Abstract
The thulium laser resection of bladder tumor (TmLRBT) is widely used in the treatment of non-muscle-invasive bladder cancer (NMIBC), and we conduct this study to compare the safety and efficacy of TmLRBT with transurethral resection of bladder tumor (TURBT). A comprehensive literature research was conducted using multiple databases, and comparative studies evaluating the safety and efficacy of TmLRBT and TURBT were included. For continuous outcomes, the weighted mean difference (WMD) was used to measure the difference, whereas the risk ratio (RR) with a 95% confidence interval (CI) was calculated for binary variables. Overall, ten studies with 1558 patients enrolled were included in the meta-analysis. The baseline characteristics of two groups were comparable. The operative time (p = 0.24) and catheterization time (p = 0.41) of two groups were similar but the TmLRBT group had a shorter length of hospital stay (p = 0.04). TmLRBT was related to fewer intraoperative complications including obturator nerve reflex (p < 0.001) and bladder perforation (p < 0.001). Although the rate of postoperative irrigation did not significantly differ in our analysis (p = 0.28), the TmLRBT was related to a significantly shorter duration of irrigation (p = 0.004). Besides, the TmLRBT group had a higher rate of identification of detrusor (p = 0.02). However, TmLRBT did not suggest significantly better cancer control than TURBT including the overall recurrence (p = 0.052), 1-year recurrence (p = 0.23), and 2-year recurrence (p = 0.40). Compared with conventional TURBT, the TmLRBT showed superior safety and non-inferior efficacy in cancer control. TmLRBT could also provide high-quality specimens for pathology diagnosis; therefore, it is an as effective option for NMIBC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bladder cancer is one of the most common urological malignant diseases worldwide with high recurrence and progression rates [1]. According to the depth of invasion, bladder cancer was divided into non-muscle-invasive bladder cancer (NMIBC) and muscle-invasive bladder cancer. NMIBC is defined as the tumor that is confined to the mucosa (Ta, Tis) or submucosa (T1) of the bladder, and approximately 75% of newly diagnosed bladder cancer is NMIBC [2].
The conventional transurethral resection of bladder tumor (TURBT) combined with adjuvant therapy was the primary treatment recommended for NMIBC [3]. However, the TURBT was associated with several complications including obturator nerve reflex, bladder perforation, and postoperative bleeding. To overcome these drawbacks, lasers such as holmium YAG and thulium YAG were introduced to the resection of bladder tumors and they showed advantages in tissue cutting, vaporization, and hemostasis.
Holmium laser was first used by urologists in the early 1990s [4, 5], and it had suggested non-inferior or even better safety and efficacy compared with TURBT [6]. As the latest innovation, the thulium laser was firstly applied in urological practice in 2005 [7, 8]. Compared with holmium laser, the depth penetration in water is decreased, and unlike the tearing action on tissue by pulsed emission of holmium laser, the continuous wave output of thulium laser allows smooth incision, which makes the en bloc resection more practicable, and vaporization of tissue with excellent hemostasis [9, 10].
Several studies reported the safety and efficacy of thulium laser resection of bladder tumor (TmLRBT), and as one of the largest centers of urologic holmium laser and thulium laser therapy in China, we also had some experience in the urologic laser treatment in our clinical practice. Therefore, we performed this systematic review and meta-analysis to compare TmLRBT with conventional TURBT and determine whether TmLRBT could be a superior option.
Methods
This systematic review and meta-analysis was prospectively registered on PROSPERO (CRD42020184718), and it was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement [11].
Literature search
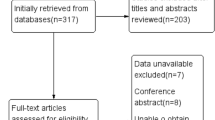
A comprehensive literature search was conducted for studies published from the inception of databases to May 8, 2020, in PubMed, Web of Science, and Scopus to identify studies comparing TmLRBT to conventional TURBT.
Separate searches were carried out using keywords including “laser”, “continuous wave”, “Thulium”, “Vela”, and “bladder cancer”. The detailed search string was previously uploaded on PROSPERO. Comparative studies that compared TmLRBT with TURBT were included, and the single-arm studies were excluded. Reviews, editorials, meeting abstracts, and other studies without original data were also excluded.
