Abstract
Purpose
Nonoperative management (NOM) has been widely accepted as one of the standard treatments for patients with acute appendicitis. However, predictive factors for the failure of NOM have not been thoroughly investigated.
Methods
A total of 196 patients with acute appendicitis underwent NOM between April 2014 and December 2020. Of these 196 patients, 24 patients failed NOM and required emergency surgery (failure group: n = 24), while the other 172 patients were successfully treated with NOM (success group: n = 172). These two groups were compared, and the predictive factors for the failure of NOM were investigated.
Results
The number of patients who had a previous history of stroke was significantly increased in the failure group (12.5% vs. 2.9%, p = 0.026). Incarceration of an appendicolith on CT images was significantly associated with the failure group (20.8% vs. 1.7%, p < 0.001), while neither the presence of an appendicolith nor abscess was associated. The presence of periappendiceal fluid was significantly associated with the failure group (50.0% vs. 26.7%, p = 0.019). The incarceration of an appendicolith (p < 0.001, odds ratio = 19.85) and periappendiceal fluid (p = 0.009, odds ratio = 3.62) were found to be independent risk factors for failure of NOM. Neither the presence of an appendicolith nor abscess was associated with the recurrence of appendicitis.
Conclusions
The presence of an appendicolith or abscess was not a crucial factor for surgery. Incarceration of an appendicolith and periappendiceal fluid on CT images was predictive factors for the failure of NOM.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The nonoperative management (NOM) of patients with appendicitis has been widely accepted [1]. Several meta-analyses have revealed the safety and feasibility of NOM for patients with uncomplicated appendicitis [2,3,4,5,6,7,8]. Furthermore, even in patients with complicated appendicitis, the superiority of NOM was demonstrated in terms of a lower incidence of complications [9,10,11,12].
The incidence for failure of NOM in patients with uncomplicated appendicitis was reported to be 10% or less; on the other hand, the incidence for failure of NOM in patients with complicated appendicitis was reported to be higher [4, 5, 10]. Previously, several retrospective studies suggested predictive factors for failure of NOM [13,14,15,16,17,18]. However, there have not been apparent criteria that imply a patients’ crucial risk for failure of NOM. Predicting patients who fail in NOM yields a well-considered strategy for patients with acute appendicitis. Herein, we retrospectively reviewed patients who underwent NOM, investigated predictive factors for failure of NOM, and evaluated the feasibility of NOM, especially in patients with abscesses.
Materials and methods
Study patients
A total of 196 patients with acute appendicitis underwent NOM between April 2014 and December 2020 at Fujinomiya City General Hospital. Of these 196 patients, 24 patients failed NOM and required emergency surgery (failure group: n = 24), while the other 172 patients were successfully treated and discharged after NOM (success group: n = 172). These two groups were compared, and the risk factors for failure of NOM were investigated. In addition, 32 patients with abscesses (abscess group: n = 32) were compared with 164 patients without abscesses (nonabscess group: n = 164).
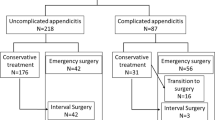
In the success group, 28 patients underwent interval appendectomy after NOM. In the other 144 patients, 31 patients developed a recurrence of appendicitis during the study period (recurrence group: n = 31), and the other 113 patients did not develop a recurrence of appendicitis (nonrecurrence group: n = 113). In a subgroup analysis, comparisons were performed between these two groups (Fig. 1).
The study protocol was approved by the Institutional Review Board of Fujinomiya City General Hospital. Informed consent was waived for this retrospective study.
Strategy of NOM and definition of failure
In this study, all included patients were diagnosed with acute appendicitis according to CT images, and enhanced CT was generally performed unless the patient had a contraindication, such as an allergy to contrast agents or impaired renal function. In this study, 34 patients performed CT examination without contrast. When patients were diagnosed with acute appendicitis, they were assigned to surgery or NOM. Although the selection of treatment was generally decided according to each patient’s discretion, emergency surgeries were performed in cases with severe abdominal pain or generalized peritonitis.
The selection of antibiotics was made at the discretion of surgeons, taking the patient’s condition into consideration. An antibiotic, cefmetazole (2 ~ 4 g/day), tazobactam piperacillin (13.5 g/day), cefepime (2 g/day), or meropenem (1.5 g/day), was generally administered until the symptoms and inflammatory response subsided. If the effect was insufficient, the antimicrobial agent was exchanged for another agent.
Failure of NOM was determined if the patient was converted to undergo surgery before the resolution of symptoms associated with appendicitis.
Clinical variables assessed
We reviewed the following clinical variables: sex, age, history of appendicitis, presence of comorbidities, and WBC and C-reactive protein (CRP) levels at diagnosis, and time from onset to diagnosis, antimicrobial agents, and length of stay were reviewed.
