Abstract
We have investigated the plasma proteome using 2D gel electrophoresis and matrix-assisted laser desorption/ionization tandem time of flight from patients with high altitude pulmonary edema (HAPE). A complete proteomic analysis was performed on 20 patients with HAPE and ten healthy sea level controls. In total, we have identified 25 protein spots in human plasma and found that 14 of them showed altered changes in HAPE patients, which mainly were acute phase proteins (APPs), compliment components, and apolipoproteins among others. Among the APPs, haptoglobin α2 chain, haptoglobin β chain, transthyretin, and plasma retinol binding precursor showed overexpression in HAPE patients as compared to controls. To validate the result of proteomic analysis, two proteins were selected for enzyme-linked immunosorbent assay and Western blotting analysis. Our data conclusively shows that two proteins, haptoglobin and apolipoprotein A-I are upregulated in plasma of HAPE patients. These proteins may provide a fast and effective control of inflammatory damage until the subsequent mechanisms can begin to operate. Taken together, our findings further support the hypothesis that inflammatory response system is linked to the pathophysiology of HAPE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Impaired pulmonary gas exchange occurs in high-altitude pulmonary edema (HAPE) and in some persons with acute mountain sickness (AMS). HAPE is a form of noncardiogenic pulmonary edema that occurs in persons who ascend to altitudes above 2,500 m and remain there for 24–48 h or longer (Schoene 1985). Although the pathogenesis of HAPE is unknown, most reports focus on hydrostatic mechanisms leading to capillary leak and pulmonary edema. These mechanisms include hypoxic pulmonary vasoconstriction (Hultgren 1978; Bartsch et al. 1991), regional overperfusion (Hultgren 1978), or capillary rupture from high pulmonary vascular pressure and shear stress (West et al. 1991). Hypoxia, cold, exertion, fluid retention, and pulmonary vasoconstriction are also thought to contribute (Hultgren 1978; Houston 1960). Although pulmonary hypertension has been documented in many HAPE patients, (Hultgren 1978; Bartsch et al. 1991), there is also evidence that increased capillary permeability and inflammation may play an important role in the pathogenesis of HAPE. Evidence for the presence of inflammation in people with HAPE has come from several sources. Many patients with HAPE have fever, peripheral leukocytosis, and raised erythrocyte sedimentation rates (Schoene et al. 2001). Examination of bronchoalveolar lavage fluid from individuals with established HAPE has high levels of inflammatory cells (Schoene et al. 1986; 1988; Kubo et al. 1996; 1998). When bronchoalveolar lavage was performed in the field, in patients suffering from HAPE for 24 h or less, there was a marked increase in total cells, with macrophages being predominant, along with elevated levels of cytokines, including IL-6, IL-8, and tumor necrosis factor alpha (Kubo et al. 1998). In hospitalized patients later in the course of HAPE, the proportion of neutrophils increases and the observation is an inflammatory process similar in magnitude and pattern due to acute respiratory distress syndrome in the critical care unit (Kubo et al. 1996). Further evidence for an inflammatory component of HAPE is provided by the high rate of preceding respiratory tract infection in children who develop HAPE (Durmowicz et al. 1997), association between certain major HLA-immunomodulating alleles with susceptibility to HAPE (Hanaoka et al. 1998) and raised plasma E-selectin concentrations in hypoxemic climbers with AMS and HAPE (Grissom et al. 1997). Thus, in addition to pulmonary hypertension, signs of inflammation are present in HAPE.
Plasma proteins are useful targets for diagnostic, prognostic, and/or therapeutic development. With proteomic tools available recently, profiling of human plasma proteome becomes more feasible in searching for disease-related markers (Anderson and Anderson 2002). The presence of a particular protein and/or its isoforms in the plasma represents the likelihood of other biologically active molecules. These in turn may correspond to cellular functions. Since cellular functions often change during different disease states, the measurement of protein expression and modification may lead to the detection and identification of particular disease. To the best of our knowledge, there are no plasma or serum biomarkers with high sensitivity and specificity for the diagnosis and monitoring of HAPE. We therefore aimed to identify the differentially expressed proteins in the plasma of HAPE patients, as these have the potential to be developed as biomarker for the detection of disease. These differentially expressed proteins may also play roles in the disease development and manifestation.
In this study, the plasma proteome profile of healthy individuals was compared with that of patients with HAPE. The plasma proteome was first resolved by two-dimensional gel electrophoresis. The resulting gels were then compared to identify proteins that were differentially expressed. The identity of these proteins was determined by matrix-assisted laser desorption/ionization tandem time-of-flight mass spectrometry (MALDI-TOF/TOF MS) followed by unambiguous immunoassay. The results showed that most of the plasma proteins found in patients with HAPE are acute phase proteins (APPs), compliment components, and apolipoproteins generated by hypoxia-induced inflammation.
Materials and methods
Materials
Biolyte pH 3–10 ampholyte, 17 cm Immobiline DryStrips pH 5–8 (Biorad, Hercules, CA,USA), mineral oil, urea, bromophenol blue, CHAPS, agarose, acrylamide, Bis, Tris, sodium dodecyl sulfate (SDS), dithiothreitol (DTT), ammonium persulfate, iodoacetamide, tetramethylethylenediamine, sodium thiosulfate, silver nitrate, sodium carbonate, potassium ferricyanide, and Trypsin Singles™ proteomics grade were obtained from Sigma (St. Louis, MO, USA). Enzyme-linked immunosorbent assay (ELISA) kits of haptoglobin and apolipoprotein A-I were purchased from AssayPro (Triad South Drive, St. Charles, MO, USA). The primary antibodies to haptoglobin (mouse monoclonal, IgG1) and apolipoprotein A-I (rabbit polyclonal, IgG) were both from Santa Cruz Biotechnology, Inc. (Santa Cruz, CA, USA). Other analytical-grade chemicals used in this study were from domestic sources. All buffers were prepared with Milli-Q deionized water.
