Abstract
Clearance of comedone is challenging in the treatment of acne, as it is very likely to develop into inflammatory lesions. However, there is lack of effective treatments for dense comedones. Comedone extractor has been widely employed by dermatologists, but the effect is temporary and may cause irritation. CO2 laser is a potential method for dense comedones, but the efficacy and safety need to be explored. In this single-center, randomized, single-blind, self-controlled study, the faces of patients with dense comedones were randomly assigned into two sides receiving either ultra-pulse dynamic CO2 laser or comedone extraction at an interval of 2 weeks for 4 sessions. After 4 treatments, the average comedone reduction rate of the CO2 laser was 64.49%, which was higher than that by the extractor (46.36%) (P < .001). 79.16% of the patients reached over 50% reduction by CO2 laser, while only 37.5% on extractor treated side reached 50% clearance. Texture index, porphyrin index, red zone, erythema index, and transepidermal water loss decreased after both treatments, and CO2 laser showed more improvement. There was no difference in hydration index and melanin index between the two treatments. No permanent or severe side effects were observed on both sides. The CO2 laser showed higher comedone clearance with lower pain scores than the comedone extractor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acne vulgaris (AV) is a common skin disease, which affects millions of patients [1]. Comedones are likely formed by abnormal proliferation and differentiation of infundibular keratinocytes [2]. According to the forms and size, comedones can be divided into microcomedones, ordinary comedones, sandpaper-like comedones, and macrocomedones [3]. Based on the Acne Assessment Scale, the number of comedones between 20-50 is described as Grade II, 50-100 is Grade III, and >100 comedones are referred to as Grade IV (dense comedones) [4]. Although comedones are considered noninflammatory lesions base on its clinical manifestation. In recent years, inflammatory factors are suggested in the pathological process in the formation of comedones [5]. Therefore, comedones are likely to develop into inflammatory lesions, especially for dense comedones [6, 7]. In order to limit the progession of acne, comedone control is key component.
Clinicians have been striving to explore treatments for comedones for decades. Comedones were once considered as mild to moderate AV, so topical medications are often recommended in clinical guidelines. At present, the first-line treatment for comedone is external retinoic, like Adapalene Gel and tretinoin cream, the irritation of which limits the application [8]. These topical medicines are somewhat effective for Grade-I and Grade-II comedones, which are fewer in number and smaller in size, but has little effects on Grade-IV comedones [9]. Oral isotretinoin could also be used for treating comedones, but teratogenicity, hepatotoxicity, and acne flaring after use make patients psychologically resistant to systemic medications [10, 11]. Besides, there are some physical therapies, including comedone extractors, syringes, tweezers, and some other tools that can remove comedones.
The comedone extractor was first devised by Dr. Henry Piffard in 1873 and has undergone a series of improvements and evolutions [12]. The modern comedone extractors widely used in clinical practice are mostly made of titanium alloy and are shaped with a pointed end for puncturing the surface and a safety pin at the other end to assist in squeezing out the contents [13]. This kind of tool is easy to operate and gradually becomes cheaper, thus is widely used all over the world to help remove comedones.
The CO2 laser is an infrared laser with 10600nm wavelength which targets water. Photothermal, photochemical, and photoacoustic effects of the CO2 laser synergistically promote skin regeneration, collagen remodeling, and regeneration [14]. Therefore, CO2 laser is widely used in the treatment of various skin diseases, such as acne scars, syringomas, onychomycosis, verruca, etc. [14,15,16,17] Ultra-pulse CO2 laser has higher energy density and deeper penetration compared with traditional CO2 laser, and the dynamic mode makes it more flexible and accurate.
In this study, we developed a high-density energy method by ultra-pulse dynamic CO2 laser to achieve better therapeutic effect with minimized pain. This study aimed to evaluate the effect and safety by comedone extractor and ultra-pulse dynamic CO2 laser in the treatment of dense comedones.
Materials and methods
Study design
This is an 8-week, prospective, split-face, randomized, and evaluator-blind trial. The study was conducted at the Dermatology Department of the Second Affiliated Hospital of Xi’an Jiao Tong University from November 2021 to March 2023. Written informed consents were obtained from all subjects before enrollment. All of the collected information was kept confidential and analyzed without specific names. This research was approved by the Research Council with the ethics code number MR-61-23-009891.