Titles and abstracts of articles identified by the keyword search were screened against the study selection criteria. Potentially relevant articles were evaluated of the full text. An additional manual search of references from identified studies was performed. Two independent reviewers screened all studies according to inclusion and exclusion criteria, and all disagreements were resolved by discussion with a third author.
Data extraction and quality assessment
Two reviewers independently extracted data from every study and evaluated methodological quality. The following information was extracted from each study: study design; origin of study; number of cases; proportion of gender; age; tumor size; tumor multiplicity; tumor location; T stage; pathological grade; adjuvant therapy; perioperative data including operation time, catheterization time, length of hospital stay, and complications; recurrence at different time points.
The quality of included randomized controlled studies (RCT) was assessed with the revised Cochrane risk of bias (RoB 2) tool [12], while the quality of non-randomized studies was determined using the ROBINS-I tool, a tool recommended by Cochrane for assessing the risk of bias in non-randomized studies of interventions [13]. The graphs for the risk of bias were generated with the robvis tool [14].
Data analysis
A formal meta-analysis of studies comparing the perioperative parameters and safety of TmLRBT and TURBT for NMIBC was performed. The recurrence of these two surgeries was also compared to assess efficacy. Besides, a subgroup analysis of the rate of recurrence of different periods was performed.
For outcomes of continuous variables, the weighted mean difference (WMD) was used to measure the difference, whereas the risk ratio (RR) with a 95% confidence interval (CI) was calculated for binary variables.
A fixed-effects model was used to calculate the pooled estimates if no significant heterogeneity was identified (I2 < 50%). Otherwise, a random-effects model was used. Additionally, a sensitivity analysis was also performed by changing the effect model. Due to the limited number of included studies, the publication bias was evaluated by using Egger’s linear regression test. All statistical analyses were performed by using Review Manager 5.3 (Cochrane Collaboration, Oxford, UK), except for the calculation of Egger’s linear regression test, which was conducted in STATA version 12.0 (Stata Corp, College Station, TX).
Results
Characteristics of included studies
Overall, ten studies involving 1558 patients were included in the meta-analysis after screening [15,16,17,18,19,20,21,22,23,24] (Fig. 1), and the characteristics of the included studies are listed in Table 1. Most studies were originated from China except for one study from Italy and one from Russia. Among the ten included studies, four studies were RCTs, and five studies were of retrospective design, and one study was a prospective cohort with historical control. As for the postoperative intravesical instilled chemotherapy, epirubicin, pirarubicin, and mitomycin were used in these included studies. Two studies were published in Chinese, and one study was published in Russian, but all of them had an English abstract [17, 19, 24].
The quality of RCTs was assessed using the RoB 2 tool, and Zhang et al.’s study [22] had a higher risk of bias due to the randomization and allocation procedures and the analysis of complications (Supplement Figure 1). Non-randomized studies were evaluated using the ROBINS-I tool and the use of historical control resulted in a higher risk of bias in Migliari et al.’s study [20] (Supplement Figure 2).
The baseline characteristics of the TmLRBT group and the TURBT group were compared, and no significant difference was detected in age (p = 0.91), proportion of gender (p = 0.87), tumor size (p = 0.06), tumor location (p = 0.76), and tumor multiplicity (p = 0.90). After a postoperative pathological evaluation, the pathological grades were similar between two groups (p = 0.14) while the TmLRBT group had more T1 tumors than the TURBT group regarding the T stage (p = 0.009).
Perioperative outcomes
Two groups were similar in operative time (WMD 2.41 min, 95%CI [− 1.65, 6.46]; p = 0.24) and postoperative catheterization time (WMD − 0.31 d, 95%CI [− 1.04, 0.42]; p = 0.41), but the TmLRBT group had a shorter length of hospital stay (WMD − 0.58 d, 95%CI [− 1.14, − 0.02]; p = 0.04; Fig. 2).