Subject characteristic and selection
Blood plasma of stringently selected HAPE patients (n = 20) and compared with healthy male sea level control (n = 10) were studied. The plasma from HAPE patients were collected at high-altitude medical research centre (HAMRC, Leh, India). The plasma from the healthy sea level controls were collected in Defence Institute of Physiology and Allied Sciences (Delhi, India). Written informed consent was obtained from all participating subjects after the procedure has fully explained. To prepare plasma, anticoagulants either EDTA, heparin, or sodium citrate were added to the blood specimens immediately after the blood was drawn to prevent clotting [EDTA plasma, 10 mL containing approximately 1.7 mg potassium EDTA; heparin plasma, 5 mL containing heparin one vial; sodium citrate plasma, 10 mL containing 1 mL of 0.118 mol/L (3.2%) citrate solution]. The specimens were then centrifuged at 1,500×g for 10 min/4°C to avoid hemolysis, decanted and transferred into Eppendorf tubes as aliquots. To each 1.0 mL plasma aliquots, 10 μL of protease inhibitor was added to obtain the reproducible results by 2DE analysis (Hulmes et al. 2004). The plasma samples were stored at −80°C until further analysis. The degree of AMS was determined by the Lake Louise score by the same interviewer. AMS was diagnosed when the Lake Louise score was >5. Chest radiogram was performed when the clinical assessment and/or the analysis of blood gas indicated HAPE by X-ray unit (TRS, Siemens) at HAMRC (Leh, India) with a fixed target to film distance of 140 cm at 95 kV and 3–6 mA/s. HAPE was diagnosed if the X-ray film showed interstitial and/or alveolar edema compared with the chest radiograph taken at lower altitude.
Depletion of high-abundance plasma proteins
Because albumin and immunoglobulin IgG collectively account for ~70% of the total plasma protein content (Hulmes et al. 2004), we selectively removed these proteins to enrich for proteins of lower abundance. A dye-based Proteoprep blue albumin and IgG depletion kit (Sigma Aldrich, Germany) was used according to the manufacturer’s instructions. Briefly, the provided suspended slurry medium were added to the spin columns, centrifuged and equilibrated at 8,000×g for 10 s. The spin columns were collected in fresh collection tube. To each spin column, 0.1 mL of the plasma sample was added to the packed medium bed, incubated for 10 min, centrifuged at 8,000×g for 60 s, and repeated the same step twice to remove the additional albumin. The twice depleted plasma remained in the collection tube and pooled for optimal protein recovery. The albumin/IgG-depleted plasma samples were stored at −80°C for long-term storage.
SDS-PAGE analysis
SDS polyacrylamide gel electrophoresis (SDS-PAGE) analysis was carried out with the Tris/glycine buffer system according to Laemmli (1970). Two microliters (20 μg) of albumin and IgG-depleted proteins of healthy sea level controls and HAPE patients were separated under reducing conditions on 12% SDS-PAGE mini gels (10 × 10.5 cm) at 250 V, 40 mA, and constant currents for 2 h and visualized by colloidal Comassie Blue G-250 or silver staining according to standard protocols. The gels were scanned in Ultra Lum Omega 16Vs system.
Acetone/TCA precipitation
A 100 μL of depleted plasma sample was diluted with 900 μL of 10% trichloroacetic acid (TCA) in acetone. The mixture was incubated overnight at −20°C and centrifuged at 15,000×g, 4°C for 10 min. The supernatant was removed, and 1,000 μL of 90% ice-cold acetone was added to wash the pellet. The sample was incubated at −20°C for 10 min and centrifuged as above. The acetone-containing supernatant was removed, and the pellet was air dried. For 2D gel electrophoresis, the protein pellet was suspended in 100 μL of lysis buffer containing 8 M urea, 2.5 M thiourea, 40 Mm Tris–HCl, 3% (w/v) CHAPS, and 0.5% (v/v) Igepal CA-630. The protein sample was stored frozen at −20°C until analysis.
First-dimension separation
The protein concentration in plasma was determined by Bradford assay and employed bovine albumin standards. Each sample was analyzed in triplicate. For each sample of plasma, HAPE patients, and sea level control, 750 μg of protein was reconstituted in rehydration buffer containing 7 M urea, 2 M thiourea, 1.2%, (w/v) CHAPS, 0.4% (w/v) ABS-14, 20 mM DTT, 0.25% (v/v), pH 3–10 ampholytes, and 0.005% (w/v) bromophenol blue (BPB) to a final volume of 300 μL. The samples were incubated (RT, 1 h) and then used to rehydrate 17-cm immobilized pH gradient (IPG) strips (Bio-Rad) with a pH 5–8 linear gradient. The strips were passively rehydrated for 18 h without current in a Protean isoelectric focus (IEF) cell (Bio Rad). First-dimension IEF was carried out at 20°C in a Protean IEF cell by the following protocol: 250 V for 1 h (slow ramping), changing the wicks every 30 min (to assist removal of ionic contaminants), 1,000 V for 1 h, linear ramping of 10,000 V to over 3 h, and a constant of 10,000 V until approximately 60 kVh was reached. Strips were removed and stored at −80°C until run on the second dimension.