Sample size estimation was calculated based on the preliminary experiment, where the mean reduction rate of the extractor-treated side was set as 50%, and that of the laser-treated side would be about 86%, the sample size was 22 when the power is 80% and the 2-sided alpha is 0.05 after putting them into the formula [18]. A total of 25 patients are needed at a 10% dropout rate.
Patients’ selection
Eligible patients were males and nonpregnant females, with ≥100 comedones distributed symmetrically on the face and <10 inflammatory papules or pustules. A history of medication for comedones in the last 3 months, having experienced of sustained increase in surface scars after wound healing, having keloids, active cutaneous infections, and suffering other facial skin diseases that may influence the result were additional criteria for exclusion.
Treatment protocols
One side of the face was treated by the comedone extractor, while the other side received CO2 laser treatment. The CO2 laser-treated side was randomly determined by the selection system when the patient enrolled. Specifically, odd numbers represented the left side and even numbers represented the right. Before starting the operation, the patients’ faces were cleaned with alcohol, and their eyes were covered with damp gauze. No anesthesia was required. Each treatment of CO2 laser and comedone extractor is operated by two regular dermatologists, and the treatment area covers all comedones.
The test side was treated with the CO2 laser (CO2 Surgical Laser System, eCO2 Plus, Lutronic, Ilsan, Korea) with the following parameter: operation mode: Dynamic; scan type: Point; spot diameter: 120μm; pulse energy: 50-60mJ; pulse rate: 20Hz; power: 40w. The endpoint reaction is the appearance of a lipid filament or a slit.
The control side was treated with a comedone extractor consisting of a needle at one end with a 5-mm diameter ring on the opposite end. Firstly, the surface of the comedone should be pierced with the pointed end at an angle of about 45°, and then the ring is used to apply mild to moderate vertical pressure around the comedones till the contents are forced out [19].
Post-treatment care
Patients treated by CO2 laser were instructed not to wash their face after the operation till the scabs fell off. Patients were told to record the side effects such as erythema and skin sensitivity, and contact us in time if there was any discomfort. We advised them to pay attention to sun protection and avoid heat exposure and sweat for at least 2 weeks.
Assessments
All patients were photographed before each treatment at 0w (baseline), 2w, 4w, and 6w, respectively, and 2 weeks after the last treatment (8w) by digital camera 700D (Canon, Tokyo, Japan) and VISIA 6.0 Complexion Analysis System (Canfield Scientific Inc, Fairfield, NJ, USA) with identical light and positions. Two independent dermatologists unaware of the treatment allocation counted comedones on each side of the face under the shadowless lamp. The mean reduction rate of comedones was calculated at each visit as (week of visit – week 0) / week 0 × 100%. The porphyrin index (PI), texture index (TI), and red zone (RZ) counted by VISIA automatically were recorded to evaluate the count of microcomedones, smoothness of facial skin, and the degree of inflammation [20].
Erythema index (EI), transepidermal water loss (TEWL), hydration index (HI), and melanin index (MI) were assessed with DermaLab® Combo (Cortex Technology, Hadsund, Denmark) at each visit and were compared by the average measurement of three times to evaluate the skin conditions.
The pain was assessed using an 11-point numerical rating scale (NRS) ranging from “0” (no pain) to “10” (worst pain) [21]. The score for the highest pain experienced during treatment was used for assessment. The difference was obtained by subtracting the pain scores of the two treatments.
Statistical analysis
Statistical analyses were performed by Statistical Package for Social Science (SPSS) statistical program version (23.0). Because it was a split-face trial, the variance was homogeneous. Paired t-test was used when the data corresponded to the normal distribution, and Wilcoxon matched-pairs signed-rank test was employed when the data were not normally distributed. P < 0.05 wass considered statistically significant. Quantitative data were statistically represented in terms of range and standard deviation (SD) or standard error of mean (SEM).
Results
Patients
25 patients were recruited in the study, while 1 dropped out before the last laser session due to inability to follow the treatment schedule (Fig. 1), ultimately 24 completed the trial. 15 participants were female (62.5%), and 9 were male (37.5%). The average age of patients was 24.17 (± 5.05) years. 11 (45.83%) participants had Fitzpatrick skin type III, 7 (29.17%) participants had Fitzpatrick skin type II, and 6 (25%) had skin type IV. Demographic data were summarized in Table 1.
