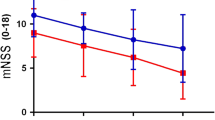
Infarction volume
In all three groups, the ischemic zone was consistently identified in the cortex and striatum of the left cerebral hemisphere. In the MH group, the infarct area (472.9±88.73 mm3) had a little reduction, but compared with that of the NT group (478.8±93.97 mm3) there was no statistical difference(P>0.05). The infarct area of the CE+MH group (316.1±53.06 mm3) was significantly reduced compared with NT group (P<0.01), as well as with the MH group (P<0.01). Figs. 1, 2 show a comparison of the NH group with the MH group, as well as the CE+MH group, on the hemispheric infarct area and volume. MH did not ameliorate infarction volume compared with NT. CE+MH showed a significant suppression of hemispheric infarct size after 24 h of MCAO.
TUNEL staining and the expression of Bcl-2 and Bax proteins
Heavy staining was seen in the brain sections at 24 h after the permanent MCAO. TUNEL-positive cells were distributed mainly in the ischemic core of the cerebral cortex and dorsal caudate of the occluded MCA area. Approximately 50–70% of cells were positive for TUNEL in the above-mentioned area, and the staining was essentially found in the nucleus of neuronal cells. However, TUNEL-positive cells were not evident in the inner boundary zone of the infarct. No TUNEL-positive cells were found in other areas of the ipsilateral hemisphere or in the contralateral side. The MH and CE+MH greatly reduced the number of TUNEL-positive cells at 24 h after permanent MCAO.
In all three experimental groups, Bcl-2 immunoreactivity in the ischemic core was absent or restricted to the nuclei of shrunken degenerated cells. The whole overlying cortex visibly exhibited obvious nuclear Bcl-2 immunoreactivity. MH and CE+MH significantly upregulated the number of Bcl-2–positive neurons in cortical areas in the proximity of the ventral and dorsal border zone, where neurons were morphologically intact. In three groups, Bax immunoreactivity in the ischemic core was absent or restricted to nuclei of shrunken degenerated cells. The adjacent border zone exhibited shrunken neurons with strong Bax immunoreactivity. MH and CE+MH significantly reduced the number of Bax immunoreactively positive neurons in cortical areas in close proximity to the ventral and dorsal border zone, where neurons were morphologically intact. The grade of TUNEL staining and immunoreactivities for Bcl-2 and Bax in the brain sections are summarized in Table 1.
Discussion
We have studied the singular and combined effects of MH and CE on permanent focal ischemia in rats. Our results suggest that temporary postischemic MH upregulates the expression of Bcl-2, reduces the expression of Bax and reduces the cell apoptosis in the penumbra cortex. But MH cannot reduce the infarction volume. Combination of CE and temporary MH not only upregulates the expression of Bcl-2, reduces the expression of Bax and reduces the cell apoptosis in the penumbra cortex, but also ameliorates infarction volume.
Recently, two clinical reports [6, 23] prospectively studied 71 and 52 patients, respectively; all revealed that early decompressive hemicraniectomy could significantly reduce mortality and morbidity. Two recently published experimental studies in rats by the same research group, using MCA occlusion, showed decompressive CE late at 4 and 12 h still resulted in significant improvement of neurological score and reduction of infarction size. But early CE is not beneficial in small thromboembolic MCA infarction [11, 12]. Our results confirm the experimental data available. Compared with controls, early CE hours after MCAO resulted in significantly reduced infarction size. But because mortality of this hemispheric MCA infarction model within the first 3 days is very high, we set our protocol to 24 h after vessel occlusion and did not attempt longer survival periods. Maybe it was not the final infarction volume. On the other hand, several experimental studies in rats demonstrated that infarction size in hypothermic and normothermic animals did not change significantly when the animals were killed 24 or 72 h after MCAO [18].
Studies about the protective effect of hypothermia on focal cerebral ischemia remain controversial. Permanent hypothermia has been shown to be very potent in reducing infarction size 6 h after MCAO. Zhang et al. [30] demonstrated that hypothermia is protective when induced 1 h after transient ischemia in a focal stroke model. In a model of transient focal cerebral ischemia, infarction volume was significantly reduced (32%) when MH was induced immediately after reperfusion and maintained for a prolonged period. However, a delay in hypothermia until 30 min after reperfusion failed to achieve statistical significance [29]. Early in 1992, two studies were able to demonstrate that moderate hypothermia permanently reduces infarction size when administered before or as early as 1 h after onset of ischemia [3, 18]. In contrast, several reported that hypothermia failed to modify permanent focal ischemia [26]. This is in accord with our results. The phenomenon of delayed neurodegeneration is well established in a focal ischemia model [10]. Thus, hypothermia may delay death in those neurons that have been irreversibly damaged. It may be difficult in small animals to maintain anesthesia and hypothermia for a prolonged time without severe side effects, but in the clinical setting MH can be administered over a long time. The beneficial effect of prolonged MH in severe MCA infarction in humans has been reported [29], but recent clinical research also showed that in patients with severe ischemic stroke, hypothermia seems to have no obvious beneficial effect compared with craniectomy [13].