Two-dimensional SDS-PAGE
After IEF, strips were equilibrated by agitating for 15 min in 50 mM of Tris–HCl, pH 8.8, 6 M urea, 30% (v/v) glycerol, 2% (w/v) SDS, 1% (w/v) DTT, and 0.01% (w/v) BPB, and then agitating for 15 min in 50 mM of Tris–HCl, pH 8.8, 6 M urea, 30% (v/v) glycerol, 2% (w/v) SDS, and 2.5% (w/v) iodoacetamide and 0.01% (w/v) BPB. The equilibrated IPG strips were slightly rinsed with Milli-Q water, blotted to remove excess equilibration buffer, and then applied to SDS-PAGE gels (20 cm × 20 cm × 1 mm 8–19% polyacrylamide [30% (w/v)acrylamide, 0.8% (w/v) bis-acrylamide, 37.5:1 stock] using a Protean II XL system (Bio-Rad) at 4°C at constant 10 mA per gel for 30 min followed by 35 mA per gel for 12 h in a running buffer containing 25 mM Tris, 192 mM glycine, and 0.1% (w/v) SDS until the dye front had run off the edge of the 2D gel.
Staining and imaging
After electrophoresis, proteins were visualized by modified silver staining procedure compatible with MS (Yan et al. 2000). The gels were fixed in 50% (v/v) methanol, 12% (v/v) acetic acid, and 0.05% (v/v) formaldehyde for at least 2 h. The fixed gels were rinsed with 50% (v/v) ethanol three times for 20 min each, then again sensitized with 0.02% (w/v) sodium thiosulfate followed by three washings with Milli-Q water each for 20 s. The gels were immersed in 0.1% (w/v) silver nitrate and 0.075% (v/v) formaldehyde for 20 min and rinsed with Milli-Q water twice for 20 s each. It was developed with 6% sodium carbonate and 0.05% (v/v) formaldehyde. Finally, the reaction was terminated by fixing with 50% (v/v) methanol and 12% (v/v) acetic acid. The stained gels were imaged using an Investigator™ ProPic II genomics solutions and the analysis of digitized images with Image Master 2D Platinum v.6 software (GE Healthcare). Automatic spot detection and matching of the gels were done, followed by manual rechecking of the matched and unmatched protein spots. The intensity volumes of the individual spots were normalized with the total intensity volume of all the spots present in each gel (%V). Differences of ≥1.5 in expression (ratio, %V) between matched spots were considered significant whenever a spot group passed statistical analysis (t test, P ≤ 0.05) and a second manual verification of the spots on the gel images. For those proteins with multiple spots in gel, such as haptoglobin, the sum of pixel volumes of individual spots from isoforms was used for analysis.
MS analysis
In-gel digestion with trypsin and extraction of peptides
The procedure for in-gel digestion of protein spots from silver-stained gels was performed. In brief, protein spots were excised from stained gels and cut into pieces. The gel pieces were destained and incubated for 30 min with 30 mM potassium ferricyanide and 100 mM sodium thiosulfate at room temperature. The gel pieces were rinsed several times with water to remove destaining solution. The gel pieces were washed for 15 min at room temperature with water and 50 mM NH4HCO3/acetonitrile. Enough acetonitrile was added to cover gel pieces for shrinking them. The gel pieces were rehydrated in 10 mM NH4HCO3 for 5 min, and equal volume of acetonitrile was added and removed after 15 min of incubation. The gel pieces were again covered with acetonitrile and removed. The gel pieces were dried in a vacuum centrifuge. The dried gel pieces were digested with 20 μL of trypsin (20 ng/μL, Trypsin Singles™ Proteomics Grade, Sigma), and the sample was incubated at 37°C overnight; the tryptic peptide was sonicated for 10 min and dried in a speed Vac. The dried peptides were extracted with 5 μL of 0.1% trifluoroacetic acid (TFA).
Matrix-assisted laser desorption/ionization tandem time of flight
Prior to mass spectromeric analysis, 10 mg/mL α-cyano-4-hydroxy cinnamic acid matrix was made in 70% acetonitrile and 0.03% TFA. Peptide extracts (0.5 μL) mixed with 0.5 μL of the matrix were manually spotted onto a 600-μm/384 well AnchorChip™ sample target (Bruker Daltonics) and dried at ambient temperature. Peptide mass spectra were recorded in the reflectron mode using an Ultraflex III TOF/TOF mass spectrometer (Bruker Daltonics) equipped with a 384-sample scout source. The ion acceleration voltage after pulsed extraction was 29,000 V. The instrument was calibrated using external standard calibration peptide mixture for the m/z range of 700–4,500 Da using the peptide peak of bradykinin (757.39 Da), angiotensin II (1,046.54 Da), angiotensin I (1,296.68 Da), substance P (1,347.73 Da), bombesin (1,619.82 Da), ACTH fragments 1–17 (2,093.08 Da) , ACTH fragments 18–39 (2,465.19 Da), somatostatin 28 (3,147.47 Da). The monoisotopic peak list was generated in post-processing S/W, and true peptide mass list was generated by Bruker Flex Analysis software version 3.0 and Biotools ver 3.1 without using the smoothing function, and the peak filter was applied to exclude the masses lower than 700 Da and the signal to noise ratio of 20. The generated peptide mass list was sent for the online data base search to find and match the protein identity. The search engine “MASCOT Server” (http://www.matrixscience.com) was used to obtain the protein identity by undertaking the peptide mass fingerprinting approach. Search was performed in NCBInr, MSDB, and SwissProt database with the following search parameter: mass tolerance, 50–100 ppm; species, Homo sapience; and maximum number of missed cleavages was set to 1 for all samples. Once the protein was identified, the identity was confirmed using tandem mass spectrometry. For each identified protein, at least one peptide was selected for MS/MS (TOF/TOF) to validate the protein identity. Instrument was used in the lift mode (TOF/TOF) to obtain the MS/MS spectra. Again, the Flex Analysis 3.0 and Biotools 3.1 S/W were used to generate the fragments mass list and the sequence Tag of peptide. The mass list was sent to database in the same way as was done in the case of above peptide mass fingerprinting approach. The mass tolerance error of 0.5–1 Da was used for MS/MS ion search. The MS/MS ion search confirmed the protein identity and provided the amino acid sequence of particular peptide.