Decrease of comedones
At the baseline (0w) before all treatments, there was no difference in the number of comedones between the two sides of the face (P = .652). Comedones were reduced on both the CO2 laser-treated side and extractor-treated side after each treatment, while the reduction rate of the CO2 laser-treated side was higher than the extractor-treated side. The differences between the two sides were appeared since the second treatment (P = .034), and was accreted along the treatments. After four treatments, the mean reduction rate on the CO2 laser-treated side was 64.49%, and 46.36% on the extractor-treated side (P < .001, Fig. 2A, C, and D).
(A) The changes in the mean comedone reduction rate of the two groups with time (n = 24). (B) The proportion of participants at different reduction rate ranks of the two treatments after each treatment (n = 24). (C) Local comedones on the forehead of an 11-year-old female: before treatment (above), after 4 treatments (below); CO2 laser-treated side (left side), extractor-treated side (right side). After 4 treatments, comedones on the CO2 laser-treated side were almost gone, while comedones on the extractor-treated side had decreased but were still quite a few. (D) Representative VISIA images with Texture Mask before (above) and after treatments (below) of a 22-year-old female. The part protruding the skin (yellow dots) on the CO2 laser-treated side has decreased more significantly, indicating a greater reduction of comedones. The data shown are Mean (± SD). *p<0.05, **p<0.01.*** p<0.001
The comedone reduction rate was categorized into four grades: 0-25%, 25-50%, 50-75%, and 75-100%. After four treatments, for the CO2 laser-treated side, the proportion whose reduction rate reached 50% or more was 79.16%, with 33.33% greater than or equal to 75% (Fig. 2B, C, and D). In contrast, on the extractor-treated side, the proportion whose reduction rate was 50% or more was slightly lower at 37.5%, and only 4.17% reached 75% or more.
Other Efficacy Assessments
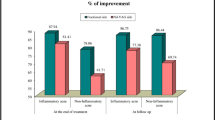
Before all treatments (baseline), TI (P = .805), PI (P = .483), RZ (P = .318), and EI (P = .115), of the two sides didn’t show differences. The mean TI reduced more in the CO2 laser-treated side (from 1438.74 ± 167.38 to 1204.48 ± 124.22, P = .02) than the extractor-treated side (from 1443.74 ± 166.32 to 1295.65 ± 132.44, P = .04) After 4 treatments, there were significantly difference between two sides (P = .029; Fig. 3A). The mean PI of both sides got lower markedly – PI of the CO2 laser-treated side reduced from 1746.83 ± 146.96 to 1283.57 ± 117.74 (P = .002) and extractor-treated side reduced from 1732.30 ± 152.01 to 1403.22 ± 130.71 (P = .033) after four treatments, thus, the difference was significant between two sides (P = .032, Fig. 3B). The mean RZ of the CO2 laser side reduced from 176.22 ± 14.53 to 156.69 ± 13.42 (P = .001), while the extractor-treated side reduced from 182.09 ± 14.42 to 169.30 ± 12.31 (P = .03) (Pbetween = .02; Fig. 3C). Similarly, EI was reduced on both sides, from 17.24 ± 0.62 to 15.85 ± 0.58 on the CO2 laser-treated side (P < .001), and from 17.51 ± 0.59 to 16.54 ± 0.59 on the extractor-treated side (P = .003). Therefore, there was a statistically significant difference between the two sides (P = .011; Fig. 3D).
Before all treatments, TEWL (P = .207), HI (P = .26), and MI (P = .831) of the two sides didn’t show differences. After four treatments, TEWL on both sides significantly reduced (CO2 laser: from 23.02 ± 1.30 to 21.47 ± 1.31, P = .022; extractor: from 23.26 ± 1.28 to 21.59 ± 1.37, P = .026; Fig. 4A). In terms of HI and MI, neither the CO2 laser-treated side nor the extractor-treated side showed differences within or between groups (Fig. 4B and C).
