Abstract
Purpose
To describe the first “arcuate sign” case series in the pediatric population, radiologic features of the associated injuries, management, and how they compare with the adult population.
Methods
Retrospective study included patients under 18 years of age with a classic “arcuate sign” on radiographs. Data collected included patient demographics, mechanism of injury, and management. Radiographs and advanced imaging (MRI, CT) were reviewed by two musculoskeletal radiologists in a blinded fashion and findings recorded.
Results
Seven patients (4 males, 3 females) with mean age 15 years (range 14–17 years) were included in the study. All 7 injuries were related to sports, 5/7 (71%) being non-contact injuries. Five patients had MRI done-1 LCL injury, MPFL sprain, and MCL sprain were reported; 3 popliteofibular ligament and popliteus sprains were seen; and 3 bone contusions were present on imaging. None of the patients had meniscus or cruciate ligament tears. One patient had an additional fracture of the lateral tibial plateau at the ilio-tibial band attachment and an associated peroneal nerve injury. Five out of seven (71.4%) were treated non-operatively and were able to return back to activity at a mean of 7.2 weeks from injury. Two out of seven (28.6%) needed operative intervention for the fracture but not arthroscopic repair.
Conclusion
Pediatric patients with a radiographic arcuate sign tend not to have ACL, PCL, or meniscal injuries, and treatment is predominantly non-operative in contrast to literature reported in adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
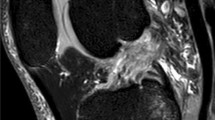
The “arcuate sign” refers to an avulsion fracture of the head of fibula seen on knee radiographs and is considered to have high association with posterolateral corner injuries of the knee (Fig. 1) [1, 2]. This avulsed bony fragment is related to the insertion site of the arcuate complex [1, 3,4,5]. The injury has been postulated to occur via two mechanisms, either varus force with the tibia externally rotated or knee hyperextension with the tibia internally rotated. There are only a few case series of this injury reported in adult literature which show a high association with posterior cruciate ligament tear and posterolateral corner ligament disruption, and no studies to our knowledge have been conducted in the pediatric population [6,7,8]. There is reason to believe that in children, who have different relative strengths of ligaments compared with their bones, the arcuate sign might not necessarily have a high association with posterolateral corner ligamentous injuries as it is in adults [9]. The purpose of our study is to describe the first case series of this injury in the pediatric and adolescent population and elaborate on the radiologic features of the associated injuries and their management. We also aim to determine how these features in pediatric patients compare with the current literature in the adult population.
Materials and methods
This IRB-approved, retrospective study included patients under 18 years at a tertiary children’s hospital with an “arcuate sign,” i.e., avulsion fracture of fibular head on radiologic imaging from 2005 to 2020. A search of all radiographs in our institution’s PACS (picture archiving and communication system) between January 2005 and April 2020 was performed using the keywords “arcuate sign,” “arcuate fracture,” and “fibular head fracture.” Patients with non-avulsive fibular head fractures that did not fit the definition of an arcuate fracture were excluded. Data collected from the chart review of these patients included demographics, age, gender, mechanism of injury and associated sport, time of presentation from injury, treatment, and return back to previous activity. Radiologic imaging, consisting of conventional radiographs and advanced imaging in the form of magnetic resonance imaging (MRI) and computerized tomography (CT) scans, was independently assessed by two fellowship-trained pediatric musculoskeletal radiologists with 12 years (S.P.J) and 1 year (M.G.D) post-fellowship experience. Differences were sorted by consensus review. The radiologists were blinded to patient management. All MRIs performed at our institution were obtained on either a 1.5- or 3-Tesla magnet with our routine knee protocol consisting of a sagittal proton density–weighted sequence without fat saturation, coronal and axial proton density–weighted sequences with fat saturation, and a sagittal T2–weighted sequence with fat saturation (Table 1). The presence of any meniscal, ligamentous, or popliteus injury was documented. Descriptive statistical analysis was completed and summarized as means with range values or frequencies with corresponding percentages. This was compared with current literature on arcuate sign in adults and associated findings.
