Abstract
Photodynamic therapy has been investigated as an alternative method of killing pathogens in response to the multiantibiotic resistance problem. This study evaluated the photodynamic effect of curcumin on methicillin-resistant Staphylococcus aureus (MRSA) compared to susceptible S. aureus (MSSA) and L929 fibroblasts. Suspensions of MSSA and MRSA were treated with different concentrations of curcumin and exposed to light-emitting diode (LED). Serial dilutions were obtained from each sample, and colony counts were quantified. For fibroblasts, the cell viability subsequent to the curcumin-mediated photodynamic therapy was evaluated using the MTT assay and morphological changes were assessed by SEM analysis. Curcumin concentrations ranging from 5.0 to 20.0 μM in combination with any tested LED fluences resulted in photokilling of MSSA. However, only the 20.0 μM concentration in combination with highest fluence resulted in photokilling of MRSA. This combination also promoted an 80% reduction in fibroblast cell metabolism and morphological changes were present, indicating that cell membrane was the main target of this phototherapy. The combination of curcumin with LED light caused photokilling of both S. aureus strains and may represent an alternative treatment for eradicating MRSA, responsible for significantly higher morbidity and mortality and increased healthcare costs in institutions and hospitals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Staphylococcus aureus, considered one of the most significant human pathogens, is commonly found in the oral environment [1]. Although the major reservoirs of S. aureus are the anterior nares, this organism has been isolated from 24% to 36% of healthy oral cavities. This incidence increases in the presence of prosthetic devices, reaching up to 48% in denture-wearing patients [2]. Furthermore, S. aureus strains have been found in different patient groups, such as children, elderly, and patients with systemic diseases and hematological malignancies [2]. Some oral infections are associated with S. aureus, such as angular cheilitis, endodontic infection, parotitis, and staphylococcal mucositis [2]. There is also scientific evidence that the oral cavity can be the source of the staphylococci responsible for infection at distant sites, such as aspiration pneumonia, endocarditis, acute septic arthritis, and chronic lung diseases [3].
As the oral cavity can be an important reservoir of this opportunistic pathogen, much effort has been made in order to promote the decolonization of Staphylococcus carriers [4]. However, the strategies to eliminate the S. aureus strains have been challenged with the development of antibiotic-resistant microorganisms, such as the methicillin-resistant S. aureus (MRSA). Strains of MRSA were first detected in 1961 and these pathogens are currently prevalent worldwide [5]. MRSA has become a major problem in nososcomial infections as it is responsible for significantly higher morbidity and mortality and increased healthcare costs [6]. It is known that the colonization precedes the systemic infection and therefore decolonization may reduce the risk of MRSA infection in individual carriers and prevent cross-infection to other patients or healthcare workers. Intranasal mupirocin, daily chlorhexidine body wash, antibiotics such as rifampin and doxycline, oral hygiene procedures, use of denture-cleansing agents and denture sterilization methods have been proposed to prevent colonization by MRSA and methicillin-susceptible S. aureus (MSSA) [6, 7]. However, a systematic review concluded that there is insufficient evidence to support the use of any topical or systemic antimicrobial therapy for eradicating MRSA [8].
The photodynamic therapy (PDT) has emerged in the clinical field as a potential alternative to antibiotics for inactivating resistant microorganisms using a non-toxic light-sensitive compound (known as photosensitizer—PS), visible light and oxygen. Briefly, activation of the PS by a visible light that matches its photophysical properties generates reactive oxygen species (ROS)-like free radicals by electron or hydrogen transfer (type I reaction) or reactive singlet oxygen by direct energy transfer to oxygen (type II reaction) [9]. Photodynamic inactivation of microorganisms has advantages, such as the local application of PS and light, which limits the action of ROS and avoids systemic effects on normal bacterial flora [10]. In addition, unlike antibiotics, which have a single target in the microbial cell, the reactive species generated by the photodynamic reaction have a multifunctional nature and can damage multiple cellular structures, reducing the chances of development of PDT-resistant strains [11]. Dovigo et al. [12] observed that fluconazole-resistant C. albicans and C. glabrata strains were sensitivity to PDT, although they were less susceptible than non-resistant strains. At the same time, however, this is a limitation of PDT because the host cells are also susceptible to the action of ROS. Ribeiro et al. [13] found that PDT caused severe toxic effects in normal cell culture, characterized by the reduction of the mitochondrial activity, morphological alterations and induction of necrotic cell death. Therefore, the challenge in PDT is to find a therapeutic window, as a function of the incubation time, PS concentration and applied light dose, in which bacteria can be killed without causing cytotoxic effects to the host’s surrounding healthy tissues [14].
