Abstract
Transthoracic ultrasound (US) is useful in the evaluation of a wide range of peripheral parenchymal, pleural, and chest wall diseases. Furthermore, it is increasingly used to guide interventional procedures of the chest and pleural space. The role of chest US in the diagnosis of pneumothorax has been established, but comparison with lung computed tomography (CT) scanning has not yet been completely performed. The purpose of this study is to prospectively compare the accuracy of US with that of chest radiography in the detection of pneumothorax, with CT as the reference standard. One hundred ninety-seven patients who were evaluated by spiral chest CT scan for various clinical indications were prospectively evaluated. Ultrasonography was performed by a radiologist, blinded to the chest CT findings. Sensitivity, specificity, and accuracy of ultrasound in the detection of pneumothorax were then compared with chest CT scan. CT scan showed pneumothorax in 92 patients. Sonography and plain X-ray of the chest revealed 74 and 56 cases of pneumothorax, respectively. Statistical analysis disclosed the US to be 80.4 % sensitive and 89 % specific in the detection of pneumothorax with an overall accuracy of 85 %. In this study, US was more sensitive than chest radiography in the detection of pneumothorax. The results of this study suggest that thoracic US, when performed by trained individuals, can be helpful for the detection of pneumothorax.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pneumothorax or presence of air in the pleural space is one of the most common chest disorders. It is traditionally classified as spontaneous, traumatic, or iatrogenic. Primary spontaneous pneumothorax occurs in those without clinically apparent lung disease; secondary spontaneous pneumothorax is a complication of preexisting lung disease. Iatrogenic pneumothorax results from a complication of a diagnostic or therapeutic intervention. Traumatic pneumothorax is caused by penetrating or blunt trauma to the chest, with air entering the pleural space directly through the chest wall, visceral pleural penetration, or alveolar rupture due to sudden compression of the chest [1].
Primary spontaneous pneumothorax has an estimated incidence of between 7.4 cases (age-adjusted incidence) and 18 cases per 100,000 population per year among men and between 1.2 cases (age-adjusted incidence) and 6 cases per 100,000 population per year among women. It typically occurs in tall, thin boys and men between the ages of 10 and 30 years and rarely occurs in persons over the age of 40. Smoking cigarettes increases the risk of primary spontaneous pneumothorax in men by as much as a factor of 20 in a dose-dependent manner [2, 3].
Several imaging modalities can be used for the detection of pneumothorax. Chest X-ray is the most common radiologic investigation in suspected cases; however, there are shortcomings in the evaluation of loculated pneumothorax and unstable patients [4, 5].
Chest computed tomography (CT) scan is the most sensitive imaging modality for the diagnosis of pneumothorax even in subtle cases. Both conventional radiography (CR) and CT scan have limitations in patients who are not stable enough for radiologic investigations. Ultrasonography (US) is another imaging modality which can be easily performed even in unstable patients, and lack of ionizing radiation is another advantage of this procedure [4, 5].
This study was conducted to evaluate the sensitivity and specificity of ultrasonography in the detection of pneumothorax. In this respect, CT scan was used as the gold standard imaging modality, and US and CR findings were compared with CT scan results.
Patients and method
Ninety-two patients with pneumothorax were prospectively studied over a 26-month period. These patients who underwent chest CT scan due to respiratory problems (caused by trauma or underlying lung disorders or sudden respiratory distress) were included in this study, and pneumothorax in these patients had been confirmed by chest CT scan as the imaging modality of choice. Also, the patients were evaluated by chest radiograph and ultrasound. Those with unstable vital signs, emergency indications for chest tube insertion or subcutaneous emphysema, precluding ultrasound examination were excluded from the study.
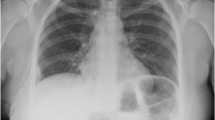
Also, 105 patients in whom pneumothorax was excluded on the base of normal chest CT scan were enrolled in the study as the control group. US was performed after chest CT scan and chest radiograph by logiq 7, GE, USA, ultrasound machine, with a 7.5-MHz linear array probe. Two radiologists and a radiology resident contributed in this study. An ultrasound-performing radiologist was unaware of the CT scan results. In the patients who were stable enough, chest US was performed in supine and sitting positions and in anterior, lateral, and posterior aspects of the chest cavity. In those who were not able to sit, US was performed only in supine position, and anterolateral areas were evaluated. All the US exams were performed within 48 h after the chest CT scan acquisition. The presence of pneumothorax was confirmed ultrasonographically by the disappearance of normal lung sliding and lack of comet tail artifact at the pleural interface (Fig. 1).
