Abstract
Frameless neuronavigation has been increasingly used in intracranial and spinal neurosurgery. However, the application of neuronavigation in orbital surgery has not yet been reported. The purpose of this study was to evaluate whether frameless navigation in the orbit provides sufficient clinical application accuracy and thus a useful tool in orbital surgery. A frameless infrared-based neuronavigation system (VectorVision, BrainLAB, Heimstetten, Germany) was used in the microsurgical removal of 11 orbital tumors (five cavernomas, three lymphomas, two dermoid tumors, and one rhabdomyosarcoma). The transconjunctival approach was performed in seven cases, lateral orbitotomy in three cases, and the extradural pterional approach was performed in one case. The surgery was successful and without any complications in all cases. The registration accuracy of the neuronavigation was between 1.8 and 2.2 mm, with a mean of 1.9 mm. Subtotal tumor debulking was performed in one case with lymphoma. One patient was only biopsied due to suspected systemic lymphoma disease. Total removal of the tumor could be accomplished in the other nine patients. Image guidance during orbital surgery offered excellent three-dimensional guidance on the surface of the intraorbital lesions, allowing a safer, more controlled surgery. The surgical targets in the orbit are fixed structures, thus no shifting occurs and continuous high intraoperative navigation accuracy can be achieved. The use of the navigation clearly reduces the operative risk and increases the effectiveness of microsurgical orbital procedures.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The neurosurgical treatment of space-occupying processes in the orbit bears a relatively high risk of either postoperative ocular deficits (“radical approach”) or of residual tumor (“conservative approach”). Therefore, special techniques of intraoperative topographic orientation and control (image-guided surgery) could play an important role here.
Several years of convincing experience with cranial neuronavigation suggested the application of the cranial software and registration method in the microsurgical removal of orbital lesions.
The possible impact of neuronavigation and its benefits in surgical removal of orbital lesions was studied in 11 patients harboring space-occupying lesions of the orbit.
This is the first report of the direct integration of cranial neuronavigation into orbital surgery.
Materials and methods
The series consisted of 11 patients (five male and six female) with orbital tumors. Follow-ups were available from 5 to 48 months, with a median of 18 months. The mean age was 51.6 years (range 33–71 years). Ophthalmologic examinations consisted of testing the patient’s visual acuity, fundoscopy and Goldmann perimetry for visual field defects. Ocular motor functions as well as the degree of proptosis were evaluated (Hertel exophthalometer). All patients underwent neurologic and clinical examinations. All patients underwent evaluation by magnetic resonance imaging (MRI) (with/without contrast agent) and computerized tomography (CT). Both T1- and T2-weighted MRI was performed in three planes. MRI follow-up examinations were scheduled at 3, 12 months postoperatively, and after that yearly. Table 1 lists the 11 patients, age, location and histology of the tumors, surgical approaches, extent of surgery, and the registration accuracy of the neuronavigation.
Histology and location
Five patients had cavernoma, two had primary orbital lymphoma (POL), one had secondary lymphoma, two had dermoid tumor, and one had rhabdomyosarcoma (Fig. 1). Five tumors were located intraconal (three cavernomas, one lymphoma, and one dermoid tumor) and two extraconal (cavernomas). Four tumors involved the intra- and extraconal space (two POL, one dermoid tumor, and one rhabdomyosarcoma). Bony involvement was found in one case with POL (patient no. 7). The lacrimal gland was affected in one patient with secondary lymphoma (patient no. 6). One large deep-lying intraconal cavernoma, located more laterally to the optic nerve and extended in the orbital apex, was totally removed via a navigated lateral orbitotomy (patient no. 2, Fig. 2).
