Abstract
The purpose of this study was twofold: (1) to determine the incidence of positive computed tomography (CT) findings in patients presenting to the emergency department (ED) with non-traumatic headache at our institution and (2) to examine follow-up exams, including lumbar puncture, non-enhanced CT, CT angiogram, CT venogram, and magnetic resonance imaging (MRI), to see how often the use of further testing changes the diagnosis. With IRB approval, 865 patients were identified through ED requisitions for CT head with the indication of headache during the calendar year 2011. Exclusion criteria included head trauma, prior intracranial surgery, focal neurologic symptoms, and known intracranial mass. CT results were divided into three categories: P0, P1, and P2. Negative studies were graded as P0. Positive studies were subdivided into clinically insignificant or P1 and clinically significant or P2. Clinically significant was defined as requiring medical treatment. Subsequently, the electronic medical records and picture archiving and communication system (PACS) were reviewed to determine the incidence of follow-up exams, including lumbar puncture or imaging. The secondary tests were divided into the same P0, P1, and P2 categories. There were 254 positive studies: P1 clinically insignificant (27.1 %, 235/865) and P2 clinically significant (2.2 %, 19/865). Of 257 follow-up exams performed, the majority were lumbar punctures (36.0 %) or CT angiograms (29.5 %). In 19/257 exams or 7.4 %, the additional testing changed the clinically insignificant (P0/P1) diagnosis to a significant (P2) result. At our institution, there was a 2.2 % incidence of significant positive CT findings in patients presenting to the ED with non-traumatic headache. Follow-up testing was variable and resulted in a 7.4 % increase in the severity of diagnosis compared to the initial negative CT scan.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Headache is a common complaint with many potential etiologies. Global prevalence of headache disorder in general has been estimated to be 47 % in the general population with chronic daily headache occurring in 3 % [1]. Headaches lead to innumerable visits to clinics and emergency rooms around the world. In the setting of non-traumatic headache as an isolated symptom, with no focal neurologic deficits, most patients can be managed safely without radiologic imaging [2]. Multiple previous studies have demonstrated that computed tomography (CT) and magnetic resonance imaging (MRI) evaluation in this patient population is of extremely low yield [2–5]. Unfortunately, emergency physicians often face intense pressure from patients and often feel compelled to obtain imaging, even in those who could be treated conservatively [2].
CT utilization for non-traumatic headache in US emergency departments trended upwards from 1998 to 2008 with a concurrent decrease in the prevalence of intracranial pathology (ICP) [6]. Some have advocated for specific clinical decision rules for determining who should receive neuroimaging for acute headache, especially when the differential includes subarachnoid hemorrhage [7]. Others have suggested using clinical risk factors to stratify patients’ overall risk for actionable CT results [8] or using online clinical decision support tools to ensure that only those patients who meet certain criteria will receive appropriate use of resources [9]. While CT assessment is an important tool in assessing cranial pathology in the emergency department (ED), appropriateness criteria should be utilized to ensure that the potential benefits outweigh the harms [10]. Advanced imaging remains relatively expensive. Many of the older studies focusing on effectiveness of CT are more than 10 years old [3, 11–13].
The purpose of our study was twofold. Firstly, we sought to examine the incidence of positive findings of non-enhanced CT head scans at our institution for those patients presenting to the emergency department with non-traumatic headache. Secondly, we sought to evaluate how many patients went onto follow-up testing, such as a second CT scan, CT angiography (CTA), MRI, or lumbar puncture (LP) and to determine if those results altered the initial diagnosis. To our knowledge, no other studies have looked specifically at this patient population and how follow-up testing may or may not change the initial diagnosis at non-enhanced CT.
Methods
ED imaging requisitions for non-enhanced CT head were reviewed over a 1-year period (January 1 to December 31, 2011) at our institution, a tertiary care academic hospital. Patients with requisition indications including the word headache were recorded. The ED consultations for each encounter were reviewed for additional clinical history. Exclusion criteria included head trauma, prior intracranial surgery, and known brain tumor or metastasis. Patients with additional symptoms (including focal weakness, numbness, paresthesias, visual symptoms, vertigo, fever) were also excluded.