Curcumin is a naturally occurring, intensely yellow pigment that is isolated from the rhizomes of the plant Curcuma longa (Linn) [15]. It is the active ingredient of the spice turmeric and is used worldwide as a cooking spice, flavoring agent and colorant [15]. Potential therapeutic applications of curcumin have been investigated due to its anti-inflammatory, antioxidant, antimicrobial, antitumor [15], and antifungal properties [16]. It has also been proposed that the beneficial effects of curcumin are enhanced in combination with light activation, which has stimulated researchers to explore the use of this pigment in several areas including photochemistry and photobiology [17]. In this scenario, it would be of interest to investigate the phototoxicity of curcumin against a pathogen that is a leading cause of bacterial diseases, including oral infections, in humans. The aim of this study was to evaluate the photodynamic effect of curcumin in combination with light-emitting diode (LED) light on MRSA and MSSA as well as its potential cytotoxic effects on L929 fibroblasts.
Material and methods
Microorganisms
The microorganisms used in this study were methicillin-susceptible (MSSA; ATCC 25923) and methicillin-resistant (MRSA; ATCC 33591) S. aureus obtained from American Type Culture Collection (ATCC; Rockville, MD, USA). These bacteria were individually inoculated in 5 mL of tryptic soy broth and grown aerobically overnight at 37°C. Each culture was harvested after centrifugation at 2,000 rpm for 10 min, washed twice with sterile distilled water and resuspended in sterile saline to a turbidity of 106 cells mL−1 (McFarland standard).
Cell culture
Immortalized L929 fibroblasts purchased from the Adolfo Lutz Institute (São Paulo, SP, Brazil) were cultured in Dulbecco's Modified Eagle Medium (DMEM; Sigma Chemical Co.) supplemented with 10% bovine fetal serum (Gibco, Grand Island, NY, USA) with 100 IU/mL penicillin, 100 μg/mL streptomycin and 2 mmol/L glutamine (Gibco) in an humidified incubator with 5% CO2 and 95% air at 37°C (Isotemp Fisher Scientific, Pittsburgh, PA, USA). The cells were sub-cultured every 3 days until an adequate number of cells were obtained for the study. After reaching approximately 80% density, the cells were trypsinized, seeded in sterile 24-well plates (30,000 cells/cm2) and incubated for 72 h.
Photosensitizer and light source
A stock solution of curcumin (200 μM) was prepared in DMSO. On the day of the experiment, this solution was diluted in sterile saline to final concentrations of 0.1, 0.5, 1, 5, 10, and 20 μM (keeping the final concentration of DMSO at 10%). A LED-based device with a predominant wavelength of 455 nm and composed of eight royal blue LEDs (LXHL-PR09, Luxeon® III Emitter, Lumileds Lighting, San Jose, CA, USA) uniformly distributed into the device was used to excite the PS. The intensity of light delivered was 22 mW/cm2.
Phototoxicity assay against MSSA and MRSA
Aliquots of 100 μL of MSSA suspension were individually transferred to separate wells of 96-well microtitre plates. An equal volume of each PS solution was added to each well to give final concentrations of 0.1, 0.5, 1, 5, 10, and 20 μM. After dark incubation for 20 min (pre-irradiation time), each plate was placed on the LED device. The MSSA suspensions were subjected to three light fluences, 18.0, 25.5, and 37.5 J/cm2. In order to determine whether curcumin alone had any effect on cell viability, additional wells containing one of the bacterial suspensions were exposed to curcumin identically to those described above, but not to LED light (C+L−). The effect of LED light alone was also determined by exposing cells to light without being previously exposed to curcumin (C−L+). Suspensions exposed to neither curcumin nor LED light were considered as the negative control group (C−L−).