MRI (left-sided) shows a medial intra-extraconal rhabdomyosarcoma, totally removed via a MRI-based navigated transconjunctival approach (patient no. 11) and further treated by chemotherapy and radiotherapy without recurrence (follow-up 48 months). Control MRI, taken 42 months later, showed no tumor (right-sided)
T2-weighted enhanced axial (a) and sagittal (c), and axial T1-weighted enhanced (b) magnetic resonance images showing a large cavernoma located intraconal more laterally to the optic nerve extended in the orbital apex region. The cavernoma was totally removed via an MRI-based navigated lateral orbitotomy (patient no. 2). Control axial T1-weighted MRI, taken 25 months later, showed no tumor (d)
Operative techniques
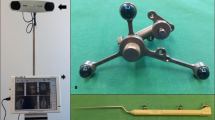
All patients underwent neuronavigation assisted microsurgical removal of their lesions (VectorVision, BrainLAB, Heimstetten, Germany). The fiducials were attached supraorbitally and to both mastoids, determining a wide registration area and allowing the caudal extension of the navigation space. Preoperative planning of the surgical approach was performed with respect to the exact location of the tumor and the results of the neuronavigation data prepared prior to surgery (Figs. 3, 4). The automatic fusion of image sets (CT, MRI T1-weighted, and MRI T2-weighted) was important and helpful to identify the exact extension of the lesion in four cases (patients no. 2, 6, 7 and 11). Before surgery the patients were fixed in the Mayfield Clamp. Intraoperative accuracy was checked using four precise bony landmarks. The transconjunctival approach (TCA) was performed in seven cases with lesions located medial or superior intra- and extraconal. The lateral orbitotomy were performed in three cases with lesions located lateral and basal to the optic nerve or in the orbital apex region (two patients with cavernoma and one with lymphoma). The extradural pterional approach was performed in one case with POL with extension intra-, extraconal, and intracranially with destruction of the ethmoidal cells (patient no. 7).
Pre-operative planning with the VectorVision navigation system (patient no. 11). The exact extension of the tumor and the access route could be evaluated according to data prepared prior to surgery. The target could be also virtually seen using the operative microscope integration tool of the neuronavigation
Pre-operative planning with the VectorVision navigation system (patient no. 2). The various steps in the operation and the access route are discussed using the display. The surgeon uses the pointer to indicate the route via which a large deep lying intraconal cavernoma, laterally to the optic nerve, will be removed (in this case using lateral orbitotomy)
Results
Proptosis with visual impairment was the main initial symptom in nine patients; five of them had a visual acuity of less than 5/10. Pain, photophobia, excessive tearing, and redness of the conjunctiva were the initial symptoms in two patients (patients no. 7 and 11). Restrictive motility disturbance was present in nine patients.
The registration accuracy of the neuronavigation was between 1.8 and 2.2 mm, with a mean of 1.9 mm. Intraoperative accuracy was checked before, during, and after removal of the lesions using four precise anatomical bony landmarks and remained continuously high. At the beginning of the operation, the neuronavigation system provided an accuracy of registration of 1.8–2.2 mm (mean 1.9 mm). Landmark and registration plausibility checks (with four precise anatomical landmarks, using of the microscope integration tool of the neuronavigation) during surgery documented stable accuracy.
Subtotal tumor debulking was performed in one case with POL (patient no. 7). One patient was only biopsied due to suspected systemic lymphoma disease (patient no. 6). Total removal of the tumor could be accomplished in the other nine patients.
Ophthalmological outcome
The postoperative visual acuity improved in seven of nine cases with visual impairment (four regained normal vision), and remained unchanged in two. Proptosis resolved completely in seven patients, improved in two patients, and was unchanged in one patient. Ocular motility recovered in seven patients and remained unchanged in two patients.
Discussion
Although a very small area, the orbit contains essential anatomical structures for the physiological function of vision, image processing, ocular motility, and for the patient’s physiognomic appearance, thus minutely detailed pre-operative planning of the surgical strategy and the surgical access route are essential. A fundamental prerequisite for this type of minimally invasive microsurgery is an exact knowledge of the localization of the lesion [2–4]. This information is provided by the modern imaging modalities (CT and MRI). However, it is sometimes difficult to transfer the information from the cross-sectional images to the real anatomy at the site of the operation.
The principle of coupling radiological images with real anatomical structures has been realized in modern neuronavigation techniques [1, 6].
With the incredible advances in image-guided neuronavigation including image-fusion techniques of CT and MR imaging, and the precision afforded by microsurgical techniques, lesions in and about the orbit can be approached in very direct surgical routes, mostly without intracranial invasion or significant external facial incisions.
The fact that the intraorbital surgical targets are mostly fixed lesions neighboring with bony structures reduces the intraoperative shifting effects, so continuous high intraoperative navigation accuracy can be achieved. The mean accuracy in our cases was 1.9 mm. The use of the microscope integration tool of the neuronavigation made the continuous intraoperative check of the accuracy possible. We found, that the shift in neuronavigation in orbital procedures was minimal, if compared with the shift in brain surgery. There have been several studies on the accuracy of navigation systems in brain surgery [1, 6–8]. Reinges et al. [6] studied the limits of conventional neuronavigation during microsurgical resection of supratentorial cerebral lesions in 61 patients, comparing superficial with subcortical brain shift. They found a mean superficial shift of 4.6 mm (1.6–10.8 mm, standard deviation 2.8 mm) and a mean subcortical shift of 3.5 mm (1.0–7.7 mm, standard deviation: 2.3 mm).