Imaging parameters assessed
Among the 196 patients included in the study, all patients were examined by abdominal MDCT using Light Speed VCT (GE Healthcare, Tokyo, Japan) until January 2017 and SOMATOM Force (Siemens Healthineers AG, Erlangen, Federal republic of Germany) after February 2017. As CT findings, presence of appendicolith, incarceration of appendicolith (dilation of peripheral side of appendix) (Fig. 2), periappendiceal fluid (Fig. 3), and abscess were reviewed.
Two experienced reviewers (a gastroenterological surgeon with 15 years of experience and a radiologist with 20 years of experience) retrospectively reviewed the imaging parameters. Measurements were performed in consensus, and both readers were blinded to the outcome at the time of performing the measurements.
Statistical analyses
Study variables are shown as the number and percentage of patients, percentage of patients, or mean values. Between-group differences in nominal variables were analyzed by Pearson’s chi-square test, and differences in continuous variables were analyzed by the Mann–Whitney U test. Multivariable logistic regression analysis was performed to determine independent predictors of outcomes. All statistical analyses were performed with the Statistical Package for the Social Sciences, version 11.5 J for Windows 10 (SPSS, Chicago, IL, USA). A p value < 0.05 was considered significant.
Results
Comparison between the failure group and success group (Table 1)
The male to female ratio and age were not different between the groups. The presence of comorbidities, including diabetes mellitus, chronic renal failure, and coronary heart disease/chronic heart failure, was not different between the groups. The number of patients with a previous history of stroke was significantly increased in the failure group (12.5% vs. 2.9%, p = 0.026). The WBC and CRP levels at diagnosis and the time from onset to diagnosis were not different. Regarding CT findings, the presence of an appendicolith was not different. On the other hand, the incarceration of an appendicolith was significantly increased in the failure group (20.8% vs. 1.7%, p < 0.001). The presence of periappendiceal fluid was significantly increased in the failure group (50.0% vs. 26.7%, p = 0.019). The presence of abscess was not different.
In the success group, seven of the 20 patients who showed an appendicolith at diagnosis were confirmed to have the disappearance of said appendicolith on follow-up CT images performed during the study period (not shown in table).
Factors predicting failure of NOM (Table 2)
Incarceration of an appendicolith (p < 0.001, odds ratio = 19.85) and periappendiceal fluid (p = 0.009, odds ratio = 3.62) were found by logistic regression analysis to be independent predictors for failure of NOM.
Comparison between the abscess group and the nonabscess group (Table 3)
The male to female ratio was not different. Age was significantly higher in the abscess group (p < 0.001). The presence of chronic renal failure was significantly increased in the abscess group (6.2% vs. 0.6%, p = 0.017). The presence of stroke was significantly increased in the abscess group (12.5% vs. 2.4%, p = 0.008). The WBC level at diagnosis was not different, while the CRP level at diagnosis was significantly higher in the abscess group (p < 0.001). The time from onset to diagnosis was significantly longer in the abscess group (p < 0.001). Regarding treatment, broad-spectrum antibiotics were significantly used in the abscess group (84.3% vs. 20.1%, p < 0.001). Two or more different antibiotics were significantly used in the abscess group (31.2% vs. 10.9%, p = 0.002). The length of hospital stay was significantly longer in the abscess group (p < 0.001). In the abscess group, three patients underwent percutaneous abscess drainage, and all three patients successfully underwent NOM (not shown in Table).
Subgroup analysis: comparison between the recurrence group and the nonrecurrence group (Table 4)
The male to female ratio and mean age were not different between the groups. The number of patients with a previous history of appendicitis was significantly increased in the recurrence group (19.3% vs. 7.0%, p = 0.041). The presence of comorbidities, including diabetes mellitus, chronic renal failure, coronary heart disease/chronic heart failure, and stroke, was not different between the groups. The mean WBC and CRP levels at diagnosis were not different. The time from onset to diagnosis was not different. Regarding CT findings, the presence of an appendicolith (9.6% vs. 12.3%), incarceration of an appendicolith (0% vs. 2.6%), presence of periappendiceal fluid (19.3 vs. 25.6%), and presence of an abscess (12.9% vs. 14.1%) were not significantly different.
Discussion
Our study revealed that incarceration of an appendicolith and periappendiceal fluid on CT images were independent predictors for failure of NOM, while neither the presence of an appendicolith nor abscess were predictors. In addition, our study also revealed that a previous history of appendicitis was associated with recurrence, while neither the presence of an appendicolith nor abscess was associated with recurrence.