The TmLRBT was superior regarding safety during surgery without obturator nerve reflex (RR 0.04, 95%CI [0.02, 0.12]; p < 0.001) and bladder perforation (RR 0.11, 95%CI [0.04, 0.35]; p < 0.001; Fig. 3) compared with TURBT. After the resection of bladder tumors, the pathological assessment was conducted. The identification rate of detrusor was significantly lower in the TURBT group (RR 0.84, 95%CI [0.72, 0.97]; p = 0.02). Although the rate of postoperative irrigation did not significantly differ in our analysis (RR 0.60, 95%CI [0.24, 1.50]; p = 0.28), the TmLRBT was related to a significantly shorter duration of irrigation (WMD − 7.91 h, 95%CI [− 13.25, − 2.58]; p = 0.004; Fig. 4).
Recurrence
All patients were followed up for 12–36 months after surgery, and there was no significant difference in the overall recurrence rate during the follow-up in the TmLRBT group and TURBT group (RR 0.678, 95%CI [0.458, 1.003]; p = 0.052; Fig. 5). Recurrence at different points of time was also compared, and there was also no difference in 1-year recurrence (RR 0.68, 95%CI [0.36, 1.28]; p = 0.23) and 2-year recurrence (RR 0.82, 95%CI [0.52, 1.30]; p = 0.40).
Publication bias and sensitivity analysis
Publication bias was assessed using Egger’s test, and the results are listed in Table 2. The analysis of bladder perforation and 2-year recurrence rate suggested significant bias. The result of bladder perforation analysis was consistent with the initial result after excluding the biased studies.
Sensitivity analyses were conducted by changing the effect model, and results are summarized in Table 2. The inconsistent results in catheterization time, irrigation rate, overall recurrence, and 1-year recurrence suggested weak robustness of these analyses, and they should be cautiously interpreted.
Discussion
TURBT is commonly used in the diagnosis and treatment of primary NMIBC, but the occurrence of obturator nerve reflex during surgery, especially for lesions located in the lateral bladder wall, is inevitable, even under the transperineal obturator nerve block [25]. On the other hand, TURBT is not efficient enough in the hemostasis and the postoperative bleedings are frequent and even a second surgery is required to control the blood loss in some cases. Fortunately, the application of lasers efficiently solved these problems, and the less thermal injuries and safe penetration depth made thulium laser a feasible tool for enucleation.
In our analysis, the operation time and catheterization time were similar between two groups, but the TmLRBT was related to a shorter length of hospital stay. Theoretically, the TmLRBT could reduce the thermal injury and therefore shorten the catheterization duration, but our analysis did not suggest a significant advantage. However, considering the instability of the catheterization time analysis in the sensitivity analysis, whether the TmLRBT could reduce the catheterization still needs to be ascertained in future studies.
The hospital stay duration is shorter in the TmLRBT group (WMD − 0.58 days, 95%CI [− 1.14, − 0.02]; p = 0.04). It might infer that the TmLRBT could bring better postoperative recovery. However, it should be noted that the hospital stay duration greatly varied between different studies. In clinical practice, the length of hospital stay depends on more than the patients’ situation, but also could be influenced by parameters such as the local policies and surgeon’s habit. Therefore, the hospital stay might not be a strong surrogate to assess the postoperative performance of surgery and this result should be interpreted with caution.
The main strength of TmLRBT is the fewer complications during surgery, and in our analysis, the obturator nerve reflex and bladder perforation did not occur in the TmLRBT group. The bladder perforation is the most serious complication of TURBT, and obturator nerve reflex and the thermal injury might be important causes. During the TURBT procedure, the current flow passing through may stimulate the obturator nerve, which results in muscle contraction and bladder perforation. In contrast, no current flow was produced during the TmLRBT and the perforation caused by obturator nerve reflex could be avoided. The high temperature ranged from 100 to 300 °C at the treatment site during the TURBT is another cause of perforation. In the TmLRBT, the central part of the exposed tissue could be heated to a temperature as high as 90 to 100 °C, which caused the tissue vaporization, and the tissue adjacent to the vaporized part could be coagulated under a temperature of 60 to 80 °C. Beneath the coagulation layer, the tissue temperature is around only 45 to 50 °C and the thermal injury is minimal [26].