Results
Seven patients (4 males, 3 females) with mean age 15 years (range 14–17 years) were included in the study (Table 2). The patients had an average height of 168 cm (range 154.7–178 cm), average weight of 73.6 kg (range 44.5–116.5 kg), average BMI of 22.0 (range 18.6–24.9), and average BMI percentile of 69.4% (range 36.7–91.5). The laterality of the injuries involved 4 right knees and 3 left knees; the majority of the patients (6/7) presented to the hospital within a week of the injury. All 7 injuries were related to sports; American football was implicated sport in 2/7(29%) and 5/7 (71%) being non-contact injuries (Table 2). The mean width of the avulsed fibula fragment was 2.3 mm (range 1–6 mm, median 1.6 mm).
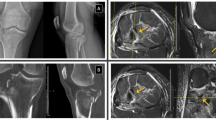
Of the 7 patients who were diagnosed with standard radiographs, 5 patients had MRI done for further characterization of associated injuries; the other 2 did not get advanced imaging as it was not felt necessary by the physician based on stability of the ligaments on clinical examination. One out of five patients had an LCL injury, MPFL sprain, and MCL sprain, 3/5 had mild strains of the popliteus and sprains of the popliteofibular ligament, and 3/5 had bone contusions. None of the patients had meniscal or cruciate ligament tears (Table 3). One patient additionally had a displaced avulsion fracture of the lateral tibial plateau at the ilio-tibial band attachment with an associated peroneal nerve injury as defined by foot drop on clinical examination. Five out of seven patients (71.4%) were treated non-operatively with RICE (rest, ice, compression, elevation), bracing, NSAIDs (non-steroidal anti-inflammatory drugs), and physical therapy and were able to return to their baseline level of activity at a mean of 7.2 weeks from injury. Only 2/7 patients (28.6%) needed operative intervention (Table 3): one had open reduction and internal fixation (ORIF) of the proximal fibular fracture with neurolysis of the common peroneal nerve and the second patient with foot drop and underwent a peroneal nerve neurolysis and sural nerve grafting without fracture fixation.
Discussion
Avulsion fractures of the proximal fibula can occur during isolated knee injuries or as a part of complex knee trauma. Plain radiograph evaluation may demonstrate a fleck of bone superiorly displaced from the fibula, which is also called the “arcuate sign”[1, 6, 8, 10, 11]. The “arcuate” sign is used to describe an avulsed bone fragment related to the insertion site of the arcuate complex, which consists of the fabello-fibular, popliteofibular, and arcuate ligaments [5, 7, 8, 12].
The mechanism of this injury, which leads to posterolateral instability, is most commonly a direct blow against the anteromedial tibia with the knee in extension [7]; this is most commonly described in association with motor vehicle accidents, high velocity trauma, high impact sports injuries, and knee dislocations in obese individuals in the adult population [13,14,15]. However, sports injuries, particularly in association with American football, are commonly implicated in the pediatric population[16] as seen in our patient series.
Recognizing posterolateral knee instability is very important clinically as it is well known that unrecognized and untreated posterolateral instability may result in a failure of reconstruction of either the anterior or posterior cruciate ligaments [14, 15]. Hence, identifying the presence of an avulsion fracture of the fibular head and recognizing any associated injuries are of great clinical importance [3, 7, 17].
MRI is the imaging modality of choice and potentially demonstrates the entire spectrum of posterolateral corner injuries and associated lesions of the knee, including those that may be overlooked during clinical examination or arthroscopy [4, 18]. To determine the diagnostic performance of MRI for helping to predict posterolateral knee instability in patients with acute anterior cruciate ligament (ACL) tear, Filli et al. [19] found that a complete tear or avulsion of the LCL was the most significant predictor of posterolateral instability and the assessment of the smaller posterolateral corner structures did not improve diagnostic performance. Practically, all tears of LCL are associated with damage to posterolateral knee structures. Most injuries of the popliteus muscle and tendon are associated with damage to other knee structures [3].
In children or adolescents with open growth plates, the posterolateral corner injury pattern is considered more rare than in adults. Because knee ligaments are felt to be stronger than the adjacent physeal plates, the energy of pathologic translational and rotatory stress commonly results in a fracture or avulsion injury rather than a ligamentous injury [20]. This was confirmed in our case series with only 1 patient showing a mild sprain of the LCL. One patient had medial collateral and medial patellofemoral ligament sprains. Three patients had mild sprains of the popliteofibular ligament and mild popliteus strain. None of our patients had a complete tear of a PLC structure. Also, unlike some adult case reports [6], our case series had no associated ACL tear.