In majority of the cases, chest X-ray was performed in the upright PA position, and in others, supine radiographs were obtained for various reasons such as hemodynamic instability and orthopedic injuries. Criteria for radiographic diagnosis of pneumothorax included visualization of the visceral pleura with loss of lung markings laterally and detection of a deep sulcus sign.
CT was performed using a CT scanning unit (Highspeed Advantage Dual Slice CT Scanner, GE Medical Systems, Milwaukee, WI, USA) and IV administration of 2-ml/kg contrast agent (Omnipaque 300 strength), when indicated. Helical sections were obtained at a pitch factor of 1 and slice thickness of 5 mm. Statistical analysis was performed using SPSS software (SPSS Inc., Chicago, IL, USA), and the sensitivity, specificity, and accuracy of ultrasound and chest X-ray were evaluated considering CT scan as the gold standard.
Results
Ninety-two patients with CT-proven pneumothorax were enrolled in the study. Of these, 67 cases (72.8 %) showed nonloculated pneumothorax, and in 25 cases (27.2 %), encysted pneumothorax was found. Loculated cases of pneumothorax were 11, 12, and 2 in the anterior, lateral, and posterior aspects of the chest cavity, respectively. US demonstrated the presence of pneumothorax in 53 patients (79 %) with nonloculated pneumothorax and 21 patients (84 %) with loculated pneumothorax, showing overall sensitivity of near 80 %.
Chest X-ray of the patients disclosed 56 cases (60.8 %) of pneumothorax; of these, 50 (74.6 %) were nonloculated and 6 were loculated with the overall sensitivity of 61 %. In this study, 105 cases with the absence of pneumothorax in their CT scans were also studied. Of these, 94 patients revealed normal US findings, and 11 cases showed ultrasonographic signs of pneumothorax (false positive cases). However, chest X-ray showed only two cases with signs of pneumothorax (false positive cases). Accuracy, sensitivity, and specificity of these two imaging modalities are compared as seen in Table 1.
Discussion
The diagnosis of pneumothorax is generally made with combination of symptoms and physical exam and is confirmed with chest radiography or occasionally computed tomographic scans. A pneumothorax which is apparent on the chest CT but not visible on the chest radiograph is called an occult pneumothorax which occur in 40 % of traumatic pneumothoraces (Fig. 2). It can be due to supine chest radiography, which is commonly performed in the setting of trauma and ventral location of extra pleural air in supine patients [6]. Although moderate pneumothorax is generally not life-threatening, delays in diagnosis and therapy may result in progression of respiratory compromise. The absence of immediate radiographic capabilities because of the patient’s instability, remote location, or other factors complicates the diagnosis of pneumothorax. Furthermore, the reliability of supine chest radiography is not absolute, and misdiagnosis may occur in up to 30 % of all pneumothoraces. Chest radiographs taken on expiration or in the lateral decubitus position have been proposed but are not yet routinely performed [7]. Considering the shortcomings of routine chest X-ray in the diagnosis of pneumothorax, chest CT has been introduced as the gold standard but necessitates transfer of critically ill patients out of the ICU. Besides, CT cannot always be performed promptly. Pneumothorax can quickly become life-threatening in a ventilated patient. In some instances, any delay in provision of radiologic evidence may be deleterious. Ultrasound can be an important alternative to some of these problems.
Although in preliminary studies, chest X-ray was reported to be more sensitive than US, subsequent investigations showed higher accuracy of US in the detection of pneumothorax and even rib fracture in patients with blunt trauma [8]. This can be due to the advent of newer machines and higher frequency probes.
Rowan et al. reported 27 trauma patients; in their study, US was more sensitive and accurate than supine chest radiography and as sensitive as thoracic CT in the detection of pneumothoraces. They concluded that thoracic US, when performed by trained individuals, can enable definitive exclusion of pneumothorax. As a corollary, they believe that thoracic US should be added to the currently performed FAST examination in trauma cases and be labeled as the expanded FAST examination [7, 9]. Goodman et al. reported 13 cases of pneumothorax following CT-guided biopsy. In this patient group, US was more sensitive than erect chest radiography in the detection of pneumothorax. Both have a specificity of 100 %. This study suggests that US may prove valuable in pneumothorax detection when rapid conventional radiography is not possible or practical and in circumstances where US is readily available, such as during US-guided interventional procedures [10, 11]. Lichtenstein et al. have studied 41 pneumothoraces with 146 hemithoraces in 73 critically ill patients: US visualization of “lung sliding” was always correlated with the absence of pneumothorax (ESM_1). From this elementary sign alone, they concluded that it was possible to exclude at least anterior pneumothorax promptly and at the bedside of a mechanically ventilated patient. This was the major finding of this study [12].