Based on the results of the experiments reported above, the three concentrations of curcumin that achieved the most promising results for MSSA inactivation (5, 10, 20 μM) and the light fluence of 37.5 J/cm2 were selected to be used against MRSA. The experimental protocol was carried out as described above and the experimental groups C+L+, C+L−, C−L+ and C−L− were evaluated. To determine MSSA and MRSA survival, aliquots of the contents of each well were serially diluted tenfold in sterile saline to give dilutions of 10−1 to 10−3 times the original concentration. Triplicate 25-μL aliquots were plated onto mannitol salt agar plates. All plates were aerobically incubated at 37°C for 24 h and thereafter colony counts of each plate were quantified using a digital colony counter (CP 600 Plus, Phoenix Ind Com Equipamentos Científicos Ltda, Araraquara, SP, Brazil). The number of colony-forming units per milliliter (CFU/mL) was determined.
Phototoxicity assay of L929 fibroblasts
For the L929 fibroblast cell line, after 48 h of incubation, the culture medium was removed and cells were washed with phosphate buffered saline (PBS). Aliquots of 350 μL of curcumin at final concentrations of 5, 10, and 20 μM were transferred individually to wells of 24-well plates and were incubated in contact with the cells for 20 min protected from light. After incubation, cells were irradiated with a light fluence of 37.5 J/cm2. Additional wells containing cells exposed only to curcumin or only to LED light were also evaluated. Negative control group was composed of cells exposed to neither curcumin nor LED light.
For fibroblast culture, cell viability was evaluated by succinic dehydrogenase (SDH) production, which is a measure of the mitochondrial respiration of the cell. For such purpose, the methyltetrazolium (MTT) assay was used. In ten wells, 900 μL of DMEM plus 100 μL of MTT solution (5 mg/mL sterile PBS; Sigma Chemical Co.) were applied to the cells cultured in each well and incubated at 37°C for 4 h. Thereafter, the culture medium (DMEM with the MTT solution) was aspirated and replaced by 600 μL of acidified isopropanol solution (0.04 N HCl) to dissolve the blue crystals of formazan present in the cells. Cell metabolism was determined as being proportional to the absorbance measured at 570 nm wavelength with an ELISA plate reader (BIO-RAD, model 3550-UV, microplate reader, Hercules, CA, USA).
For analysis of the L929 cell line morphology by SEM, sterile 12-mm-diameter cover glasses (Fisher Scientific) were placed on the bottom of the wells of all experimental and control groups immediately before seeding the cells. After the experimental conditions, the culture medium was removed and the viable cells that remained adhered to the glass substrate were fixed in 1 mL of buffered 2.5% glutaraldehyde for 24 h and post-fixed with 1% osmium tetroxide for 1 h. The cells adhered to the glass substrate were then dehydrated in a series of increasing ethanol concentrations (30%, 50%, 70%, 95%, and 100%) and immersed in 1,1,1,3,3,3-hexamethyldisilazane (Acros Organics, Springfield, NJ, USA) for 90 min and stored in a desiccator for 24 h. The cover glasses were then mounted on metallic stubs, sputter-coated with gold and the morphology of the surface-adhered L929 cells was examined with a scanning electron microscope (JEOL-JMS-T33A Scanning Microscope, Tokyo, Japan).
Data analysis and statistics
Bacterial cell counts were carried out in duplicate and repeated five times for each experimental condition. For the purpose of analysis, colony-forming units per milliliter values were transformed into logarithm (log10). Data from microbiological evaluation (S. aureus) and cytotoxicity test (L929 fibroblasts) presented a normal distribution and were analyzed statistically by ANOVA and Tukey post hoc tests. P values of <0.05 were considered significant.