Quantitative validation by enzyme-linked immunosorbent assay
To determine the correlation of haptoglobin and apolipoprotein A-I with HAPE, 30 plasma samples, including 20 HAPE patients and ten from normal control groups, were used for quantitative validation. The total haptoglobin and apolipoprotein A-I were quantified using competitive ELISA kit with the purified polyclonal antibody against haptoglobin and apolipoprotein A-I (Assaypro, USA) according to the manufacturer’s instructions. Briefly, individual plasma samples (1 μL) were diluted with mix diluent (2,000 μL for haptoglobin and 800 μL for apolipoprotein A-I). The diluted mixtures of 25 μL were added onto 96-well plate, and immediately, 25 μL of biotinylated haptoglobin and apolipoprotein A-I were added, mixed, and incubated for 1 h. After five washes with buffer, 50 μL of streptavidin–peroxidase conjugate was added and incubated for 30 min. After five washes, 50 μL of chromogen substrate was added and incubated for 10 min until the optimal blue color density developed. Fifty microliters of the stop solution was added to each well, and a yellow color developed and absorbance was measured on a microplate reader at a wavelength of 450 nm immediately.
Quantitative validation by Western blot analysis
The protein quantification of haptoglobin and apolipoprotein A-I were selected to be validated by Western blot analysis because the expression changes of these proteins were more obvious than that of the other proteins, and the obtaining of their antibodies was convenient. Briefly, plasma samples were first diluted ten times by 1× phosphate-buffered saline, and then total proteins (40 μg) were separated by SDS-PAGE and electro-blotted to nitrocellulose membrane. After being blotted with 5% nonfat dried milk in 1× TBST (25 mM Tris, pH 7.5, 150 mM NaCl, 0.1% Tween 20) overnight, membranes were incubated with primary antibodies for 2 h, followed by secondary antibody for another hour. All these experiments were conducted at room temperature. The immunocomplexes were visualized by chemiluminescence using the chemiluminescent peroxidase substrate kit (Sigma-Aldrich, St. Louis, MO, USA). The film signals were digitally scanned and then quantified using image J software.
Results
Removal of high abundance proteins from plasma and acetone/TCA precipitation
Albumin and IgG collectively account for ~70% of the total plasma proteins and therefore mask the presence of low abundance proteins. In order to maximize the coverage of disease-specific proteins, low abundance protein depletion of albumin and IgG was performed. Figure 1 demonstrates representative one-dimensional gel profile human plasma from control and HAPE patient. Depletion of human plasma resulted in significant removal of albumin and IgG at 64 kDa and IgG bands at 50 and 25 kDa (lanes 4 and 8) with no apparent loss of other proteins (lanes 2, 3, 6, and 7) in both the groups compared to undepleted plasma (lanes 1 and 5). Concomitant with the removal of albumin, there was a significant enhancement of the staining of several protein spots as observed in two-dimensional gel profiles in control and HAPE group. We carried out acetone/TCA precipitation for the removal of protease activity, biological contaminants, and enrichment of proteins.
Removal of high abundance proteins from plasma: depletion of human plasma of control and HAPE resulted in significant removal of albumin band at 64 kDa and IgG bands at 50 and 25 kDa (lanes 4 and 8) with no apparent loss of other proteins (lanes 2, 3, 6, and 7) in both the groups compared to undepleted plasma (lane 1 and 5)
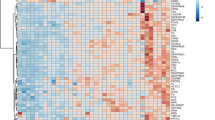
Proteome profiles of plasma patients with HAPE
The difference in protein profiles between HAPE patients and healthy controls was examined using 2DE with linear IPG strips of 17 cm ranging from pH 5–8. Each plasma samples were run on duplicate gels, and proteins were visualized by silver staining. Figure 2 shows the representative proteome profiles for HAPE patients. The relative intensities of the protein spots (normalized spot volume) were compared and analyzed between patients and healthy samples using 2DE gel analysis software. More than 300 protein spots in each silver stained gel can be visualized by 2D ImageMaster software. The quantitative evaluation of the differentially expressed plasma proteins in normal vs HAPE patients was performed using Student’s t test. In comparison with 2DE from the patients with healthy controls, many chains of spots that may represent different degrees of protein modification and/or degradation products were significantly varied. We compared 25 clear plasma protein spots in 2DE gel maps, which were analyzed by MALDI-MS and MS/MS (Fig. 2). Identification was based on NCBInr, MSDB and SwissProt database entries with the mascot search engine. In HAPE patients and healthy control, 25 common proteins were identified (Table 1). Table 1 lists the Swiss port accession numbers as well as the full names of the 25 protein spots, molecular mass, and pI values, and the number of matching peptides and protein amino acid sequence coverage by matching peptides. A comparison of 2DE gels from patients with those of healthy controls indicated that 14 spots were significantly upregulated. Among these upregulated protein spots, 11 protein spots clearly showed several fold increases in quantitative protein expression for HAPE patients and were selected for further analysis. The close-up images of upregulated proteins in the HAPE patients are presented in Fig. 3. Among these proteins, haptoglobin Hp-β chain expression was significantly increased in HAPE patients as compared to sea level healthy controls (p < 0.001). Only a marginal increase was observed in Hp-α2 chain in HAPE patients (p < 0.034) compared to healthy controls. Comparison of Hp-β spots from patients with those of healthy control indicated that some chains of Hp-β spots were representing different degree of modification or degradation products. In addition, the HAPE patients exhibited a significantly high content of ApoA-I (p < 0.001) when compared to sea level healthy controls (Table 2). We can see the representative gels of HAPE patients and controls in Fig. 2. Especially, the expression of Hp-β chain and ApoA-I (p < 0.001) displayed remarkably significant differences between the patients and control subjects.