Previous reports suggested some predictive factors for failure of NOM [13,14,15,16,17,18]. Several studies suggested that the presence of an appendicolith is one of the predictive factors for failure of NOM, especially in pediatric patients [5, 13,14,15]. In addition, a recent randomized trial that included 1552 adult patients demonstrated that the presence of an appendicolith is associated with worse outcomes in patients with appendicitis [19]. However, these studies did not distinguish patients with incarceration of an appendicolith from those without incarceration. Our study demonstrated that incarceration of an appendicolith was one of the independent predictors for failure of NOM, while the presence of an appendicolith was not associated with failure of NOM. Ishiyama et al. suggested that an appendicolith greater than 5 mm and an appendicolith at the root of the appendix on CT images are exacerbating factors for acute appendicitis [20]. Our study advocates that surgeons stratify patients with appendicoliths at risk for failure of NOM, depending on whether the appendicolith is incarcerated.
In patients with an abscess or phlegmon, operative management is often challenging, resulting in a higher incidence of intestinal injury or the requirement for extended surgery [21]. Previous meta-analyses revealed that, in patients with an abscess or phlegmon, NOM yields a lower incidence of complications compared to that in operative management [9,10,11,12]. In our study, the presence of an abscess was associated with a relatively high failure ratio (29.1%) and required a significantly longer hospital stay and two or more different antibiotics; on the other hand, it was not associated with recurrence during the study period. A previous study also suggested the unnecessity for routine interval appendectomy in patients with appendiceal masses after NOM due to a lower recurrence rate [22]. However, a recent study reported that, especially in patients older than 40 years old, patients with abscesses showed a high rate (20%) of neoplasms [23]. Therefore, surgeons have to keep it in mind that NOM for patients with abscesses implies a risk of overlooking appendiceal neoplasms, and patients with abscesses require close observation after NOM.
To our knowledge, predictive factors for recurrence after NOM have not been investigated in detail. Our study suggested that a previous history of appendicitis was significantly associated with recurrence. It is worth noting that, in our study, neither the presence of an appendicolith nor abscess was associated with recurrence. In addition, at least seven of 20 patients with appendicoliths showed disappearance of said appendicolith after NOM during the study period. This phenomenon also supported the presence of an appendicolith is not a contraindication to NOM.
There were some limitations associated with this study. First, the present study was retrospective in nature and was performed at a single center with relatively small sample size. Second, as an entrance bias, the choice of procedure, namely, operation or NOM, was at the patient’s discretion, and patients who had severe pain or generalized peritonitis were usually allocated to an operation and excluded from this study. In addition, the selection of antimicrobial agents was decided according to the surgeon’s discretion. Therefore, strong biases that affect the objectivity of the final statistical results might be present. Third, the number of patients with an appendicolith or abscess was small in our study. Furthermore, two readers obtained CT findings via a consensus read. It was desirable to perform measurement by several readers independently. Further study is needed to validate our results.
Data availability
Not applicable.
Code availability
Not applicable.
References
Di Saverio S, Podda M, De Simone B et al (2020) Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg 15:27. https://doi.org/10.1186/s13017-020-00306-3
Sallinen V, Akl EA, You JJ et al (2016) Meta-analysis of antibiotics versus appendicectomy for nonperforated acute appendicitis. Br J Surg 103:656–667. https://doi.org/10.1002/bjs.10147
Harnoss JC, Zelienka I, Probst P et al (2017) Antibiotics versus surgical therapy for uncomplicated appendicitis: systematic review and meta-analysis of controlled trials (PROSPERO 2015: CRD42015016882). Ann Surg 265:889–900. https://doi.org/10.1097/SLA.0000000000002039
Podda M, Gerardi C, Cillara N et al (2019) Antibiotic treatment and appendectomy for uncomplicated acute appendicitis in adults and children: a systematic review and meta-analysis. Ann Surg 270:1028–1040. https://doi.org/10.1097/SLA.0000000000003225
Huang L, Yin Y, Yang L, Wang C, Li Y, Zhou Z (2017) Comparison of antibiotic therapy and appendectomy for acute uncomplicated appendicitis in children: a meta-analysis. JAMA Pediatr 171:426–434. https://doi.org/10.1001/jamapediatrics.2017.0057