Pediatric studies on isolated posterolateral corner injuries are very rare and primarily case reports [21]. In a study on collateral ligament injuries in the pediatric population, Kramer et al. [16] found that 22% of patients had LCL injuries, of which 6% had concurrent posterolateral corner injuries. Forty-two (82%) knees had injuries that occurred during sports which is similar to our patient series. Previous arcuate sign case series in adults (Table 3) suggest a much higher incidence of severe associated ligament injuries. For example, injury of the posterior cruciate ligament was seen in 100% of adult patients in 2 case series [6, 7] and 66.7% in another [22]. This is in contrast to our pediatric case series which did not show any cruciate ligament tears (Table 3). In young patients without any major ligamentous injuries, a non-operative management is the treatment of choice which includes weight bearing as tolerated and rehabilitation [23]. Based on this, we would recommend getting an MRI only if indicated based on clinical findings.
One of our patients had another proximal tibia fracture along with a PLC injury. This has been described in adults as an often missed, unusual injury pattern that consists of a large anteromedial tibial plateau fracture associated with a posterolateral (PL) knee corner injury sparing injury to the cruciate ligaments [24].
The appropriate treatment for either injury (posterolateral corner or posterior cruciate ligament) remains controversial in the skeletally immature patient [20]. The literature on non-operative treatment of low-grade injuries is sparse. Good results have been reported for non-surgical treatment for low-grade injuries [13, 23], which was the case in the majority of our patients who were treated non-operatively (5/7). This is in contrast to adult case series on arcuate fractures, which have a high incidence of operative intervention ranging from 66% [22] to sometimes up to 100% of patients [7]. The mean time for return to sports in a pediatric collateral ligament case series was 2.2 months [16], which is similar to our patient series.
Limitations of our study include a small cohort of patients precluding us from conducting inferential statistical analysis as it would be underpowered. However, it is still the largest case series in the pediatric population, which renders the descriptive analysis meaningful. Multicenter studies with larger patient populations could possibly be done in the future.
Conclusion
Pediatric patients presenting with a radiographic “arcuate sign” tend to have low-grade injuries to the posterolateral corner structures with low frequency of meniscal or cruciate ligament injuries. Treatment is predominantly non-operative in contrast to literature reported in adults.
References
Shindell R, Walsh WM, Connolly JF (1984) Avulsion fracture of the fibula: the ‘arcuate sign’ of posterolateral knee instability. Nebr Med J 69(11):369–371
Strub WM (2007) The arcuate sign. Radiology 244(2):620–621. https://doi.org/10.1148/radiol.2442042160
Recondo JA, Salvador E, Villanúa JA, Barrera MC, Gervás C, Alústiza JM (2000) Lateral stabilizing structures of the knee: functional anatomy and injuries assessed with MR imaging. Radiographics 20 Spec No:S91–S102. https://doi.org/10.1148/radiographics.20.suppl_1.g00oc02s91
Bolog N, Hodler J (2007) MR imaging of the posterolateral corner of the knee. Skelet Radiol 36(8):715–728. https://doi.org/10.1007/s00256-006-0271-5
Jadhav SP, More SR, Riascos RF, Lemos DF, Swischuk LE (2014) Comprehensive review of the anatomy, function, and imaging of the popliteus and associated pathologic conditions. Radiographics 34(2):496–513. https://doi.org/10.1148/rg.342125082
Crimmins JT, Wissman RD (2008) The arcuate sign: a marker of potential knee dislocation? A report of two cases. Radiol Case Rep 3(2):160. https://doi.org/10.2484/rcr.v3i2.160
Huang GS, Yu JS, Munshi M, Chan WP, Lee CH, Chen CY, Resnick D (2003) Avulsion fracture of the head of the fibula (the “arcuate” sign): MR imaging findings predictive of injuries to the posterolateral ligaments and posterior cruciate ligament. AJR Am J Roentgenol 180(2):381–387. https://doi.org/10.2214/ajr.180.2.1800381
