Abstract
Congenital dermal sinus tracts are frequently a cause of recurrent meningitis. We present a case of a rare lower cervical dermal sinus and an associated intraspinal abscess causing meningitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meningitis is a frequent presentation of children in the emergency department. Dermal sinus tracts are an unusual source of meningitis: congenital structural malformations that occur early in embryogenesis can provide a pathway for microorganisms to spread from the skin and delve into the subcutaneous tissue, ending anywhere from the immediate subcutaneous tissues to the spinal cord. They are frequently responsible for recurrent meningitis, and can cause intraspinal abscesses. Careful physical examination in the emergency room can direct the clinician towards appropriate antibiotic choice and surgical management.
Case report
A 14-month-old boy was brought to our emergency department by his parents. He had been discharged the day before from another hospital where he had been treated for pneumonia and a retropharyngeal abscess. On the day of arrival at our institution, he had a fever of 38.2 °C, refused to sit up, refused to unclench his fists, would not drink, and had only one wet diaper in 24 h.
The patient had a history of multiple physical anomalies including low set ears, stenotic left external ear, malformed upper lip, bifid uvula, malformed left third and fourth digits of the hand, hypospadias, and two sacral dimples. A skin tag in the lower cervical/upper thoracic midline region was observed which intermittently discharged an exudative fluid. The child's workup for chromosomal abnormalities was negative. His lungs were clear to auscultation. His breathing was not stridorous, and cervical adenopathy was not observed. On direct visualization, his posterior oropharynx was normal. Head measurements revealed that his head circumference was at 97%. His lab work was significant for an elevated white blood cell count of 24.4×109/l with 57.5% granulocytes, 33% lymphocytes, and 2.1% monocytes.
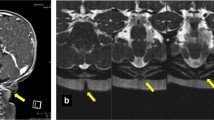
Radiographic studies performed in the emergency department included a plain radiograph of the lateral neck (Fig. 1) which revealed prominent prevertebral soft tissues displacing the airway anteriorly. A CT scan of the head showed lateral and third ventriculomegaly without evidence of hydrocephalus. CT of the neck did not reveal a retropharyngeal abscess. It demonstrated a midline posterior subcutaneous soft tissue defect and spina bifida of C7 (Fig. 2). Subsequent MRI of the brain and spine revealed agenesis of the corpus callosum and gray matter heterotopia, and confirmed dilated lateral and third ventricles without transependymal migration of cerebrospinal fluid. Gadolinium-enhanced MRI of the spine revealed a sinus tract at C6–C7 communicating with an intraspinal abscess with an enhancing wall (Fig. 3), with abnormal signal in the adjacent spinal cord representing myelitis (Fig. 4).
Sagittal post-gadolinium MRI with fat saturation depicts an irregular, 3.0-cm posterior epidural abscess (large white arrow) communicating with the dermal sinus tract (small white arrow) and compressing the cervical spinal cord. Spin echo T1-weighted image, TR=500 ms, TE=14 ms, FOV 24×24 cm, 3 mm slice thickness/1 mm gap, 256×160 matrix, NEX=1, time=3 min 2 s
Discussion
A dermal sinus tract is an epithelium-lined tract that originates at the skin and delves deep into the body at various lengths. It ends in a cystic expansion which is called an epidermoid if it is lined by epithelium, or a dermoid if the lining is comprised by skin appendages like hair, sebaceous gland, and fat in addition to the epithelial lining [1].
Dermal sinuses are caused by incorrect separation of the cutaneous and neuroepithelial ectoderms during formation of the neural tube. In the third to fourth weeks of embryogenesis, the medullary tube starts closing in the middle of the embryo to form the neural tube, and this closure proceeds cranially and caudally. As this formation of the neural tube is occurring, the overlying ectoderm and mesoderm are also separating into layers. When this separation is altered, a dermal sinus tract can form that can terminate anywhere from the subcutaneous tissues to the intramedullary space of the central nervous system, anywhere along the course of the spine [2].
Spinal dermal sinus tracts occur, in decreasing order of frequency, at the sacrococcygeal, lumbar, occipital, thoracic, and cervical levels [1]. Approximately two-thirds terminate intradurally, especially the ones in the occipital, cervical, thoracic, and lumbar regions. The sacrococcygeal anomalies usually end in an extradural location [2]. Dermoids and epidermoids also occur in the suprasellar and parasellar region of the brain, with extension into the third or fourth ventricles, subarachnoid cisterns, and cerebellum. They can also occur in the pericranial or diploic regions of the orbit, temporal lobe, or the cerebellopontine angle [3].
On physical exam, the spectrum of findings of dermal sinuses includes deep dimples, presumed sinuses, skin tags, mass [2], hyperpigmented patch, hairy nevus, and hemangioma [4].