Pain Score
The pain of both treatment methods was tolerable. Topical or local anesthetics were not used. With the times of treatments increases, the pain scores of both treatments decreased slightly (CO2 laser: from 5.22 ± 1.29 to 4.50 ± 1.26, P < .001; extractor: from 8.00 ± 0.89 to 7.46 ±0.87, P < .001). The difference in pain scores between the two treatments was significant for each treatment (P < .001), and the D-value was 2.76-2.96 (Fig. 5).
The pain scores were recorded using the maximum pain experienced during the treatment period ranging from “0” (no pain) to “10” (worst pain) according to the pain numerical rating scale (NRS). The gray shaded area is the difference between the two treatments. The data shown are Mean ± SD. *p<0.05, **p<0.01.*** p<0.001. w, week
Side effects
Side effects were recorded in both CO2 laser and comedone extractor groups. For 4 treatment sessions with 24 patients, a sum of 96 timepoints was recorded (Table 2).
For CO2 laser-related side effects (Table 2, upper), side effects mainly appeared as scabs, the severity of which depends on the severity of the comedone. Approximately 21.88% of cases were mild scabbing, 20.83% were moderate, and 57.29% were severe. Immediately after CO2 laser treatment, the incidence of small urticarial response at the treated spot was 82.29% (mild: 54.17%, moderate: 28.12%), but subsided within a few hours. Transient erythema occurred three times (occurrence rate: 3.12%) after the CO2 laser, hyperpigmentation was observed only once (occurrence rate: 1.04%), and both of which vanished in 14 days. No skin sensitivity, hypertrophic scar, or keloids occurred after CO2 laser treatment.
The main side effect associated with the comedone extractor was bleeding (Table 2, below), which occurred in all patients postoperation (mild: 78.13%, moderate: 12.50%, severe: 9.37%), and all stopped bleeding within half an hour by pressing or without treatment. Transient erythema occurred about 51.04% immediately after comedone extraction (mild: 28.12%, moderate: 22.92%), and all faded away gradually in 72 hours. Two patients were observed hyperpigmentation because of comedone extraction (occurrence rate: 2.08%), and it vanished in 14 days. Same as the CO2 laser, no skin sensitivity, hypertrophic scar, or keloids occurred after comedone extraction.
Discussion
In this study, we demonstrate that the efficacy of the ultra-pulse dynamic CO2 laser has higher treatment efficacy in the clearance of comedone higher than the comedone extractor. After 4 treatments, 79.16% of patients showed 50% comedone reduction, and the mean reduction rate by CO2 laser was 64.49%. TI, PI, RZ, and EI decreased more on the CO2 laser-treated side, indicating that the improvement of skin smoothness, reduction of micro comedones, and reduction in the area and degree of skin inflammation were more obvious when treated with CO2 laser.
The comedone extractor can remove excess sebum, keratin, and hyperproliferative funnel keratin-forming cells by puncturing the epidermis with a needle at one end and squeezing with a ring at the other. The simplicity of operation and low price makes it a widely used tool in clinical practice. However, it’s difficult for operators to control the intensity to attend sufficient pressure, especially the inexperienced operators. Moreover, the comedone extractor might cause incomplete stripping of sebum, which serves as a substrate for the growth of bacteria and other microorganisms, contributing to the progression of comedone [22]. Besides, the extraction treatment could only focus on the comedones that already appeared on the epidermis, but cannot prevent or provide deeper treatment.
The CO2 laser, by contrast, makes up for these shortcomings. Firstly, the ultra-pulsed CO2 laser in the dynamic mode could target the comedones accurately. On the one hand, the photomechanical effects of the CO2 laser can damage abnormal keratin, on the other hand, it helps to remodel the epithelium, normalizing the newborn epidermis [14, 23]. Secondly, the selective photothermal effect of CO2 laser makes the content of comedone vaporize into lipid filaments or solidify into particles, which are then discharged through the open epidermal channels created by the CO2 laser [14, 24]. The heat will also be transmitted to the surroundings of SGs, which makes SGs shrink and sebum production decrease [25]. Thirdly, the CO2 laser has antibacterial and anti-inflammatory effects. The laser-generated shockwave could kill bacteria and fracture the biofilm [26, 27], achieving the antibacterial effect. Previous studies found the reduction of TNF-α and IFN-γ after laser treatment illustrating the anti-inflammatory effect [28].