Lee J, Papakonstantinou O, Brookenthal KR, Trudell D, Resnick DL (2003) Arcuate sign of posterolateral knee injuries: anatomic, radiographic, and MR imaging data related to patterns of injury. Skelet Radiol 32(11):619–627. https://doi.org/10.1007/s00256-003-0679-0
Dwek JR (2016) A structural and mechanism-based perspective toward understanding pediatric and adult sports injuries. AJR Am J Roentgenol 206(5):980–986. https://doi.org/10.2214/ajr.15.15937
Cohen BH, DeFroda SF, Hodax JD, Johnson D, Kristopher Ware J, Fadale PD (2018) The arcuate fracture: a descriptive radiographic study. Injury 49(10):1871–1877. https://doi.org/10.1016/j.injury.2018.08.009
Markeson CD, Renacci RM, Bartolotta RJ (2020) Arcuate sign in posterolateral corner injury of the knee. J Emerg Med 58:509–511. https://doi.org/10.1016/j.jemermed.2019.11.035
Takahashi H, Tajima G, Kikuchi S, Yan J, Kamei Y, Maruyama M, Sugawara A, Saigo T, Doita M (2017) Morphology of the fibular insertion of the posterolateral corner and biceps femoris tendon. Knee Surg Sports Traumatol Arthrosc 25(1):184–191. https://doi.org/10.1007/s00167-016-4304-x
Chahla J, Moatshe G, Dean CS, LaPrade RF (2016) Posterolateral corner of the knee: current concepts. Arch Bone Jt Surg 4(2):97–103
Dold AP, Swensen S, Strauss E, Alaia M (2017) The posteromedial corner of the knee: anatomy, pathology, and management strategies. J Am Acad Orthop Surg 25(11):752–761. https://doi.org/10.5435/jaaos-d-16-00020
Hughes JD, Rauer T, Gibbs CM, Musahl V (2019) Diagnosis and treatment of rotatory knee instability. J Exp Orthop 6(1):48. https://doi.org/10.1186/s40634-019-0217-1
Kramer DE, Miller PE, Berrahou IK, Yen YM, Heyworth BE (2017) Collateral ligament knee injuries in pediatric and adolescent athletes. J Pediatr Orthop 40:71–77. https://doi.org/10.1097/bpo.0000000000001112
de Alencar Neto JB, de Souza CJD, Lopes MBG, Cavalcante MLC, Neto LHP (2020) Bilateral avulsion fracture of the fibula head of the knee associated with avulsion fracture of the iliotibial band: a rare case of fracture Segond associated with arcuate fracture. Case Rep Orthop 2020:8825638–8825638. https://doi.org/10.1155/2020/8825638
Vasilevska Nikodinovska V, Gimber LH, Hardy JC, Taljanovic MS (2016) The collateral ligaments and posterolateral corner: what radiologists should know. Semin Musculoskelet Radiol 20(1):52–64. https://doi.org/10.1055/s-0036-1579677
Filli L, Rosskopf AB, Sutter R, Fucentese SF, Pfirrmann CWA (2018) MRI predictors of posterolateral corner instability: a decision tree analysis of patients with acute anterior cruciate ligament tear. Radiology 289(1):170–180. https://doi.org/10.1148/radiol.2018180194
Mascarenhas R, Bonci G, Bowman KF, Forsythe B, Harner CD (2013) Combined ACL-posterolateral corner injury in a skeletally immature athlete. J Knee Surg 26(Suppl 1):S94–S99. https://doi.org/10.1055/s-0032-1322597
von Heideken J, Mikkelsson C, Boström Windhamre H, Janarv PM (2011) Acute injuries to the posterolateral corner of the knee in children: a case series of 6 patients. Am J Sports Med 39(10):2199–2205. https://doi.org/10.1177/0363546511416198
Juhng SK, Lee JK, Choi SS, Yoon KH, Roh BS, Won JJ (2002) MR evaluation of the “arcuate” sign of posterolateral knee instability. AJR Am J Roentgenol 178(3):583–588. https://doi.org/10.2214/ajr.178.3.1780583
Spadafore S, Khodaee M (2020) Avulsion fracture of the proximal fibula (arcuate sign) in a young woman. BMJ Case Rep 13(9):e237368. https://doi.org/10.1136/bcr-2020-237368
Tomás-Hernández J, Monyart JM, Serra JT, Vinaixa MR, Farfan EG, García VM, Feliu EC (2016) Large fracture of the anteromedial tibial plateau with isolated posterolateral knee corner injury: case series of an often missed unusual injury pattern. Injury 47(Suppl 3):S35–S40. https://doi.org/10.1016/s0020-1383(16)30604-0
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kushare, I., Ghanta, R.B., Ditzler, M. et al. Arcuate sign—fibular head avulsion fracture and associated injuries in the pediatric and adolescent population. Emerg Radiol 28, 723–727 (2021). https://doi.org/10.1007/s10140-021-01910-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-021-01910-9