CT head results were divided into three categories: P0, P1, and P2. Negative (normal) studies were graded as P0. Positive studies were subdivided into clinically insignificant or P1 and clinically significant or P2. Clinically significant results were defined as those that required immediate change in medical management. Fellowship-trained neuroradiologists reported all exams.
Subsequently, the electronic medical records and picture archiving and communication system (PACS) were used to see if patients went on for follow-up testing (within a 2-year window following the initial CT), including lumbar puncture or further imaging. The secondary tests were then divided into the same P0, P1, and P2 categories. For those who received follow-up testing, the initial exam result (P0, P1, or P2) was compared to the subsequent result to see if the second test changed the diagnosis from a clinically insignificant finding (P0, P1) to a clinically significant finding (P2).
Results
Upon review of the imaging requisitions, there were 1098 patients who were categorized with headache only (HA only) and 876 patients who were excluded as they had headache with other symptoms or a history of trauma. Emergency department consultations were reviewed to determine if additional symptoms were recorded, but not included on the imaging requisition. This resulted in 213 additional patients being excluded. After excluding patients and removing multiple visits of those who presented to the ED more than once, there were 865 patients remaining.
Women constituted 64.7 % of patients, while men constituted 35.3 %. The age range was 15 to 95 years, a mean of 47.6 years. Seven pediatric patients (<18 years) were included. Demographic features of the sample group are summarized in Table 1.
In the sample group, there were 612 P0-negative results (70.8 %), 234 P1 results (27.1 %), and 19 P2 results (2.2 %) (Fig. 1). Overall, there were 254 positive studies out of 865 patients, classified as either P1 or P2. The majority of results were in the P1 category (92.1 %, 234/254). The most common P1 results included microvascular changes/remote infarcts/encephalomalacia (45.5 %, n = 107) and paranasal sinus changes (37.9 %, n = 89). Uncommon P1 findings included volume loss/atrophy (5.1 %, n = 12), low-lying tonsils (3.0 %, n = 7), meningioma (1.7 %, n = 4), cavernoma (1.3 %, n = 3), and arachnoid cyst (0.9 %, n = 3). P1 findings are summarized in Table 2.
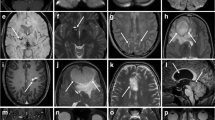
Of the positive results, 19/865 CT head scans (2.2 %) demonstrated P2 findings, defined as those requiring immediate change in management. These findings included subarachnoid hemorrhage (36.8 %, n = 7), sinus venous thrombosis (15.8 %, n = 3), intracranial mass (15.8 %, n = 3), subdural hematoma (10.5 %, n = 2), possible aneurysm (5.3 %, n = 1), bone lesions (5.3 %, n = 1), hydrocephalus (5.3 %, n = 1), and a large pineal cyst (5.3 %, n = 1) (see Table 3).
After calculating the incidence of positive findings on the initial non-enhanced CT, follow-up testing was then examined. The average period of time between the initial exam and the follow-up test was 147 days (minimum 0 days, maximum 584 days). There were 257 patients who underwent further testing, most commonly lumbar puncture (35.8 %). Other possible tests included a second non-enhanced CT head (10.5 %), CT angiogram (29.6 %), CT venogram (1.1 %), MRI (22.6 %), and one case of conventional angiography (0.4 %) (Table 4). The results of each of the second tests were then categorized into the same P0, P1, and P2 categories as the initial head CT scans. There were 19/257 (7.4 %) secondary tests that increased the severity of findings from P0 or P1 (clinically insignificant) to a clinically significant P2 result (Table 5). The LP was the most common test, and meningitis was the most common diagnosis (10/19, 52.6 %). Other pathologies included aneurysms (6/19, 31.6 %), possible fibromuscular dysplasia (1/19, 5.2 %), idiopathic intracranial hypertension at LP (1/19, 5.2 %), and an occluded right internal carotid artery with good collateral flow (1/19, 5.2 %). However, if LP is excluded and only imaging follow-up is analyzed, then eight of 164 (4.9 %) secondary exams changed the severity of diagnosis. Interestingly, only one of 58 MRIs that were performed after initial CT changed the severity of the diagnosis.