The alleviation of inflammation may be due to the involvement of inflammatory factors and bacterial proliferation in the comedone stage, and the process of treating comedone is also a process of reducing inflammation and preventing the further development of inflammatory acne lesions [29, 30]. The decrease of TEWL indicates the repair of skin barrier function after treatment, which may indicate the possible potential relationship between dense comedones and the skin barrier, but it’s unknown which happened first. We speculate that the disruption of the skin barrier was one of the seeds for dense comedones, and the progression of comedones further aggravated the disruption of the skin barrier [31]. There was no significant change in HI and MI, demonstrating the safety of the two treatments. The pain caused by CO2 laser is much less than that caused by the comedone extractor, and the difference is statistically and clinically significant, as the minimal clinically important difference of the pain NRS was defined as two units [32]. We believe that treating comedone with the CO2 laser instead of the traditional comedone extractor could relieve the pain. As for the difference among times of treatment, it may be related to the comedone amount, which is only statistically but not clinically significant. No permanent or severe side effects were observed on either side. For the urticarial response caused by the CO2 laser, the patients had no discomfort such as pain or itching, and these reactions faded spontaneously within an hour without leaving any traces. As for the transient erythema and hyperpigmentation caused by CO2 laser or extraction, they all disappeared within 14 days, and no patients left erythema or pigmentation at the last follow-up.
Compared with traditional comedone extractors, the ultra-pulse dynamic CO2 laser exhibits a higher clearance rate and lower pain scores for treating dense comedones. The high precision and strong penetration of CO2 laser make the treatment not only limited to the surface of the skin but can penetrate deep into the skin, treating and preventing comedones from the root. The CO2 laser could also stop bleeding during treatment, reducing the risk of infection and bleeding. For clinicians, easier handling and lower price (requiring no consumables) are advantages of the CO2 laser. However, the longer-term effect results in a longer recovery period CO2 laser has scab-forming and shedding phase.
Conclusion
Both CO2 laser and comedone extractor are effective in the treatement of comedones, while CO2 laser showed higher comedone clearance with lower pain than the comedone extractor. Both treatments didn’t show severe and permanent side effects.
Limitations
A longer-term follow-up and larger-size subjects are needed. Moreover, there is a lack of comparison between the efficacy of different form of comedone.
Data Availability
Other scholars and readers could contact the corresponding authors for the detailed data.
Abbreviations
- AV:
-
acne vulgaris
- CO2 :
-
carbon dioxide
- SG:
-
sebaceous glands
- TI:
-
texture index
- PI:
-
porphyrin index
- RZ:
-
red zone
- EI:
-
erythema index
- TEWL:
-
transepidermal water loss
- HI:
-
hydration index
- MI:
-
melanin index
- NRS:
-
numerical rating scale
- w:
-
weeks
References
Clayton RW, Gobel K, Niessen CM, Paus R, van Steensel MAM, Lim X (Oct 2019) Homeostasis of the sebaceous gland and mechanisms of acne pathogenesis. Br J Dermatol 181(4):677–690. https://doi.org/10.1111/bjd.17981
Knutson DD (Mar 1974) Ultrastructural observations in acne vulgaris: the normal sebaceous follicle and acne lesions. J Invest Dermatol 62(3):288–307. https://doi.org/10.1111/1523-1747.ep12676804
Cunliffe WJ, Holland DB, Jeremy A (Sep-Oct 2004) Comedone formation: etiology, clinical presentation, and treatment. Clin Dermatol 22(5):367–374. https://doi.org/10.1016/j.clindermatol.2004.03.011