In our analysis, the TmLRBT group had a higher identification rate of detrusor. First, the 0.2-mm tissue penetration depth and less thermal damage of TmLRBT resulted in a more precise cutting of tissue and the complete specimen could more easily be acquired. During the TURBT, the depth of resection might be compromised due to the risk of bladder perforation, which may lead to the absence of the detrusor. Besides, in the conventional TURBT, the resection of lesions was conducted in a “piece by piece” way, which resulted in poor specimen quality. The application of lasers made the en bloc resection more feasible, and the identification of detrusor could be more practicable.
The identification of detrusor is essential for accurate pathological assessment. Also, unlike the specimen of pieces during the TURBT, the en bloc resection made the pathological assessment much more convenient. Besides, even the detrusor was acquired, the thermal damage could also lead to poor specimen quality and made it hard to assess the cancer stage. When the specimen was not sufficient to confirm that cancer was confined to the submucosa, it could only be staged as Ta or Tis. These could be the reasons for the higher proportion of T1 tumors in the TmLRBT group.
Postoperative bleeding is another important complication after the resection of bladder tumors. During the TmLRBT, the tissue around the lesions was instantly coagulated and therefore might be more efficient in hemostasis. Due to constant irrigation during the resection surgeries, the estimation of blood loss was impracticable. Instead, the postoperative irrigation could be a simple parameter to assess the postoperative irrigation as the irrigation was commonly stopped if there were no signs of postoperative bleeding. In our analysis, the rate of postoperative irrigation was not significantly different between the two groups. In this analysis, only two studies were included and the limited number could be the reason for the insignificant result. On the other hand, the use of postoperative irrigation depended on the surgeon’s decision. For example, in Liu et al.’s study, postoperative irrigation was not applied for all patients; while in Xu et al.’s study, all patients received postoperative irrigation [19, 21]. But still, the shorter irrigation duration in our analysis suggested the less postoperative bleeding in the TmLRBT group. Besides, Zhang et al. [22] reported that two patients after TURBT extended postoperative irrigation due to bleeding, Migliari et al. [20] reported the endoscopic hemostasis in the TURBT group, Zhong et al. [23] reported the higher hemoglobin decrease in TURBT, and Liu et al. [19] reported the longer duration of gross hematuria after TURBT. All these findings supported the less risk of postoperative bleeding after TmLRBT.
In the conventional TURBT, the tumors are resected piece by piece, which is the contrast to any other neoplasms. The incomplete tumor resection may contribute to the recurrence of bladder tumors. The TURBT has been suggested to cause the spreading of tumor cells in the bladder and circulation [27, 28], which also might be a reason for the high recurrence rate and progression rate of bladder cancers. The en bloc technique used in the TmLRBT allows for the tumor to be entirely cut out, and the risk of dissemination is low. For these large tumors which need to be incised longitudinally, due to the coagulation layer beneath the vaporized part of tissues, the possibility of tumor cell seeding was also extremely low. In our analysis, the TmLRBT might be related to a lower overall recurrence rate, though not statistically significant (p = 0.052). Due to the limited number of included studies, the recurrence rate of the different periods also did not suggest significant results. Nevertheless, these results suggested the non-inferior cancer control of TmLRBT compared with TURBT. Well-designed prospective studies with large sample sizes are still warranted to ascertain the efficacy in cancer control of TmLRBT.
To the best of our knowledge, this is the first systematic review and meta-analysis to compare the TmLRBT and TURBT. We evaluated the perioperative parameters, intraoperative and postoperative complications, and long-term recurrence to assess the safety and efficacy of the TmLRBT. There were also several limitations in this study. First, the RCTs and non-randomized studies were mixed in our analysis; therefore, the reliability of outcomes might be compromised, and we were unable to perform an effective subgroup analysis to assess the effect of the study design. Second, due to the limited number and high heterogeneity of included studies, some results of our analysis, especially the recurrence outcomes, were not able to produce a reliable conclusion. Although there were 10 studies involving 1558 patients included in this study, only a subset of studies reported the outcomes for each variable compared. It should be noted that the sample size for each individual comparison is considerably smaller than the overall number of patients reported. Third, some important parameters, the postoperative bleeding, for example, were not well-documented in a standard way and we were unable to conduct a powerful quantitative analysis to assess the results. Well-designed prospective RCTs with large sample sizes are still warranted to determine the safety and efficacy of TmLRBT.