Dermal sinus tracts have been found in patients aging from newborn to 35 years old [1, 4, 5]. Approximately 75% of the patients present with infection [2], with 60% presenting with meningitis [1, 2, 4]. The remaining 15% present with cellulitis, abscess, infected dermoid, or osteomyelitis [2]. Most of these present before age 5 [6]. The etiologic organisms causing meningitis, frequently recurrent [4], include Staphylococcus aureus, Staph. epidermidis, Streptococcus pneumoniae, Strep. agalactiae, Haemophilus influenzae, Escherichia coli, Proteus species, Salmonella, and anaerobic organisms including Peptostreptococcus and Bacteroides [1, 4, 5, 6]. Intramedullary spinal abscesses have also been reported as a complication [7]. Rarely, intracranial dermoids and epidermoids cause chemical meningitis due to spontaneous leakage of their contents [3].
Management of a congenital dermal sinus involves appropriate antibiotics if the sinus is infected, together with surgical evaluation. Most dermal sinuses cephalad to the lumbosacral region, as in our case, should be excised during the newborn period. Controversy exists in the management of lumbosacral sinuses, with some authorities suggesting that pilonidal sinuses need not be operated on, but those with associated radiographic evidence of underlying bony defects should be prophylactically removed. Other authors have recommended complete removal of any sinus whose base cannot be exposed by pressure on the adjacent skin. If neurological symptoms occur, prompt surgery is needed. If a sinus is complicated by infection, surgery is to be performed once the infection is under control [2].
Clues to the presence of dermal sinus tracts lie in the history, physical exam, and imaging. A history of recurrent meningitis with detection of cutaneous anomalies in the cranial spinal axis should arouse the clinician's suspicion. MRI, as shown in our case, is an invaluable tool that noninvasively images the anomaly, its extent, and complications. The neurological symptoms and history of intermittently exudative midline lower cervical/upper thoracic skin tag were clues in our patient's history. Imaging, including CT showing the midline subcutaneous defect and spina bifida defect in the lower cervical spine, and MRI demonstrating the course of the dermal sinus tract and the associated abscess, led to the correct diagnosis and management. Retrospectively, the appearance of a retropharyngeal abscess on the lateral radiograph of the neck was most likely due to performance of a film in incomplete extension. Such pseudomass configurations pose a challenge that the radiologist needs to be aware of [8]. Perhaps the intraspinal abscess and associated meningeal irritation contributed to suboptimal radiographic evaluation of the retropharynx, i.e., they prevented full extension of the patient's neck. A lateral cervical spine radiograph obtained to evaluate the soft tissues of the neck must be performed in full inspiration and neck extension.
A dermal sinus tract, although most common in the lumbar region, may be present anywhere along the cranial spinal axis. It may lead to recurrent meningitis and, occasionally, intraspinal abscesses. Astute physical examination by the emergency room clinician and a high index of suspicion on the part of the emergency room radiologist can lead to a quick, accurate diagnosis. The treatment involves antibiotic coverage for microorganisms not usually associated with meningitis in children, and surgical consultation to remove the congenital structural defect.
References
Gurbani SG, Cho CT, Lee KR (1994) Staphylococcus epidermidis meningitis and an intraspinal abscess associated with a midthoracic dermal sinus tract. Clin Infect Dis 19:1138–1140
Powell KR, Cherry JD, Hougen TJ, Blinderman EE, Dunn MC (1975) A prospective search for congenital dermal abnormalities of the craniospinal axis. J Pediatr 87:744–750
Schwartz JF, Balentine JD (1978) Recurrent meningitis due to an intracranial epidermoid. Neurology 28:124–129
Andiran N, Coskun T, Ozaydin E, Secmeer G (1998) Recurrent meningitis associated with congenital paravertebral dermal sinus tract. Turk J Pediatr 40:121–125
Reimer CM (2001) Dermal sinus presenting as group B streptococcal meningitis. Arch Neurol 58:820–821
Givner LB, Baker CJ (1983) Anaerobic meningitis associated with a dermal sinus tract. Pediatr Infect Dis 2:385–387
Dev R, Husain M, Gupta A, Gupta RK (1997) MR of multiple abscesses associated with congenital dermal sinus. AJNR Am J Roentgenol 18:742–743
Swischuk LE (2000) Emergency imaging of the acutely ill or injured child, 4th edn. Lippincott Williams & Wilkins, Philadelphia, pp 119–121
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shah, R.K., Chaljub, G. & Swischuk, L.E. Lower cervical dermal sinus tract and associated intraspinal abscess causing meningitis in a child. Emergency Radiology 10, 160–162 (2003). https://doi.org/10.1007/s10140-003-0304-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-003-0304-5