A representative 2D gel of plasma from one HAPE patient with a pH range from 5 to 8. Distribution of expressed protein spots (marked by circle) and each spot number relate to data shown in Table 1
The representative gels of HAPE (A) and controls (B): Two-dimensional gels of human plasma from a subject with HAPE and a healthy comparison subject, displaying proteins with isoelectric points (pI) between 5 and 6 and molecular weights between 200 and 10 kDa. (C) The expression of haptoglobin-β (spot nos. 10-13), chain, and Apo A-I (spot nos. 8, 9) displayed remarkably significant differences (p < 0.001) between HAPE patients and control subjects. The expression of haptoglobin-α chain (spot nos. 2-6) showed only a marginal increase in HAPE patients (p = 0.034) as compared to healthy control subjects
Validation of Hp and ApoA-I with ELISA and Western blot analysis
To validate the result of proteomic analysis, two proteins were selected for ELISA and Western blotting analysis. We verified whether the expression patterns of selected proteins of haptoglobin and apolipoprotein A-I observed in 2DE gels paralleled those validated by ELISA and Western blot analysis. ELISA analysis of 20 patients with HAPE and ten healthy controls confirmed that concentrations of haptoglobin and apolipoprotein A-I were significantly increased in the plasma of patients with HAPE (Fig. 4). The mean plasma Hp concentration was 3,800 ± 754.24 μg/mL (mean ± SD) in HAPE patients vs 340 ± 67.987 μg/mL in sea level controls (p < 0.01); the mean APO A-I concentration was 5,088.9 ± 807.59 μg/mL in HAPE patients vs 688 ± 102.54 μg/mL in sea level controls (p < 0.01). The expression patterns of both proteins haptoglobin and apolipoprotein A-I were upregulated in plasma of HAPE patients (Fig. 5) and in agreement with 2DE results, so the results of ELISA analysis and Western blot analysis confirmed the reliability of the proteomic analysis.
ELISA analysis of patients with HAPE and healthy controls: ELISA confirmed that concentrations of haptoglobin (a) and apolipoprotein A-I (b) were significantly increased in the plasma of patients with HAPE. The mean plasma Hp concentration was 3,800 ± 754.24 μg/mL (mean ± SD) in HAPE patients vs 340 ± 67.987 μg/mL in sea level controls (p < 0.01); the mean Apo A-I concentration was 5,088.9 ± 807.59 μg/mL in HAPE patients vs 688 ± 102.54 μg/mL in sea level controls (p < 0.01)
Western blot analysis of haptoglobin and Apo A-I from plasma of three healthy controls and three patients with HAPE. Blots of haptoglobin (a) and apolipoprotein A-I (b) were represented along with their respective relative optical densities (ROD). Data represents the mean ± SD of three independent experiments. Densitometry analysis of results from Western blot, indicating significant change between the two groups compared by Student’s t test. *p < 0.05, significantly different vs control
Discussion
The present study demonstrated the use of proteomic analysis to study the nature of the identified proteins and their significance in disease pathogenesis. Our studies demonstrate that plasma analysis is not only more feasible but safer. In addition, because of the close communication between the alveolar space and blood circulation during lung inflammation, the pathological events occurring in the inflamed lung may be attainable by simply analyzing the patient’s plasma. This study has identified a number of overexpressed plasma proteins with different functions in patients with HAPE. Selected description of these proteins that may play a role in HAPE pathogenesis is discussed below.
In this study, we have found many APPs in plasma of patients with HAPE. These proteins may provide a fast and effective control of inflammatory damage until the subsequent defensive mechanisms can begin to operate (Moshage 1997). Our findings are in agreement with previous reports.
Along with inflammation caused by injury, trauma, autoimmunity, or infection, APP are massively synthesized and released systemically (Gabay and Kushner 1999a). This process is called the “acute phase response,” and it is supposedly induced in order to minimize and repair tissue damage. In general, concentration of various positive and negative regulators of APPs increases and decreases in response to inflammation (Cecilliani et al. 2002a). Among the acute phase proteins found in HAPE patients, transthyretin, haptoglobin β chain, compliment component 4A, haptoglobin α2 chain, and plasma retinol binding protein showed an increase in the plasma concentration during acute inflammation. Transthyretin (spot no. 1) has been shown to be a valuable prognostic factor of nutritional and inflammatory indices in patient’s acute respiratory failure (Schlossmacher et al. 2002). Because it is known as a negative APP (Doherty et al. 1998), i.e., an increase in the plasma concentration during acute inflammation, it indicates that the multimeric form of plasma transthyretin showed upregulation in HAPE. A persistent low level of serum transthyretin is predictive of lethality, whereas increased levels were associated with improved ventilatory performances. Additionally, transthyretin interacts with retinol binding protein (spot no. 7), thus enabling retinol transportation. Lower levels of transthyretin coincide with lower levels of retinol and retinol binding protein, as reported for ovarian cancer (Zhang et al. 2004). A decrease in transthyretin plasma levels is also seen in negative acute phase regulation during inflammation; correspondingly, its increased expression might be utilized as a biomarker for cancer. The transthyretin monomer may also serve as a marker to cerebrospinal fluid barrier disruption and lung cancer (Maciel et al. 2005). We also observed upregulation of transthyretin by threefold in plasma of HAPE patients, alongside an overexpression of retinol binding protein by twofold, respectively. Our findings in 2DE analysis suggested the conformational significance of transthyretin in patients with HAPE condition, and the development of a means for the detection of transthyretin in its conformation forms is needed to clarify its roles in the disease progression.