Conclusion
Compared with conventional TURBT, the TmLRBT showed superior safety with fewer intraoperative complications and less risk of postoperative bleeding, and non-inferior efficacy in cancer control. TmLRBT could also provide high-quality specimens for accurate pathology diagnosis; therefore, it is an effective option for NMIBC. Whether TmLRBT can provide superior cancer control than TURBT remains to be ascertained by further studies.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Cumberbatch MGK, Jubber I, Black PC, Esperto F, Figueroa JD, Kamat AM et al (2018) Epidemiology of bladder cancer: a systematic review and contemporary update of risk factors in 2018. Eur Urol 74(6):784–795. https://doi.org/10.1016/j.eururo.2018.09.001
Babjuk M, Burger M, Compérat EM, Gontero P, Mostafid AH, Palou J et al (2019) European Association of Urology guidelines on non-muscle-invasive bladder cancer (TaT1 and Carcinoma In Situ)-2019 Update. Eur Urol 76(5):639–657. https://doi.org/10.1016/j.eururo.2019.08.016
Johnson DE, Cromeens DM, Price RE (1992) Use of the holmium:YAG laser in urology. Lasers Surg Med 12(4):353–363. https://doi.org/10.1002/lsm.1900120402
Johnson DE (1994) Use of the holmium:YAG (Ho:YAG) laser for treatment of superficial bladder carcinoma. Lasers Surg Med 14(3):213–218. https://doi.org/10.1002/lsm.1900140303
Li C, Gao L, Zhang J, Yang X, Liu C (2020) The effect of holmium laser resection versus standard transurethral resection on non-muscle-invasive bladder cancer: a systematic review and meta-analysis. Lasers Med Sci. https://doi.org/10.1007/s10103-020-02972-w
Xia SJ, Zhang YN, Lu J, Sun XW, Zhang J, Zhu YY et al (2005) Thulium laser resection of prostate-tangerine technique in treatment of benign prostate hyperplasia. Zhonghua Yi Xue Za Zhi 85(45):3225–3228
Gao X, Ren S, Xu C, Sun Y (2008) Thulium laser resection via a flexible cystoscope for recurrent non-muscle-invasive bladder cancer: initial clinical experience. BJU Int 102(9):1115–1118. https://doi.org/10.1111/j.1464-410X.2008.07814.x
Wendt-Nordahl G, Huckele S, Honeck P, Alken P, Knoll T, Michel MS et al (2008) Systematic evaluation of a recently introduced 2-microm continuous-wave thulium laser for vaporesection of the prostate. J Endourol 22(5):1041–1045. https://doi.org/10.1089/end.2007.0421
Bach T, Wendt-Nordahl G, Michel MS, Herrmann TR, Gross AJ (2009) Feasibility and efficacy of thulium:YAG laser enucleation (VapoEnucleation) of the prostate. World J Urol 27(4):541–545. https://doi.org/10.1007/s00345-008-0370-0
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898. https://doi.org/10.1136/bmj.l4898
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919. https://doi.org/10.1136/bmj.i4919
McGuinness LA, Higgins JPT (2021) Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods 12(1):55-61. https://doi.org/10.1002/jrsm.1411
Chen X, Liao J, Chen L, Qiu S, Mo C, Mao X et al (2015) En bloc transurethral resection with 2-micron continuous-wave laser for primary non-muscle-invasive bladder cancer: a randomized controlled trial. World J Urol 33(7):989–995. https://doi.org/10.1007/s00345-014-1342-1
Huang JH, Hu YY, Liu M, Wang GC, Peng B, Yao XD (2016) Comparative study of 2 um laser versus holmium laser for the resection of non-muscle invasive bladder cancer. Int J Clin Exp Med 9(12):23618–23623
Liao J, Chen X, Chen Z, Chen L, Li X, Chen J (2015) Feasibilty and safety of en bloc transurethral resection with thulium-Yag laser in the management of patients with non-muscle-invasive bladder cancer. Tumor 35(7):788–793
