Abstract
We present the case of an 18-year-old man involved in a fall with blunt abdominal trauma. The patient had hypovolemic shock and findings of an acute abdomen. Initial computed tomography (CT) showed pulmonary contusion, pneumohemothorax, hemoperitoneum, hepatic contusion, right kidney laceration and vascular avulsion, rupture of the mesenteric vein, rupture of the right rectus muscle with bowel hernia, and infrarenal aortic dissection. There were no signs of limb or medullar ischemia. After hemodynamic stabilization and surgical repair of the associated lesions, the dissection was successfully treated with a self-expanding aortic Wallstent. Postprocedure CT showed a well-positioned patent stent and the patient was discharged asymptomatic. Percutaneous endovascular stent implantation is minimally invasive and seems to be a safe treatment for traumatic dissection of the abdominal aorta.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute traumatic dissection of the aorta secondary to blunt trauma is an infrequent and potentially fatal injury with growing incidence due to motor vehicle accidents, sports accidents, arteriosclerosis, and increasing age. Most cases of blunt traumatic aortic lesions are confined to the descending thoracic aorta and the isthmus. Isolated dissection of the abdominal aorta has been rarely reported [1]. Due to the presence of severe associated visceral lesions, it may go initially unrecognized in up to one third of the cases [1, 2]. A prompt diagnosis is essential, as dissections of the abdominal require treatment because of the high morbidity and mortality associated with conservative medical therapy [3]. However, the optimum treatment remains controversial [1, 4].
We present a case of acute traumatic dissection of the infrarenal abdominal aorta, and its successful therapy by percutaneous placement of an endovascular stent.
Case report
An 18-year-old man involved in an industrial accident was admitted to our hospital. He had fallen from a height of 13 m and struck his waist against a barrier. On arrival at the emergency department he was conscious but he was in a hypovolemic shock which responded well to the administration of fluids. He presented abdominal defense.
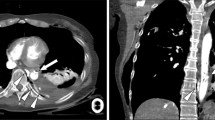
Thoracoabdominal contrast-enhanced computed tomography (CT) revealed a bilateral pulmonary contusion, pneumohemothorax, hemoperitoneum, hepatic contusion, a shattered right kidney with avulsion of the renal hilium, a rupture of the mesenteric vein, a rupture of the right rectus muscle with bowel hernia, and the dissection of the infrarenal aorta. The intimal tear of the dissection was identified, beginning 4 cm below the left renal artery and extending 1.2 cm distally, without thrombosis of the false lumen (Fig. 1). There was no dissection of the thoracic aorta. The patient was transferred to the operating room where he underwent right nephrectomy, repair of the anterior abdominal wall, and vascular suture of the mesenteric vein. As the hypovolemic shock was under control, and there were no signs of limb or medullar ischemia, we decided not to treat the aortic dissection at the first intervention.
Initial CT scan. Axial CT image (a) shows infrarenal aortic dissection, right kidney injury with avulsion of the renal hilium, and rupture of the right rectus muscle. Coronal and oblique sagittal reformatted CT images show the intimal flap (arrow) below the left renal artery and without reaching the aortic bifurcation
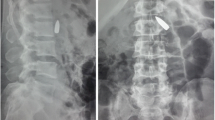
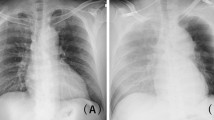
On a control angio-CT performed 24 h after admission, a progression of the dissection of the infrarenal aorta was observed, with the intimal tear 4 cm distal to the left renal artery, extending 6 cm, albeit without reaching the aortic bifurcation (Fig. 2). The patient remained hemodynamically stable and without signs of ischemia. Under angiographic control, using a 7F-femoral approach, an endovascular self-expanding Wallstent (Boston Scientific, 18 mm diameter and 60 mm length) was placed from 2 cm below the left renal artery until 1 cm above the bifurcation (Fig. 3). The patient had an uneventful postoperative course and on day 19, he was discharged home asymptomatic. Six months after the percutaneous endovascular stent implantation, the patient is asymptomatic, and a follow-up angio-CT demonstrated a well-positioned patent stent (Fig. 4).
Discussion
In the setting of nonpenetrating trauma aortic dissection is a less frequent lesion than aortic rupture. Most of these cases affect the thoracic portion of the aorta [5, 6]. There is little information on the frequency of isolated dissection of the abdominal aorta. Berthert et al. [1] found an incidence of 8% in a series of 87 patients with blunt aortic trauma. The true incidence, however, may be higher, as many of these patients do not reach the hospital alive or die shortly after, without the diagnosis being made.