Complement component C4 (spot no. 25) is an acute phase protein and essential component of the effector arm of the humoral immune response. Compliment C4 exists as two isotypes, C4A and C4B. Although sharing >99% sequence identities, they have different hemolytic activities, covalent affinities to antigens and immune complexes, and serological reactivities (Schifferli et al. 1986). C4A may be functionally advantageous for ensuring the solubilization of antibody-–antigen aggregates (or inhibition of immune complexes (IC), and clearance of IC through binding to complement receptor CR1. In this study, we found that C4A was upregulated in blood plasma during inflammation.
Haptoglobin (Hp) (spot nos. 10–13) is a positive acute-phase plasma glycoprotein. It is synthesised by hepatocytes and is also found in adipose tissue and in lung, and is normally released in the blood during acute and chronic inflammation (Gabay and Kushner 1999b; Cecilliani et al. 2002b; Wang et al. 2001; Quaye 2008). Haptoglobin is considered to have significant antioxidant and anti-inflammatory properties because of its ability to bind hemoglobin, and haptoglobin depletion could add to vascular dysfunction in the hypertensive lung (Belcher et al. 2009). This might also affect the expression of other proteins because in silico analysis has been used to identify a group of genes that are coexpressed with haptoglobin and hemopexin and modulated in their absence (Fagoonee et al. 2006). Hemoglobin in plasma is instantly bound with high affinity to Hp, an interaction leading to the recognition of the complex by HbSR/CD 163 and endocytosis in macrophages (Madsen et al. 2001). Hp also acts as an antioxidant, has antibacterial activity, and plays a role in modulating many aspects of acute phase response. Hp is expressed at high levels in specific cells, including alveolar macrophages and eosinophils in diseased or inflamed human lung tissues, but not in the normal lung. Because the Hp–hemoglobin complex can be removed efficiently by alveolar macrophages, Hp synthesised by alveolar macrophages at the site of inflammation could contribute significantly to the clearance of hemoglobin and thus protect the lower respiratory tract against hemoglobin-mediated oxidative damage (Funmei et al. 2000). Hp has been identified as one of the serum angiogenic factors required for the proliferation and differentiation of endothelial cells (Cid et al. 1993; Cockerill et al. 1995a). Increased serum concentration in chronic inflammatory and (or) ischemic conditions is important for tissue repair and promotion of the growth of collateral vessels (Padma and Valli 1989). In this study, we found that Hp was upregulated in HAPE plasma patients. The concentration of plasma Hp increased to 3,800 ± 754.24 μg/mL (mean ± SD), whereas that of controls was 340 ± 67.987 μg/mL (p < 0.01). We might conclude that overexpression of Hp might attenuate hypoxia-induced inflammation in HAPE patients.
Apolipoprotein A-I (Apo A-I) (spot nos. 8 and 9) is the major protein of high-density lipoprotein (HDL), comprising about 70% of total HDL protein. The best characterized functions of Apo A-I are related to its role in reverse cholesterol transport and include lipid and cholesterol binding, lecithin/cholesterol acyl transferase activation, and receptor binding (Rodrigueza et al. 1997). Beyond its role in cholesterol metabolism, there are many other disparate activities attributed to apo A-I (and HDL) that may be physiologically relevant, some of which may also contribute to apo A-I’s anti-atherogenic properties, such as its anti-inflammatory and antioxidant activities (Cockerill et al. 1995b). Plasma HDL, quantified by either its cholesterol or Apo A-I content, is the best single predictor of coronary artery disease (CAD), with high HDL levels being correlated with low CAD (Calabresi and Franceschini 1997). In terms of the mechanism of ApoA-I, previous researchers showed that ApoA-I could bind LPS to interrupt activation of macrophage (Ma et al. 2004), inhibit LPS-activated macrophage to release inflammatory cytokines (Yan et al. 2006), and inhibit activation of neutrophils (Liao et al. 2005). Recently, a study examined the effect of ApoA-I overexpression on LPS-induced systemic inflammation and multiple organ injury in mice and concluded that ApoA-I overexpression has a protective effect on LPS- induced multiple organ injury (Li et al. 2008). Increasing studies provide new evidence supporting the notion that HDL plays a protective role in the lung. ABCA1, which interacts with lipid-poor Apo A-I, was earlier shown to be essential for maintaining normal lipid composition and architecture of the lung as well as respiratory physiology (Bates et al. 2005). More recently, proteomic studies revealed that homozygous sickle cell anemia patients with pulmonary arterial hypertension (PAH) consistently had lower Apo A-I levels than sickle patients without PAH (Yuditskaya et al. 2009). Interestingly, genetic deletion of endothelial lipase resulted in a nearly twofold increase in HDL, which was credited with decreasing airway hyperresponsiveness and pulmonary inflammation in ovalbumin-sensitized BALB/c mice (Otera et al. 2009). There is emerging evidence that Apo A-I plays a critical role in protecting pulmonary artery and airway function as well as preventing inflammation and collagen deposition in the lung (Wang et al. 2010). In this study, Apo A-I was found to be upregulated in HAPE patients as confirmed by ELISA and Western blotting, suggesting the anti-inflammatory role of Apo A-I in HAPE.
Considering that the expression of Hp and Apo A-I show roughly twofold variances in HAPE, which were acceptable criteria for disease biomarkers in differential display techniques, we suggest that these two proteins might become biomarkers for HAPE diagnosis and prognosis. Furthermore, changes in the proteome observed in the analysis require validation over a much larger sample size for sensitivity and specificity. While it is unlikely that the change in expression of a single protein will be specific indicator for a particular disease, an understanding of different proteins behave in combination may provide an indication of the occurrence of disease. Ongoing investigation into the roles of these differentially expressed proteins will determine their possible use and specificity in the diagnosis and monitoring of HAPE.