Liu H, Wu J, Xue S, Zhang Q, Ruan Y, Sun X et al (2013) Comparison of the safety and efficacy of conventional monopolar and 2-micron laser transurethral resection in the management of multiple nonmuscle-invasive bladder cancer. J Int Med Res 41(4):984–992. https://doi.org/10.1177/0300060513477001
Liu Y, Lu J, Xiao C (2013) Comparison between 2-mum continuous-wave thulium laser and transurethral resection for non-muscle-invasive bladder cancer: a retrospective comparative study. Chin J Minim Invasive Surg 13(1):23–28
Migliari R, Buffardi A, Ghabin H (2015) Thulium laser endoscopic en bloc enucleation of nonmuscle-invasive bladder cancer. J Endourol 29(11):1258–1262. https://doi.org/10.1089/end.2015.0336
Xu H, Ma J, Chen Z, Yang J, Yuan H, Wang T et al (2018) Safety and efficacy of en bloc transurethral resection with 1.9 microm vela laser for treatment of non-muscle-invasive bladder cancer. Urology 113:246–250. https://doi.org/10.1016/j.urology.2017.11.030
Zhang XR, Feng C, Zhu WD, Si JM, Gu BJ, Guo H et al (2015) Two micrometer continuous-wave thulium laser treating primary non-muscle-invasive bladder cancer: is it feasible? a randomized prospective study. Photomed Laser Surg 33(10):517–523. https://doi.org/10.1089/pho.2015.3913
Zhong C, Guo S, Tang Y, Xia S (2010) Clinical observation on 2 micron laser for non-muscle-invasive bladder tumor treatment: single-center experience. World J Urol 28(2):157–161. https://doi.org/10.1007/s00345-010-0532-8
Sorokin NI, Enikeev DV, Dymov AM, Tsarichenko DG, Kislyakov DA, Gololobov GY et al (2018) Safety and efficacy of thulium transurethral en block resection with fiber laser “Urlaz” for treatment of non-muscle-invasive bladder cancer. Onkourologiya 14(1):144–151. https://doi.org/10.17650/1726-9776-2018-14-1-144-151
Khorrami MH, Javid A, Saryazdi H, Javid M (2010) Transvesical blockade of the obturator nerve to prevent adductor contraction in transurethral bladder surgery. J Endourol 24(10):1651–1654. https://doi.org/10.1089/end.2009.0659
Liang JH, Pan YL, Kang J, Qi J (2012) Influence of irrigation on incision and coagulation of 2.0-μm continuous-wave laser: an ex vivo study. Surg Laparosc Endosc Percutan Tech 22(3):e122–e125. https://doi.org/10.1097/SLE.0b013e318248b69e
Hafner C, Knuechel R, Zanardo L, Dietmaier W, Blaszyk H, Cheville J et al (2001) Evidence for oligoclonality and tumor spread by intraluminal seeding in multifocal urothelial carcinomas of the upper and lower urinary tract. Oncogene 20(35):4910–4915. https://doi.org/10.1038/sj.onc.1204671
Blaschke S, Koenig F, Schostak M (2016) Hematogenous tumor cell spread following standard transurethral resection of bladder carcinoma. Eur Urol 70(3):544–545. https://doi.org/10.1016/j.eururo.2016.03.051
Funding
This work is supported by the Natural Science Fund of Hubei Province (Grant Number: 2018CFB459, Recipient: Dr. Heng Li).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Figure 1
Risk of bias graph of randomized studies assessed with the RoB 2 tool. (PNG 1033 kb).
Supplementary Figure 2
Risk of bias graph of non-randomized studies assessed with the ROBINS- I tool. (PNG 1018 kb).
ESM 3
(DOCX 29 kb).
Rights and permissions
About this article
Cite this article
Long, G., Zhang, Y., Sun, G. et al. Safety and efficacy of thulium laser resection of bladder tumors versus transurethral resection of bladder tumors: a systematic review and meta-analysis. Lasers Med Sci 36, 1807–1816 (2021). https://doi.org/10.1007/s10103-021-03272-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-021-03272-7