The situation in orbital lesions is different. The surgical targets in the orbit are fixed structures, no shift has to be expected, and continuous high intraoperative navigation accuracy can be achieved.
Intraoperative anatomical localization at the start of surgery in all cases was accurate to within 1.21 mm and remained stable during the operative procedure. So-called brain shift, which may cause increasing inaccuracy during the brain procedure, is unimportant when treating patients with lesions of the orbit.
In our previous publications, the microsurgical TCA to the orbit was advocated to remove intraorbital and especially intraconal lesions [2, 3]. The manipulation and search for the lesions can have many disadvantages and can cause scarring and injuries. The combination of this approach with the neuronavigation can clearly reduce the risks. The extent of removal could be also improved (total removal in nine of 11 patients). The introduction of the neuronavigation in orbital surgery helps reduce the surgical manipulation as far as possible and removal of the lesion as radically as possible.
The neuronavigation does not significantly prolong operative time (mean addition 8 min). We think that the clearly reduced operative manipulations and traumatizing of the intraorbital structures in neuronavigation assisted procedures counterbalance the relative additional operative time required.
This extremely visual type of surgical planning is also very helpful in neurosurgical training. The specific anatomy for each operation is displayed, and can be discussed and learned in detail. Nevertheless, neuronavigation cannot replace the surgeon’s own anatomical knowledge or his own ability to visualize structures in three dimensions.
The intra-operative accuracy of the system, taking into account all influencing factors—from image acquisition to individual manipulation of the instruments—was on average within 1.9 mm. The deviation of 1.9 mm proved to be negligible in intra-operative navigation, as the orbital structures movement is already in the millimeter range.
A prerequisite for accurate intraorbital navigation is that there must be no major shift in the position of the intraorbital structures at the beginning of surgery. This means that aspiration or opening of cystic components of the lesion before finding and identifying of the borders must be avoided. Due to the presence of enough bony anatomical landmarks, the navigation system has no major problems with structure shift in the orbit.
Conclusion
Image guidance during orbital surgery provides high accuracy for lesion targeting and permits excellent anatomic orientation, allowing a safer, more controlled surgery. The surgical targets in the orbit are fixed structures, thus no shifting occurs and continuous high navigation accuracy can be achieved. The use of the navigation clearly reduces the operative risk and increases the effectiveness of microsurgical orbital procedures.
The use of neuronavigation represents a major step towards the basic aim of modern orbital microneurosurgery; minimizing the surgical trauma.
References
Dorward NL, Alberti O, Palmer JD, Kitchen ND, Thomas DG (1999) Accuracy of true frameless stereotaxy: in vivo measurement and laboratory phantom studies. Technical note. J Neurosurg 90:160–168
Hejazi N, Hassler W, Farghaly F (1996) Microsurgical transconjunctival approach to the orbits. Initial retrospective analysis of experiences with the transconjunctival approach in 15 patients. Clinical and surgical aspects. Ophthalmologe 93:623–630 German
Hejazi N, Hassler W (1997) The transconjunctival microsurgical approach to the orbit: recent experience in 22 cases. Br J Neurosurg 11:310–317
Hejazi N, Claasen N, Hassler W (1999) Orbital and cerebral cavernomas: comparison of clinical, neuroimaging, and neuropathological features. Neurosurgical Rev 22:28–33
McCutcheon IE, Kitagawa RS, Demasi PF, Law BK, Friend KE (2004) Frameless stereotactic navigation in transsphenoidal surgery: comparison with fluoroscopy. Stereotact Funct Neurosurg 82:43–48
Reinges MH, Nguyen HH, Krings T, Hutter BO, Rohde V, Gilsbach JM (2004) Course of brain shift during microsurgical resection of supratentorial cerebral lesions: limits of conventional neuronavigation. Acta Neurochir (Wien) 146:369–377
Roberts DW, Hartov A, Kennedy FE et al (1998) Intraoperative brain shift and deformation: a quantitative analysis of cortical displacement in 28 cases. Neurosurgery 43:749–760
Schlaier JR, Warnat J, Dorenbeck U, Proescholdt M, Schebesch KM, Brawanski A (2004) Image fusion of MR images and real-time ultrasonography: evaluation of fusion accuracy combining two commercial instruments, a neuronavigation system and a ultrasound system. Acta Neurochir (Wien) 146:271–276; discussion 276–277
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hejazi, N. Frameless image-guided neuronavigation in orbital surgery: practical applications. Neurosurg Rev 29, 118–122 (2006). https://doi.org/10.1007/s10143-005-0007-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-005-0007-3