Study limitations
One important limitation of our study is that the protein quantification is based on only 2D gels. Most of the proteins have multiple isoforms that differ in electrophorectic mobility. We could not estimate all the isoforms of the identical protein in 2D gel, and this may affect the accuracy of the single protein quantification. Second limitation of the 2D gel-based proteomic approach is the variable validity of the protein identification. Some gel spots may contain more than one protein. The identification of proteins from peptide sequence is calculated as a high probability. Therefore, the validity of the approach has to be confirmed by different methods. However, since only a few of the respective antibodies against the observed proteins are currently available, it remains necessary to confirm the validity of our gel-based protein expression data by antibody-based techniques. (e.g., Western blotting) whenever antibodies become available.
References
Anderson NL, Anderson NG (2002) The human plasma proteome: history, character, and diagnostic prospects. Mol Cell Proteomics 1:845–867
Bartsch P, Maggiorini M, Ritter M, Noti C, Vock P, Oelz O (1991) Prevention of high-altitude pulmonary edema by nifedipine. N Engl J Med 325:1284–1289
Bates SR, Tao JQ, Collins HL, Francone OL, Rothblat GH (2005) Pulmonary abnormalities due to ABCA1 deficiency in mice. Am J Physiol Lung Cell Mol Physiol 289:L980–L989
Belcher JD, Beckman JD, Balla G, Balla J, Vercellotti G (2009) Heme degradation and vascular injury. Antioxidant Redox Signal 12:233–248
Calabresi L, Franceschini G (1997) High density lipoprotein and coronary heart disease: insights from mutations leading to low high density lipoprotein. Curr Opin Lipidol 8:219–224
Cecilliani F, Giordano A, Spagnolo V (2002) The systemic reaction during inflammation: the acute phase proteins. Protein Pept Lett 9:211–223
Cid MC, Grant DS, Hoffman GS, Auerbach R, Fauci AS, Kleinman HK (1993) Identification of haptoglobin as an angiogenic factor in sera from patients with systemic vasculatis. J Clin Invest 91:977–985
Cockerill GW, Gamble JR, Vadas MA (1995a) Angiogenesis: model and modulators. Int Rev Cytol 159:113–160
Cockerill GW, Rye KA, Gamble JR, Vadas MA, Barter PI (1995b) High-density lipoproteins inhibit cytokine-induced expression of endothelial cell adhesion molecules. Arterioscler Thromb Vasc Biol 15:1987–1994
Doherty NS, Littman BH, Reilly K, Swindell AC, Buss JM (1998) Analysis of changes in acute-phase plasma proteins in acute inflammatory response and in rheumatoid arthritis using two-dimensional gel electrophoresis. Electrophoresis 19:355–363
Durmowicz AG, Noordeweir E, Nicholas R, Reeves JT (1997) Inflammatory processes may predispose children to high-altitude pulmonary edema. J Pediatrics 130:830–840
Fagoonee S, Di Cunto F, Vozzi D, Volinia S, Pellegrino M, Gasparini P, Silengo L, Altruda F, Tolosano E (2006) Microarray and large-scale in silico-based identification of genes functionally related to haptoglobin and/ or hemopexin. DNA Cell Biol 25:323–330
Funmei Y, Andrew JG, Damon CH, Frank JW, Christi AW, Jacqueline J (2000) Pulmonary expression of the human haptoglobin gene. Am J Respir Cell Mol Biol 23:277–282
Gabay C, Kushner I (1999) Acute-phase proteins and other systemic responses to inflammation. N Engl J Med 340:448–454
Grissom CK, Zimmerman GA, Whatley RE (1997) Endothelial selectins in acute mountain sickness and high-altitude pulmonary edema. Chest 112:1572–1578
Hanaoka M, Kubo K, Yamazaki Y, Miyahara T, Matsuzawa Y, Kobayashi T, Sekiguchi M, Ota M, Watanabe H (1998) Association of high-altitude pulmonary edema with major histocompatibility complex. Circulation 97:1124–1128
Houston CS (1960) Acute pulmonary edema of high altitude. N Engl J Med 263:478–480
Hulmes JD, Betheab D, Ho K, Huang S-P, Ricci DL, Opiteck GJ, Hefta SA (2004) An investigation of plasma collection, stabilization, and storage procedures for proteomic analysis of clinical samples. Clin Proteomics J 1:17–31
Hultgren HN (1978) High-altitude pulmonary edema. In: Staub N (ed) Lung water and solute exchange. Marcel Dekker, New York, pp 437–449
Kubo K, Hanaoka M, Hayano T, Yamaguchi T, Hayano M, Hayasaka M, Koizumi T, Fujimoto K, Kobayashi T, Honda T (1996) Cytokines in bronchoalveolar lavage fluid in patients with high altitude pulmonary edema at moderate altitude in Japan. Thorax 51:739–742
Kubo K, Hanaoka M, Hayano T, Miyahara T, Hachiya T, Hayasaka M, Koizumi T, Fujimoto K, Kobayashi T, Honda T (1998) Inflammatory cytokines in BAL fluid and pulmonary hemodynamics in high-altitude pulmonary edema. Respir Physiol 111:301–310
Laemmli UK (1970) Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature 227:680–685
Li Y, Dong, Ji B, Wu MP (2008) Human ApoA-I overexpression diminishes LPS-induced systemic inflammation and multiple organ damage in mice. Eur J Pharm 590:417–422
Liao XL, Lou B, Ma J, Wu MP (2005) Neutrophils activation can be diminished by apolipoprotein A-I. Life Sci 77:325–335