Witkowski JA, Parish LC (Sep-Oct 2004) The assessment of acne: an evaluation of grading and lesion counting in the measurement of acne. Clin Dermatol 22(5):394–397. https://doi.org/10.1016/j.clindermatol.2004.03.008
Burkhart CG, Burkhart CN (Oct 2007) Expanding the microcomedone theory and acne therapeutics: Propionibacterium acnes biofilm produces biological glue that holds corneocytes together to form plug. J Am Acad Dermatol 57(4):722–724. https://doi.org/10.1016/j.jaad.2007.05.013
Common JEA, Barker JN, van Steensel MAM (Oct 2019) What does acne genetics teach us about disease pathogenesis? Br J Dermatol 181(4):665–676. https://doi.org/10.1111/bjd.17721
Do TT, Zarkhin S, Orringer JS et al (Apr 2008) Computer-assisted alignment and tracking of acne lesions indicate that most inflammatory lesions arise from comedones and de novo. J Am Acad Dermatol 58(4):603–608. https://doi.org/10.1016/j.jaad.2007.12.024
Leyden JJ (Sep 2003) A review of the use of combination therapies for the treatment of acne vulgaris. J Am Acad Dermatol 49(3 Suppl):S200–S210. https://doi.org/10.1067/s0190-9622(03)01154-x
Shalita A, Weiss JS, Chalker DK et al (Mar 1996) A comparison of the efficacy and safety of adapalene gel 0.1% and tretinoin gel 0.025% in the treatment of acne vulgaris: a multicenter trial. J Am Acad Dermatol 34(3):482–485. https://doi.org/10.1016/s0190-9622(96)90443-0
Bagatin E, Costa CS (Aug 2020) The use of isotretinoin for acne - an update on optimal dosing, surveillance, and adverse effects. Expert Rev Clin Pharmacol 13(8):885–897. https://doi.org/10.1080/17512433.2020.1796637
Ochsendorf F (2015) Clindamycin phosphate 1.2% / tretinoin 0.025%: a novel fixed-dose combination treatment for acne vulgaris. J Eur Acad Dermatol Venereol (29 Suppl 5):8–13. https://doi.org/10.1111/jdv.13185
Parish L (1994) Historical aspects of cutaneous surgery. In: Cutaneous Surgery Philadelphia. WB Saunders, pp 4–5
Mukhtar M, Sharma R (Dec 2004) Surgical pearl: the safety pin as a better alternative to the versatile paper clip comedo extractor. Int J Dermatol 43(12):967–968. https://doi.org/10.1111/j.1365-4632.2004.02293.x
Omi T, Numano K (2014) The Role of the CO2 Laser and Fractional CO2 Laser in Dermatology. Laser Ther 23(1):49–60. https://doi.org/10.5978/islsm.14-RE-01
Lim EH, Seo YJ, Lee JH, Im M (Dec 2013) Onychodystrophy treated using fractional carbon dioxide laser therapy and topical steroids: new treatment options for nail dystrophy. Dermatol Surg 39(12):1931–1933. https://doi.org/10.1111/dsu.12365
Karsai S, Czarnecka A, Junger M, Raulin C (Feb 2010) Ablative fractional lasers (CO(2) and Er:YAG): a randomized controlled double-blind split-face trial of the treatment of peri-orbital rhytides. Lasers Surg Med 42(2):160–167. https://doi.org/10.1002/lsm.20879
Vrijman C, van Drooge AM, Limpens J et al (Nov 2011) Laser and intense pulsed light therapy for the treatment of hypertrophic scars: a systematic review. Br J Dermatol 165(5):934–942. https://doi.org/10.1111/j.1365-2133.2011.10492.x
Eng J (May 2003) Sample size estimation: how many individuals should be studied? Radiology 227(2):309–313. https://doi.org/10.1148/radiol.2272012051
Fox L, Csongradi C, Aucamp M, du Plessis J, Gerber M (2016) Treatment Modalities for Acne. Molecules 21(8). https://doi.org/10.3390/molecules21081063
Patwardhan SV, Richter C, Vogt A, Blume-Peytavi U, Canfield D, Kottner J (Apr 2017) Measuring acne using Coproporphyrin III, Protoporphyrin IX, and lesion-specific inflammation: an exploratory study. Arch Dermatol Res 309(3):159–167. https://doi.org/10.1007/s00403-017-1718-3
Hawker GA, Mian S, Kendzerska T, French M (Nov 2011) Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken) 63(Suppl 11):S240–S252. https://doi.org/10.1002/acr.20543
Xu H, Li H (Jun 2019) Acne, the Skin Microbiome, and Antibiotic Treatment. Am J Clin Dermatol 20(3):335–344. https://doi.org/10.1007/s40257-018-00417-3