Gorter RR, The SML, Gorter-Stam MAW et al (2017) Systematic review of nonoperative versus operative treatment of uncomplicated appendicitis. J Pediatr Surg 52:1219–1227. https://doi.org/10.1016/j.jpedsurg.2017.04.005
Georgiou R, Eaton S, Stanton MP, Pierro A, Hall NJ (2017) Efficacy and safety of nonoperative treatment for acute appendicitis: a meta-analysis. Pediatrics 139:e20163003. https://doi.org/10.1542/peds.2016-3003
Maita S, Andersson B, Svensson JF, Wester T (2020) Nonoperative treatment for nonperforated appendicitis in children: a systematic review and meta-analysis. Pediatr Surg Int 36:261–269. https://doi.org/10.1007/s00383-019-04610-1
Simillis C, Symeonides P, Shorthouse AJ, Tekkis PP (2010) A meta-analysis comparing conservative treatment versus acute appendectomy for complicated appendicitis (abscess or phlegmon). Surgery 147:818–829. https://doi.org/10.1016/j.surg.2009.11.013
Yang Z, Sun F, Ai S, Wang J, Guan W, Liu S (2019) Meta-analysis of studies comparing conservative treatment with antibiotics and appendectomy for acute appendicitis in the adult. BMC Surg 19:110. https://doi.org/10.1186/s12893-019-0578-5
Fugazzola P, Coccolini F, Tomasoni M, Stella M, Ansaloni L (2019) Early appendectomy vs. conservative management in complicated acute appendicitis in children: a meta-analysis. J Pediatr Surg 54:2234–2241. https://doi.org/10.1016/j.jpedsurg.2019.01.065
van Amstel P, Sluckin TC, van Amstel T et al (2020) Management of appendiceal mass and abscess in children; early appendectomy or initial nonoperative treatment? A systematic review and meta-analysis. Surg Endosc 34:5234–5249. https://doi.org/10.1007/s00464-020-07822-y
Aprahamian CJ, Barnhart DC, Bledsoe SE, Vaid Y, Harmon CM (2007) Failure in the nonoperative management of pediatric ruptured appendicitis: predictors and consequences. J Pediatr Surg 42:934–8. https://doi.org/10.1016/j.jpedsurg.2007.01.024 (discussion 938)
Mahida JB, Lodwick DL, Nacion KM et al (2016) High failure rate of nonoperative management of acute appendicitis with an appendicolith in children. J Pediatr Surg 51:908–911. https://doi.org/10.1016/j.jpedsurg.2016.02.056
Fuhrer AE, Sukhotnik I, Ben-Shahar Y, Weinberg M, Koppelmann T (2021) Predictive value of Alvarado score and pediatric appendicitis score in the success of nonoperative management for simple acute appendicitis in children. Eur J Pediatr Surg 31:95–101. https://doi.org/10.1055/s-0040-1718406
Talishinskiy T, Limberg J, Ginsburg H, Kuenzler K, Fisher J, Tomita S (2016) Factors associated with failure of nonoperative treatment of complicated appendicitis in children. J Pediatr Surg 51:1174–1176. https://doi.org/10.1016/j.jpedsurg.2016.01.006
Maxfield MW, Schuster KM, Bokhari J, McGillicuddy EA, Davis KA (2014) Predictive factors for failure of nonoperative management in perforated appendicitis. J Trauma Acute Care Surg 76:976–981. https://doi.org/10.1097/TA.0000000000000187
Walker C, Moosavi A, Young K et al (2019) Factors associated with failure of nonoperative management for complicated appendicitis. Am Surg 85:865–870
Collaborative CODA, Flum DR, Davidson GH et al (2020) A randomized trial comparing antibiotics with appendectomy for appendicitis. N Engl J Med 383:1907–1919. https://doi.org/10.1056/NEJMoa2014320
Ishiyama M, Yanase F, Taketa T et al (2013) Significance of size and location of appendicoliths as exacerbating factor of acute appendicitis. Emerg Radiol 20:125–130. https://doi.org/10.1007/s10140-012-1093-5
Shekarriz S, Keck T, Kujath P et al (2019) Comparison of conservative versus surgical therapy for acute appendicitis with abscess in five German hospitals. Int J Colorectal Dis 34:649–655. https://doi.org/10.1007/s00384-019-03238-w
Tekin A, Kurtoğlu HC, Can I, Oztan S (2008) Routine interval appendectomy is unnecessary after conservative treatment of appendiceal mass. Colorectal Dis 10:465–468. https://doi.org/10.1111/j.1463-1318.2007.01377.x
Mällinen J, Rautio T, Grönroos J et al (2019) Risk of appendiceal neoplasm in periappendicular abscess in patients treated with interval appendectomy vs follow-up with magnetic resonance imaging: 1-year outcomes of the peri-appendicitis acuta randomized clinical trial. JAMA Surg 154:200–207. https://doi.org/10.1001/jamasurg.2018.4373
Author information
Authors and Affiliations
Contributions
A.K. wrote the manuscript and performed data analysis. All authors contributed to acquire data and revise the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kohga, A., Kawabe, A., Yajima, K. et al. Does the presence of an appendicolith or abscess predict failure of nonoperative management of patients with acute appendicitis?. Emerg Radiol 28, 977–983 (2021). https://doi.org/10.1007/s10140-021-01951-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-021-01951-0