Many mechanisms have been documented about the neuroprotective capability of MH and CE [14, 16, 19, 22, 28]. However, expression of pro and anti-apoptotic factors and apoptotic cell death in focal ischemia following MH and CE remains inadequately defined. Neuroprotection in this study predominantly occurred in the cortex, since Bcl-2 expression can be upregulated, as suggested previously [1]. In stroke models in which the cortex represents large parts of the penumbra, an attractive explanation for the mechanism of action of the neuroprotective effect of MH and CE could be the prevention of apoptotic cell death. Our results show apoptotic cell death has been confined to the penumbral border of the infarction, as determined by TUNEL staining, where cells are not so rapidly and severely damaged that they can undergo an apoptotic cell death rather than necrosis [21]. The presence and anatomic location of apoptotic cells, in particular after temporary focal cerebral ischemia, suggest that apoptosis may contribute to the final infarct size. As demonstrated in this study, a combination of MH and CE reduced expression of the proapoptotic protein Bax and counterregulated the antiapoptotic protein Bcl-2 in neurons located at the ischemic border zone. Neurons destined to develop apoptosis have been reported to express upregulation of the proapoptotic Bax protein and nuclear translocation paralleled by Bcl-2 decrease in the same neurons [15, 17]. On the other hand, Bcl-2 is expressed in cortical neurons that survive focal cerebral ischemia [5], Bcl-2 can be upregulated by MH only [1]. However, reseach has also shown that MH did not alter Bcl-2 and Bax expression in a relatively short period of time after ischemia [30].
Whether MH produces a permanent reduction in definite infarction size is controversial. However, even if MH only delays the onset of permanent neuronal damage, it may well increase the window of opportunity for some other form of therapy, such as pharmacological neuroprotection or craniectomy.
In conclusion, our results suggest that a combination of CE and MH upregulates the expression of Bcl-2, downregulates the expression of Bax, reduces cell apoptosis and reduces the infarction size after permanent focal cerebral ischemia in rats. MH can upregulate the expression of Bcl-2, downregulate the expression of Bax, reduce cell apoptosis, but not reduce the infarction size. The neuroprotective role of CE and/or MH might be associated with the inhibition of cell apoptosis.
References
Babu PP, Yoshida Y, Su M, Segura M, Kawamura S, Yasui N (2000) Immunohistochemical expression of Bcl-2, Bax and cytochrome c following focal cerebral ischemia and effect of hypothermia in rat. Neurosci Lett 291:196–200
Baker CJ, Fiore AJ, Frazzini VI, Choudhri TF, Zubay GP, Solomon RA (1995) Intraischemic hypothermia decreases the release of glutamate in the cores of permanent focal cerebral infarcts. Neurosurgery 36:994–1002
Baker CJ, Onesti ST, Solomon RA (1992) Reduction by delayed hypothermia of cerebral infarction following middle cerebral artery occlusion in the rat: a time-course study. J Neurosurg 77:438–444
Bederson JB, Pitts LH, Germano SM, Nishimura MC, Davis RL, Bartkowski HM (1986) Evaluation of 2,3,5–triphenyltetrazolium chloride as a stain for detection and quantification of experimental cerebral infarction in rats. Stroke 17:1304–1308
Chen J, Graham SH, Chan PH, Lan J, Zhou RL, Simon RP (1995) Bcl-2 is expressed in neurons that survive focal ischemia in the rat. Neuroreport 26:394–398
Cho DY, Chen TC, and Lee HC (2003) Ultra-early decompressive craniectomy for malignant middle cerebral artery infarction. Surg Neurol 60:227–233
Dietrich WD, Busto R, Globus MY, Ginsberg MD (1996) Brain damage and temperature: cellular and molecular mechanisms. Adv Neurol 71:177–194
Doerfler A, Forsting M, Reith W, Staff C, Heiland S, Schaebitz WR, von Kummer R, Hacke W, Sartor K (1996) Decompressive craniectomy in a rat model of “malignant” cerebral hemispheric stroke: experimental support for an aggressive approach. J Neurosurg 85:853–859
Du C, Hu R, Csernansky CA, Hsu CY, Choi DW (1996) Very delayed infarction after mild focal cerebral ischemia: a role for apoptosis? J Cereb Blood Flow Metab 16:195–201
Engelhorn T, Heiland S, Schabitz WR, Schwab S, Busch E, Forsting M, Doerfler A (2004) Dempressive craniectomy in acute cerebral ischemia in rats. Is there any benefit in smaller thromboembolic infarcts? Nurosci Lett 370:85–90
Engelhorn T, Kummer RV, Reith W, Forsting M, Doerfler A (2002) What is effective in malignant middle cerebral artery infarction: reperfusion, craniectomy, or both? An experimental study in rats. Stroke 33:617–622