In agreement with these studies, we also found US to be significantly more sensitive compared with simple X-ray, but not as sensitive as CT scan. One reason for this can be the larger number of cases in our study. Besides, some of our false negative cases were those with loculated pneumothoraces, which detection by US was more difficult, especially those at apices of the lungs with poor US windows (Fig. 3). Thus, although US can be quite as sensitive as CT in the detection of free pneumothoraces, there are some drawbacks in these loculated cases. However, considering our results, US is much more effective in detecting loculated pneumothoraces (21 out of 25 cases) compared with chest X-ray (6 out of 25).
In addition, the time interval within which US is performed influences its accuracy, as is investigated by Dente et al. [13]. They studied fourteen hospitalized patients with thoracostomy tube in place to treat traumatic pneumothorax. Patients underwent serial delayed bedside US. Significant decline in both sensitivity and specificity of US was detected, after 24-h appearance of pneumothorax. It was concluded that US evaluation for pneumothorax was very accurate for the first 24 h after insertion of the thoracostomy tube, but the accuracy and especially the positive predictive value were not sustained over time, possibly as a result of formation of intrapleural adhesion. Considering our results, US was found to be significantly more sensitive in the detection of pneumothorax, especially in small amounts, in comparison with plain X-ray. Absence of ionizing radiation and easy performance are other advantages of this imaging modality. We conclude that US, when performed by trained individuals, can be helpful for rapid detection of pneumothorax.
References
Chee CB, Abisheganaden J, Yeo JK, Lee P, Huan PY, Poh SC, Wang YT (1998) Persistent air-leak in spontaneous pneumothorax—clinical course and outcome. Respir Med 92(5):757–761
Killen D, Gobbel W. Spontaneous pneumothorax. Boston: Little, Brown; 2001
Schramel FM, Postmus PE, Vanderschueren RG (1997) Current aspects of spontaneous pneumothorax. Eur Respir J 10(6):1372–1379, Review
Tocino IM, Miller MH, Fairfax WR (1985) Distribution of pneumothorax in the supine and semirecumbent critically ill adult. AJR Am J Roentgenol 144(5):901–905
Wall SD, Federle MP, Jeffrey RB, Brett CM (1983) CT diagnosis of unsuspected pneumothorax after blunt abdominal trauma. AJR Am J Roentgenol 141(5):919–921
Soldati G, Testa A, Sher S, Pignataro G, La Sala M, Silveri NG (2008) Occult traumatic pneumothorax: diagnostic accuracy of lung ultrasonography in the emergency department. Chest 133(1):204–211
Rowan KR, Kirkpatrick AW, Liu D, Forkheim KE, Mayo JR, Nicolaou S (2002) Traumatic pneumothorax detection with thoracic US: correlation with chest radiography and CT—initial experience. Radiology 225(1):210–214
Turk F, Kurt AB, Saglam S (2010) Evaluation by ultrasound of traumatic rib fractures missed by radiography. Emerg Radiol 17(6):473–477
Sistrom CL, Reiheld CT, Gay SB, Wallace KK (1996) Detection and estimation of the volume of pneumothorax using real-time sonography: efficacy determined by receiver operating characteristic analysis. AJR Am J Roentgenol 166(2):317–321
Goodman TR, Traill ZC, Phillips AJ, Berger J, Gleeson FV (1999) Ultrasound detection of pneumothorax. Clin Radiol 54(11):736–739
Sartori S, Tombesi P, Trevisani L, Nielsen I, Tassinari D, Abbasciano V (2007) Accuracy of transthoracic sonography in detection of pneumothorax after sonographically guided lung biopsy: prospective comparison with chest radiography. AJR Am J Roentgenol 188(1):37–41
Lichtenstein D, Meziere G, Biderman P, Gepner A (1999) The comet tail artifact: an ultrasound sign ruling out pneumothorax. Intensive Care Med 25:383–385
Dente CJ, Ustin J, Feliciano DV, Rozycki GS, Wyrzykowski AD, Nicholas JM, Salomone JP, Ingram WL (2007) The accuracy of thoracic ultrasound for detection of pneumothorax is not sustained over time: a preliminary study. J Trauma 62(6):1384–1389
Acknowledgments
Our work was supported by the Medical Imaging Research Center, Radiology Department, Namazi Hospital, affiliated to Shiraz University of Medical Sciences, Shiraz, Iran.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
(MPG 3172 kb)
Rights and permissions
About this article
Cite this article
Jalli, R., Sefidbakht, S. & Jafari, S.H. Value of ultrasound in diagnosis of pneumothorax: a prospective study. Emerg Radiol 20, 131–134 (2013). https://doi.org/10.1007/s10140-012-1091-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-012-1091-7