There seems to be two possible mechanical factors responsible for traumatic abdominal aortic dissection: direct compression of the aorta against the vertebral column resulting from the blunt trauma [7, 8], and indirect compression as the result of deceleration force of the body [9]. In addition, underlying vascular disease, such as atherosclerosis, hypertension or Marfan’s disease, play an important role in traumatic aortic dissection, as less force is required to tear the intima in these conditions [10]. The increasing prevalence of atheromatous plaques with age renders older patients more susceptible to aortic injuries and explains the higher frequency of traumatic aortic dissection in this population group. However, atherosclerosis is not a prerequisite for the traumatic dissection of the aorta that has been observed in all age groups. In our patient, who was 18 years old, no vascular disease was present, and the blunt trauma seems to be the sole cause of the dissection of the abdominal aorta.
Because of the rarity of traumatic abdominal aortic dissection, the severity of the associated visceral lesions in the setting of a blunt trauma and the hidden vascular symptomatology, the dissection may go initially unrecognized. A delayed diagnosis has been reported in up to 34.3% of the cases [1, 2].
Patients usually present with severe abdominal pain and signs of acute abdomen. Other findings include: hypovolemic shock, paraplegia, lower limb ischemia, and back pain [1, 12, 13]. The diagnosis is usually based on contrast-enhanced CT and/or angiography. CT, particularly multirow CT angiography is currently the method of choice for evaluation of patients with acute vascular disease following blunt trauma [14]. Compared to conventional angiography, multirow CT angiography has the advantage of assessing the vessels and also the adjacent structures and associated lesions. It has been reported to detect aortic dissections with an accuracy of 100% [15]. The diagnosis is based on the detection of the intimal flap dividing the aorta into a true lumen and a false lumen. Other findings may be observed including retroperitoneal hematoma or abnormal opacification of the aorta lumen. The thrombosis of the false lumen or the presence of an aortic aneurysm may make the detection of the dissection in older patients difficult. The thoracic aorta must be always examined to rule out dissection of this portion. Angiography, the gold standard diagnostic tool, shows the intimal flap between the two lumens and smooth narrowing of the infrarenal aorta, but the dissection may be overlooked if the false lumen is thrombosed.
Associated visceral lesions are common [1, 11–13], and must always be looked for. Especial attention should be paid to bowel lesions that become potential sources of bacterial contamination during surgical repair of the aorta.
Because of the likely progression of dissection and the high mortality rate with conservative medical management, traumatic abdominal aortic dissection must be repaired. There are three possible approaches: conventional surgery, percutaneous balloon fenestration, and percutaneous stent placement. Depending on the extension of the dissection and the damage to the aorta, surgical repair may be achieved by simple flap suture, or prosthetic graft replacement. The surgical mortality is higher in traumatic than in spontaneous dissections due to the coexistence of retroperitoneal venous injury and bacterial contamination from associated bowel lesions. Urgent conventional surgery is recommended in patients with uncontrolled hemodynamic shock, lower limb ischemia, or ischemic medullar paraplegia [1].
Percutaneous balloon fenestration either followed [12] or not followed [13] by stent placement is a less invasive method feasible in selected cases, such as dissections originating above the renal arteries, or when it is technically difficult to place a stent to the arterial wall of the iliac bifurcation.
In recent years, endovascular stenting has been successfully used for the treatment of traumatic abdominal aorta dissection [1, 11, 16, 17], mainly in infrarenal dissections. Percutaneous stent placement has advantages over open surgery repair, including avoidance of aortic cross-clamping, retroperitoneal dissection, less blood transfusion requirements, shorter time of surgical intervention, and less infectious complications. However, hemodynamically unstable patients, or those with threatened lower limbs or with tortuous iliac arteries should be managed with conventional surgery. Our patient, who presented with hemodynamic shock and a relatively short dissection without evidence of ischemia, underwent first laparotomy and surgical treatment of the visceral lesions. A surgical repair of the dissection at this time would have put the graft at risk of infection. We chose the endovascular approach in a second intervention, once the shock was controlled, and because of the absence of ischemic symptoms. Like Berthet et al. [1], we believe that for hemodynamically stable patients with viable extremities, endovascular stent placement might be the first therapeutic option for traumatic abdominal aortic dissection. Longer follow-up of patients treated with endovascular stents is needed to evaluate long-term complications and the final outcome of the procedure, so that the suitable candidates for this technique can be identified. This is of utmost importance because this therapeutic option is being offered to young patients with a long life expectancy.