Georgiadis D, Schwarz S, Aschoff A, Schwab S (2002) Hemicraniectomy and moderate hypothermia in patients with severe ischemic stroke. Stroke 33:1584–1588
Gerhard F Hamann, Dorothe Burggraf, Helge K Martens, Martin Liebetrau, Gabriele Jäger, Nathalie Wunderlich, Michael DeGeorgia, Derk W Krieger (2004) Mild to moderate hypothermia prevents microvascular basal lamina antigen loss in experimental focal cerebral ischemia. Stroke 35:764–769
Gillardon F, Lenz C, Waschke KF, Krajewski S, Reed JC, Zimmermann M, Kuschinsky W (1996) Altered expression of Bcl-2, Bcl-X, Bax, and c-Fos colocalizes with DNA fragmentation and ischemic cell damage following middle cerebral artery occlusion in rats. Mol Brain Res 40:254–260
Hofmeijer J, Schepers J, Veldhuis WB, Nicolay K, Kappelle LJ, Bar PR, Van der Worp HB (2004) Delayed decompressive surgery increases apparent diffusion coefficient and improves peri-infarct perfusion in rats with space-occupying cerebral infarction. Stroke 35:1476–1481
Isenmann S, Stoll G, Schroeter M, Krajewski S, Reed JC, Bahr M (1998) Differential regulation of Bax, Bcl-2, and Bcl-X proteins in focal cortical ischemia in the rat. Brain Pathol 8:49–63
Kader A, Brisman MH, Maraire N, Huh JT, Solomon RA (1992) The effect of mild hypothermia on permanent focal ischemia in rat. Neurosurgery 31:1056–1061
Kader A, Frazzini VI, Baker CJ, Solomon RA, Trifiletti RR (1994) Effect of mild hypothermia on nitric oxide synthesis during focal cerebral ischemia. Neurosurgery 35:272–277
Koizumi J, Yoshida Y, Nakazawa T, Ooneda G (1986) Experimental studies of ischemic brain edema, I: a new experimental model of cerebral embolism in rats in which recirculation can be introduced in the ischemic area. Jpn J Stroke 8:1–8
Li Y, Chopp M, Jiang N, Yao F, Zaloga C (1995) Temporal profile of in situ DNA fragmentation after transient middle cerebral artery occlusion in the rat. J Cereb Blood Flow Metab 15:389–397
LX Li, T Jiang, EZ Liu, CH Lin, QG Li, FM Yang, QS Dai (2003) Effect of intraischemic mild hypothermia on interleukin–1beta and monocyte chemoattractant protein–1 contents in ischemic core of rat cortex after transient focal cerebral ischemia. Zhonghua Yi Xue Za Zhi 83:541–543
Mori K, Nakao Y, Yamamoto T, Maeda M (2004) Early external decompressive craniectomy with duroplasty improves functional recovery in patients with massive hemispheric embolic infarction: timing and indication of decompressive surgery for malignant cerebral infarction. Surg Neurol 62:420–430
Onesti ST, Baker CJ, Sun PP, Solomon RA (1991) Transient hypothermia reduces focal ischemic brain injury in the rat. Neurosurgery 29:369–373
Ridenour TR, Warner DS, Todd MM, McAllister AC (1992) Mild hypothermia reduces infarct size resulting from temporary but not permanent focal ischemia in rats. Stroke 23:733–738
Scholler K, Zausinger S, Baethmann A, Schmid-Elsaesser R (2004) Neuroprotection in ischemic stroke-combination drug therapy and mild hypothermia in a rat model of permanent focal cerebral ischemia. Brain Res 1023:272–278
Schwab S, Schwarz S, Spranger M, Keller E, Bertram M, Hacke W (1998) Moderate hypothermia in the treatment of patients with severe middle cerebral artery infarction. Stroke 29:2461–2466
Winfree CJ, Baker CJ, Connolly Jr ES, Fiore AJ, and Solomon RA (1996) Mild hypothermia reduces penumbral glutamate levels in the rat permanent focal cerebral ischemia model. Neurosurgery 38:1216–1222
Yanamoto H, Hong SC, Soleau S, Kassel NF, Lee KS (1996) Mild ostischemic hypothermia limits cerebral injury following transient focal ischemia in rat neocortex. Brain Res 718:207–211
Yenari MA, Iwayama S, Chen D, Sun GH, Fujimura M, Morita-Fujimura Y, Chan PH, and Steinberg GK (2002) Mild hypothermia attenuates cytochrome c release but does not alter Bcl-2 expression or caspase activation after experimental stroke. J Cereb Blood Flow Metab 22:29–38
Zhang RL, Chopp M, Chen H, Garcia JH, Zhang ZG (1993) Postischemic (1 hour) hypothermia significantly reduces ischemic cell damage in rats subjected to 2 hours of middle cerebral artery occlusion. Stroke 24:1235–1240
Acknowledgement
This study was supported in part by a Japan–China Sasakawa Medical Fellowship.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jieyong, B., Zhong, W., Shiming, Z. et al. Decompressive craniectomy and mild hypothermia reduces infarction size and counterregulates Bax and Bcl-2 expression after permanent focal ischemia in rats. Neurosurg Rev 29, 168–172 (2006). https://doi.org/10.1007/s10143-005-0010-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-005-0010-8