Hantash BM, Bedi VP, Kapadia B et al (Feb 2007) In vivo histological evaluation of a novel ablative fractional resurfacing device. Lasers Surg Med 39(2):96–107. https://doi.org/10.1002/lsm.20468
Eberhardt H (1975) Comedo formation in acne. Arch Dermatol Res 254(3):257–262. https://doi.org/10.1007/BF00557967
Moneib H, Tawfik AA, Youssef SS, Fawzy MM (Nov 2014) Randomized split-face controlled study to evaluate 1550-nm fractionated erbium glass laser for treatment of acne vulgaris--an image analysis evaluation. Dermatol Surg 40(11):1191–1200. https://doi.org/10.1097/DSS.0000000000000167
Sol A, Feuerstein O, Featherstone JD, Steinberg D (2011) Effect of sublethal CO2 laser irradiation on gene expression of streptococcus mutans immobilized in a biofilm. Caries Res 45(4):361–369. https://doi.org/10.1159/000329390
Francis NC, Yao W, Grundfest WS, Taylor ZD (Apr 2017) Laser-Generated Shockwaves as a Treatment to Reduce Bacterial Load and Disrupt Biofilm. IEEE Trans Biomed Eng 64(4):882–889. https://doi.org/10.1109/TBME.2016.2581778
Fukuda TY, Tanji MM, Silva SR, Sato MN, Plapler H (Sep 2013) Infrared low-level diode laser on inflammatory process modulation in mice: pro- and anti-inflammatory cytokines. Lasers Med Sci 28(5):1305–1313. https://doi.org/10.1007/s10103-012-1231-z
Jeremy AH, Holland DB, Roberts SG, Thomson KF, Cunliffe WJ (Jul 2003) Inflammatory events are involved in acne lesion initiation. J Invest Dermatol 121(1):20–27. https://doi.org/10.1046/j.1523-1747.2003.12321.x
Saurat JH (2015) Strategic Targets in Acne: The Comedone Switch in Question. Dermatology 231(2):105–111. https://doi.org/10.1159/000382031
Dull K, Lenart K, Dajnoki Z et al (Jul 2023) Barrier function-related genes and proteins have an altered expression in acne-involved skin. J Eur Acad Dermatol Venereol 37(7):1415–1425. https://doi.org/10.1111/jdv.19062
Tu JF, Yang JW, Lin LL et al (2019) Efficacy of electro-acupuncture and manual acupuncture versus sham acupuncture for knee osteoarthritis: study protocol for a randomised controlled trial. Trials 20(1):79. https://doi.org/10.1186/s13063-018-3138-x
Funding
This work was funded by the Natural Science Basic Research Program of Shaanxi (2023-JC-YB-787) to Weihui Zeng. National Natural Science Foundation of China (NSFC) (82201966) and Natural Science Basic Research Program of Shaanxi (2023JC-QN-0924) to Zhao Wang.
Author information
Authors and Affiliations
Contributions
Meng-yao yang designed research, performed research, and wrote the original draft; Si-meng Qiao collected the data and prepared the resources;Di-chao Ning analyzed the data and performed the validation; Yi-hao Ding collected the data; Wei-Hui Zeng supervised the experiment and provided funding; Zhao Wang reviewed and edited the draft and provided funding.
Corresponding authors
Ethics declarations
IRB approval status
Reviewed and approved by the Second Affiliated Hospital of Xi’an Jiao Tong University IRB; approval #2022235. Clinicaltrials.gov listing: MR-61-23-009891
Consent for the publication
Consent for the publication of recognizable patient photographs or other identifiable material was obtained by the authors and included at the time of article submission to the journal stating that all patients gave consent with the understanding that this information may be publicly available.
Conflicts of interest
None declared.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Limitations
Short-term follow-up and limited sample size restricted us from drawing further conclusions.
Supplementary information
ESM 1
(XLSX 16 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, My., Qiao, Sm., Ning, Dc. et al. Treatment effect of ultra-pulse dynamic CO2 laser and comedone extractor in dense comedones: a prospective, randomized, split-face, evaluator-blind, controlled clinical trial. Lasers Med Sci 39, 233 (2024). https://doi.org/10.1007/s10103-024-04104-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10103-024-04104-0