Acute dissection of the abdominal aorta secondary to blunt trauma is a rare injury with a high morbidity and mortality. However, with the widespread use of multirow CT for evaluation of patients in the emergency setting, an increase in the number of diagnosis of (even very short) traumatic aortic dissection, as well as an earlier detection of them, are expected. In this regard, a well-adjusted scanning with thin collimation and triggered injection of intravenous contrast medium is essential. As this case illustrates, percutaneous stent placement can be successfully employed for the treatment of acute traumatic dissections of the abdominal aorta, even in shocked patients with severe visceral injuries with a two-step approach. It may be a good option for the only intervention for patients whose associated lesions are going to be managed conservatively.
References
Berthet JP, Marty-Ané CH, Vecrapen R, Picard E, Mary H, Alric (2003) Dissection of the abdominal aorta in blunt trauma: endovascular or conventional surgical management? J Vasc Surg 38:997–1004
Solovei G, Alame A, Bardoux J et al (1994) Paraplegia and dissection of the abdominal aorta after closed trauma. A propos of a case. Current review of the literature (1982–1993). J Chir (Paris) 131:236–244
Lock JS, Huffman A, Johnson RC (1987) Blunt trauma to the abdominal aorta. J Trauma 27:674–677
Fattori R, Napoli G, Lovato L, Russo V, Pacini D, Pierangeli A et al (2002) Indication for timing of, and results of catheter-based treatment of traumatic injury to the aorta. AJR Am J Roentgenol 179:603–609
Fisher RG, Hadlock F (1981) Laceration of the thoracic aorta and brachiocephalic arteries by blunt trauma: report of 54 cases and review of the literature. Radiol Clin North Am 19:91–110
Perchinsky M, Gin K, Mayo JR (1998) Trauma-associated dissection of the thoracic aorta. J Trauma 45:626–629
Campbell DK, Austin RF (1969) Seat belt injury: injury of the abdominal aorta. Radiology 92:123–124
Nunn DB (1973) Abdominal aortic dissection following non penetrating abdominal trauma. Am Surg 39:177–179
Dajee H, Richardson JW, Iype MO (1978) Seatbelt aorta: acute dissection and thrombosis of the abdominal aorta. Surgery 85:263–267
Clark JC, Milroy CM (2000). Injuries and deaths of pedestrians. In: Mason JK, Purdue BN (eds) The pathology of trauma, 3rd edn. Arnold, London, pp 17–29
Picard E, Marty-Ane CH, Vernhet H, Sessa C, Lesnik A, Senac JP et al (1998) Endovascular management of traumatic infrarenal abdominal aortic dissection. Ann Vasc Surg 12:515–521
Peterson AH, Williams DM, Rodriguez JL, Francis IR (1995) Percutaneous treatment of a traumatic aortic dissection by balloon fenestration and stent placement. AJR Am J Roentgenol 164:1274–1276
Nisihimura K, Kanaoka Y, Ikebuchi M, Hiroe T, Tachibana M, Ishiguro S et al (2000) J Vasc Surg 32:616–618
Alkadhi H, Wildermuth S, Desbiolles L, Schertler T, Crook D, Marincek B, Boehm T (2004) Vascular emergencies of the thorax after blunt and iatrogenic trauma: multi-detector row CT and three-dimensional imaging. Radiographics 24:1239–1255
Yoshida S, Akiba H, Tamakawa M et al (2003) Thoracic involvement of type A aortic dissection and intramural hematoma: diagnostic accuracy-comparison of emergency helical CT and surgical findings. Radiology 228:430–435
Marty-Ane CH, Alric P, Prudhomme M, Chircop R, Serres-Cousine O, Mary H (1996) Intravascular stenting of traumatic abdominal aortic dissection. J Vasc Surg 23:156–161
Vernhet H, Marty-Ane CH, Lesnik A, Chircop R, Serres-Cousine O, Picard E et al (1997) Dissection of the abdominal aorta in blunt trauma: management by percutaneous stent placement. Cardiovasc Intervent Radiol 20:473–476
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Martí, M., Pinilla, I., Baudraxler, F. et al. A case of acute abdominal aortic dissection caused by blunt trauma. Emerg Radiol 12, 182–185 (2006). https://doi.org/10.1007/s10140-006-0473-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-006-0473-0