Discussion
Headache is a very frequent complaint in the ED. While most cases are benign, headache may be secondary to a more serious pathology, such as subarachnoid hemorrhage (due to ruptured aneurysm), intracranial mass, or infection. Reducing costs and overutilization of imaging have become an increasing issue as the population ages, and hospitals must manage limited health-care resources. It is well known that ED care is more expensive than outpatient or ambulatory care [2].
Many studies have demonstrated the low yield of imaging evaluation for isolated headache (non-traumatic without specific neurologic findings) [2, 4, 6, 14]; however, most of these studies included outpatients. Jordan et al. (2009) found that in 882 patients presenting to the ED, 9 patients (1.02 %) demonstrated clinically significant findings on non-enhanced CT [2]. It is interesting to note that our results yielded a higher incidence of findings of 2.2 %. Excluding patients with fever may have removed those patients with possible meningitis, which most commonly have negative CT scans. The use of third-generation CT scanners and multi-planar reformats may have potentially increased our sensitivity. The increased yield could also be explained by more selective use of CT by the ED physicians at our institution, which could be related to increased awareness of over-utilization of imaging, new clinical guidelines, and efforts of cost containment.
The second aspect of our study found that follow-up testing on patients who initially presented to the ED with headache is also of low yield (19/257, 7.4 %), although higher yield than initial non-enhanced CT. Presumably, these patients received more workup due to atypical features or non-response to therapy. Excluding lumbar puncture (imaging follow-up only), the yield was even lower at 4.9 %. To our knowledge, this has not been previously described. Some of the diagnoses significantly affected management, including possible fibromuscular dysplasia and a 2.4-cm internal carotid artery aneurysm. However, other diagnoses such as tiny suspected aneurysms may be unrelated to the presentation of headache and may never become clinically significant in the patient’s lifetime; however, these patients inevitably receive multiple follow-up exams to ensure stability over time.
The largest limitation to this part of our study is that we were only able to obtain follow-up information from our own institution. If patients received imaging at another hospital, then this would not be captured in our results. As this was a retrospective study, it was also difficult to delineate why each patient received further testing and which physician ordered each test (neurologist, ED physician, family physician, or another care provider).
The American College of Radiology (ACR) Expert Panel on Neuroimaging recently updated the Appropriateness Criteria for Headache in July 2014 [15] in conjunction with a multidisciplinary panel of experts. The guidelines recommend that general screening for isolated headache by CT or MRI is not warranted in the vast majority of patients. However, when the history, physical exam, or neurologic examination elicits certain “red flags” or critical features of headache, then imaging investigation may be required to exclude a secondary cause [15]. In addition, if the patient fails conventional therapy or atypical features are present, then imaging may be appropriate [15]. Worrisome characteristics include but are not limited to “thunderclap” headache, headache following exertion, headache radiating down the neck, headache in patients with human immunodeficiency virus (HIV), patients with a history of cancer, and temporal headache in an older patient [2, 15].
Conclusion
Our study is similar to previous studies and confirms that CT imaging for non-traumatic non-focal headache in the emergency department has low yield (2.2 % at our institution). Furthermore, subsequent imaging of these patients with more advanced techniques, such as CTA or MRI, is of limited utility but can change the severity of diagnosis in a small number of cases (4.9 %). It is well known that ED care is more expensive than outpatient care. CT imaging for headaches in the ED is a long-standing and widespread issue. Implementation of appropriateness criteria, clinical decision algorithms, and computerized decision support tools are becoming more commonplace and should help physicians better manage our finite health-care resources.