Ma J, Liao XL, Lou B, Wu MP (2004) Role of apolipoprotein A-I in protecting against endotoxin toxicity. Acta Biochim Biophys Sin (Shanghai) 36:419–424
Maciel CM, Junqueira M, Paschoal ME, Kawarmura MT, Carvalho MG, Domont GB (2005) Differential proteomic serum pattern of low molecular weight proteins expressed by adenocarcinoma lung cancer patients. J Expc Ther Oncol 5:31–38
Madsen M, Graversen JH, Moestrup SK (2001) Haptoglobin and CD 163: captor and receptor gating hemoglobin to macrophages lysosomes. Redox Rep 6:386–388
Moshage H (1997) Cytokines and the hepatic acute phase response. J Patho 181:257–266
Otera H, Ishida T, Nishiuma T, Kobayashi K, Kotani Y, Yasuda T, Kundu RK, Quertermous T, Hirata K, Nishimura Y (2009) Targeted inactivation of endothelial lipase attenuates lung allergic inflammation through raising plasma HDL level and inhibiting eosinophil infiltration. Am J Physiol Lung Cell Mol Physiol 296:L594–L602
Padma T, Valli W (1989) ABO blood groups, intestinal phosphatase and haptoglobin types in patient with serum hepatitis. Hum Hered 39:345–350
Quaye IK (2008) Haptoglobin, inflammation and disease. Trans R Soc Trop Med Hyg 102:735–742
Rodrigueza WV, Williams KJ, Rothblat GH, Philips MC (1997) Remodeling and shutting: mechanisms for the synergistic effects between different acceptor particles in the mobilization of cellular cholesterol. Arterioscler Thromb Vasc Biol 17:383–393
Schifferli JA, Steiger G, Paccaud JP, Sjoholm AG (1986) Differences between C4A and C4B in the handling of immune complexes: the enhancement of CR1 binding is more important than the inhibition of immunoprecipitation. Clin Exp Immunol 63:473–477
Schlossmacher P, Hasselmann M, Meyer N, Kara F, Delabranche X, Kummerlen C, Ingenbleek Y (2002) The prognostic value of nutritional and inflammatory indices in critically ill patients with acute respiratory failure. Clin Chem Lab Med 40:1339–1343
Schoene RB (1985) Pulmonary edema at high altitude: review, pathophysiology, and update. Clin Chest Med 6:491–507
Schoene RB, Hackett PH, Henderson WR, Sage EH, Chou M, Roach RC, Mills WJ, Martin TR (1986) High-altitude pulmonary edema: characteristics of lung lavage fluid. JAMA 256:63–69
Schoene RB, Swenson ER, Pizzo CJ, Hackett PH, Roach RC, Mills WJ Jr, Henderson WR Jr, Martin TR (1988) The lung at high altitude: bronchoalveolar lavage in acute mountain sickness and pulmonary edema. J Appl Physiol 64:2605–2613
Schoene RB, Hultgren HN, Swenson ER (2001) High-altitude pulmonary edema. In: Hornbein TF, Schoene RB (eds) High altitude: an exploration of human adaptation. Mercel Dekker, New York, pp 777–814
Wang Y, Kinzie E, Berger FG, Lim SK, Baumann H (2001) Haptoglobin, an inflammation-inducible plasma protein. Redox Rep 6:379–385
Wang W, Xu H, Shi Y, Nandedkar S, Zhang H, Gao H, Feroah T, Weihrauch D, Schult ML, Jones DW, Jarzembowski J, Sorci-Thomas M, Pritchard KA (2010) Genetic deletion of apolipoprotein A-I increases airway hyperresponsiveness, inflammation, and collagen deposition in the lung. J Lipid Res 51:2560–2570
West JB, Tsukimoto K, Mathieu-Costello O, Prediletto R (1991) Stress failure in pulmonary capillaries. J Appl Physiol 70:1731–1742
Yan YX, Wait R, Berkelman T, Harry RA, Westbrook JA, Wheeler CH, Dunn MJ (2000) A modified silver staning protocol for visualization of proteins compatible with matrix-assisted laser desorption/ionization and electrospray ionization-mass spectrometry. Electrophoresis 21:3666–3672
Yan YJ, Li Y, Lou B, Wu MP (2006) Beneficial effects of ApoA-I on LPS-induced acute lung injury and endotoxemia in mice. Life Sci 79:210–215
Yuditskaya S, Tumblin A, Hoehn GT, Wang G, Drake SK, Xu X, Ying SA, Chi H, Remaley AT, Shen RF, Munson PJ, Suffredini AF, Kato GJ (2009) Proteomic identification of altered apolipoprotein patterns in pulmonaryhypertension and vasculopathy of sickle cell disease. Blood 113:1122–1128
Zhang Z, Bast RC Jr, Yu Y, Li J, Sokoll LJ, Rai AJ, Rosenzweig JM, Cameron B, Wang YY, Meng XY, Berchuck A, Van Haaften-Day C, Hacker NF, de Bruijn HW, van der Zee AG, Jacobs IJ, Fung ET, Chan DW (2004) Three biomarkers identified from serum proteomic analysis for the detection of early stage ovarian cancer. Cancer Res 64:5882–5890
Acknowledgments
Financial support for this study is provided by a grant from TC/321/Task—145 (YA)/ DIPAS/2008, Defence Research Development Organization (DRDO), Ministry of Defence, Government of India. We gratefully acknowledge the staff of High Altitude Medical Research, Leh for helping with the sample collection.
Author information
Authors and Affiliations
Corresponding author
Additional information
Y. Ahmad and D. Shukla contributed equally to this work.
Rights and permissions
About this article
Cite this article
Ahmad, Y., Shukla, D., Garg, I. et al. Identification of haptoglobin and apolipoprotein A-I as biomarkers for high altitude pulmonary edema. Funct Integr Genomics 11, 407–417 (2011). https://doi.org/10.1007/s10142-011-0234-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10142-011-0234-3