Results
Phototoxicity against MSSA and MRSA
The three highest concentrations of curcumin (5, 10, and 20 μM) in combination with any of the light fluences (18.0, 25.5 and 37.5 J/cm2) resulted in complete elimination of MSSA. In these cases, the log reduction achieved was over six logs. The association of lower curcumin concentrations (0.1, 0.5, and 1 μM) with light decreased the MSSA viability (CFU/mL counts) in a dose-dependent manner (Fig. 1). In these experimental conditions, the highest log reduction observed was approximately of 5 logs corresponding to MSSA exposed to 1 μM of curcumin at 25.5 J/cm2. Colony counts of MSSA exposed only to LED light or curcumin was not different from the negative control group (Table 1), indicating that only the combination of curcumin with light was able to cause a significant reduction on colony-forming units per milliliter counts.
Effect of curcumin concentrations on MSSA cell survival (in colony-forming units per milliliter) at different light fluences. MSSA suspensions were incubated for 20 min with curcumin concentrations ranging from 0.1 to 20 μM and then irradiated with blue LED at three different light fluences (18, 25.5, and 37.5 J/cm2). Data are expressed as mean values of three independent experiments (n = 3)
For MRSA, the concentration of 20 μM combined with illumination (37.5 J/cm2) caused the total inactivation of bacterial suspensions. The other two concentrations (5 and 10 μM) significantly reduced the CFU/mL counts (Fig. 2). The log reduction achieved was of 6.7, 8.3, and 9.8 logs for the curcumin concentrations of 5, 10 and, 20 μM, respectively. The C+L−, C−L+, and C−L− showed no significant changes in cell numbers throughout the course of the experiment.
Graphic representation of mean values and standard deviation of survival counts (in colony-forming units per milliliter) observed after experiments with MRSA. The light fluence used was 37.5 J/cm2 (groups C−L + and C+L+). Different uppercase letters denote significant differences among columns (groups) according to Tukey's test (p < 0.05)
Phototoxicity against L292 cell line
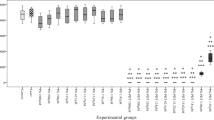
Figure 3 presents the effect of PDT (C+L+), different curcumin concentrations (C+L), and LED light (C−L+) on cell viability. Considering the negative control group (C−L−) as having 100% of cell viability, the metabolic activity of the L929 cells decreased by 68.1%, 75.1%, and 80% when exposed to 5, 10, and 20 μM curcumin concentrations in combination with blue LED light, respectively. In those groups, there was no statistically significant difference (p > 0.05) among the curcumin concentrations (5, 10, and 20 μM). The toxicity of curcumin without exposure to light was also evaluated and no significant difference (p > 0.05) was observed compared with the negative control group.
Graphic representation of mean values and standard deviation of absorbance values (MTT assay) observed after experiments with L929 fibroblast. The light fluence used was 37.5 J/cm2 (groups C−L+ and C+L+). Different uppercase letters denote significant differences among columns (groups) according to Tukey's test (p < 0.05)
Figure 4 (a–d) is a composite figure of SEM micrographs of the L929 fibroblasts representative of the experimental and control groups. For the negative control group (no treatment) and the group treated only with curcumin (20 μM), numerous L929 fibroblasts that remained adhered to the glass substrate exhibited a spindle-shaped appearance with few cytoplasmic processes originating from the membrane (Fig. 4a,b). Arrows indicate mitoses occurring in both groups. In the groups subjected to PDT, a smaller number of L929 fibroblasts remained adhered to the cover glass. In some areas of the glass substrate, rests of cytoplasmic membrane of dead cells were observed (Fig. 4c,d).
Discussion
The present in vitro study showed the efficacy of PDT using curcumin at a final concentration of 20 μM and blue LED light in promoting photokilling of MSSA and MRSA strains. Curcumin has been extensively investigated for therapeutic applications due to its anti-inflammatory, antitumor, and antimicrobial effects [18]. The antimicrobial action of this substance is directly related to its combination or not with excitation by a visible light source [17]. Wang et al. [19] found that the minimum inhibitory concentration (MIC) of curcumin against S. aureus without illumination was 62.5 mg/L. Another study confirmed the antifungal action of curcumin and found that its MIC against different Candida spp. species without light activation ranged from 32 to 256 mg/L [16].