References
Stovner L, Hagen K, Jensen R, Katsarava Z, Lipton R, Scher A, Steiner T, Zwart JA (2007) The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia 27(3):193–210. doi:10.1111/j.1468-2982.2007.01288.x
Jordan YJ, Lightfoote JB, Jordan JE (2009) Computed tomography imaging in the management of headache in the emergency department: cost efficacy and policy implications. J Natl Med Assoc 101(4):331–335
Kahn CE Jr, Sanders GD, Lyons EA, Kostelic JK, MacEwan DW, 7Gordon WL (1993) Computed tomography for nontraumatic headache: current utilization and cost-effectiveness. Can Assoc Radiol J 44(3):189–193
Jordan JE, Ramirez GF, Bradley WG, Chen DY, Lightfoote JB, Song A (2000) Economic and outcomes assessment of magnetic resonance imaging in the evaluation of headache. J Natl Med Assoc 92(12):573–578
Akpek S, Arac M, Atilla S, Onal B, Yucel C, Isik S (1995) Cost-effectiveness of computed tomography in the evaluation of patients with headache. Headache 35(4):228–230
Gilbert JW, Johnson KM, Larkin GL, Moore CL (2012) Atraumatic headache in US emergency departments: recent trends in CT/MRI utilisation and factors associated with severe intracranial pathology. Emerg Med J 29(7):576–581. doi:10.1136/emermed-2011-200088
Perry JJ, Stiell IG, Sivilotti ML, Bullard MJ, Hohl CM, Sutherland J, Emond M, Worster A, Lee JS, Mackey D, Pauls M, Lesiuk H, Symington C, Wells GA (2013) Clinical decision rules to rule out subarachnoid hemorrhage for acute headache. JAMA 310(12):1248–1255. doi:10.1001/jama.2013.278018
Bent C, Lee PS, Shen PY, Bang H, Bobinski M (2015) Clinical scoring system may improve yield of head CT of non-trauma emergency department patients. Emerg Radiol. doi:10.1007/s10140-015-1305-x
Gupta A, Ip IK, Raja AS, Andruchow JE, Sodickson A, Khorasani R (2014) Effect of clinical decision support on documented guideline adherence for head CT in emergency department patients with mild traumatic brain injury. J Am Med Inform Assoc 21(e2):e347–e351. doi:10.1136/amiajnl-2013-002536
Gunes Tatar I, Aydin H, Kizilgoz V, Yilmaz KB, Hekimoglu B (2014) Appropriateness of selection criteria for CT examinations performed at an emergency department. Emerg Radiol 21(6):583–588. doi:10.1007/s10140-014-1234-0
Knaus WA, Davis DO (1978) Utilization and cost-effectiveness of cranial computed tomography at a university hospital. J Comput Assist Tomogr 2(2):209–214
Knaus WA, Wagner DP, Davis DO (1981) CT for headache: cost/benefit for subarachnoid hemorrhage. AJR 136(3):537–542. doi:10.2214/ajr.136.3.537
Larson EB, Omenn GS, Lewis H (1980) Diagnostic evaluation of headache. Impact of computerized tomography and cost-effectiveness. JAMA 243(4):359–362
Sempere AP, Porta-Etessam J, Medrano V, Garcia-Morales I, Concepcion L, Ramos A, Florencio I, Bermejo F, Botella C (2005) Neuroimaging in the evaluation of patients with non-acute headache. Cephalalgia 25(1):30–35. doi:10.1111/j.1468-2982.2004.00798.x
Douglas AC, Wippold FJ 2nd, Broderick DF, Aiken AH, Amin-Hanjani S, Brown DC, Corey AS, Germano IM, Hadley JA, Jagadeesan BD, Jurgens JS, Kennedy TA, Mechtler LL, Patel ND, Zipfel GJ (2014) ACR Appropriateness Criteria Headache. J Am Coll Radiol 11(7):657–667. doi:10.1016/j.jacr.2014.03.024
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Quon, J.S., Glikstein, R., Lim, C.S. et al. Computed tomography for non-traumatic headache in the emergency department and the impact of follow-up testing on altering the initial diagnosis. Emerg Radiol 22, 521–525 (2015). https://doi.org/10.1007/s10140-015-1314-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-015-1314-9