On the other hand, when used in combination with visible light, the concentration of curcumin required to promote photoinactivation of bacteria is reduced to the micromolar level, as demonstrated in the present study. On irradiation with blue LED light, curcumin caused cytotoxic effects to both MSSA and MRSA and its phototoxicity was expressed in a PS concentration-, light fluence-, and bacterial strain-dependent manner. A 5-μM concentration of curcumin used in combination with the lowest energy density (18 J/cm2) was sufficient to promote photokilling of MSSA. The capacity of curcumin exerting potent phototoxic effects in micromolar amounts when illuminated by a visible light source has been described [17, 20]. Haukvik et al. [20] evaluated photokilling of gram-positive Enterococcus faecalis, Streptococcus intermedius, and gram-negative Escherichia coli after treatment with curcumin and blue light illumination and found that a 2.5 μM concentration was sufficient to kill the gram-positive bacteria, while a 25 μM concentration was necessary for E. coli. Only one study has so far evaluated the photokilling of S. aureus by curcumin [17] and the authors observed that washout of curcumin before illumination resulted in minimal reduction of bacterial counts (in colony-forming units per milliliter), even after a 90-min pre-incubation period with the PS. This result suggests that the photodynamic effect is greatly increased when curcumin is present during light application. Curcumin phototoxicity to bacterial strains seems to be mediated by the excited states of curcumin and/or products derived from the subsequent reactions with oxygen during irradiation [18]. This way, light is responsible for the triplet excited state of curcumin, resulting in energy or electron transfer to molecular oxygen with consequent formation of ROS, which ultimately cause destruction of microbial cells [21].
In the present study, a higher curcumin concentration (20 μM) combined with illumination at 37.5 J/cm2 was necessary for photodynamic inactivation of MRSA, which means that the methicillin-resistant strain was more resistant to PDT than the MSSA, requiring a fourfold higher concentration of the PS to be inactivated. Recent studies have reported that higher concentrations of PS were necessary for killing of MRSA compared with MSSA strains [14, 22]. Grinholc et al. [14] reported that the response of different MSSA and MRSA strains to PDT was not homogenous, and 0 to 3 log10-unit reduction in viable counts was observed when a porphyrin was used as a PS for photodynamic inactivation of the bacteria. Those authors observed more PDT-resistant MRSA strains compared with the MSSA strains, as observed in the present study. Tsai et al. [22] also found that the PDT susceptibility of MRSA strains was lower than the other antibiotic-susceptible strains. This greater resistance of MRSA strains to PDT has been related to the capsular polysaccharide structure on the bacterial cell surface, which would limit the penetration of the PS into the MRSA cells, reducing the toxic effects of the ROS generated during photodynamic inactivation [23]. The need for higher light fluences and drug concentration for resistant strains have been also observed for yeasts, showing that fluconazole-resistant C. albicans and C. glabrata strains had reduced sensitivity to PDT [12]. It is accepted that PDT is a non-specific and effective treatment against both susceptible and resistant pathogen [22]. Until now, the studies reported that PDT effect is strain- and isolate-dependent. In our study, the ATTC evaluated strains presented the behavior of susceptible bacteria being more sensitive to PDT treatment than the resistant bacteria. However, Grinholc et al. [14] reported on MRSA isolates highly sensitive to PDT, whereas there are some other MRSA isolates resistant to its effects [14, 22]. Therefore, it is relevant to evaluate the susceptibility of resistant microorganisms to PDT in order to determine whether it can be used in the treatment of infections in which the prevalence of these microorganisms has increased at alarming rates.
In the same way, it is important to investigate the potential toxic effects of PDT to the host’s cells, which are also susceptible to the action of ROS. In the present study, the metabolism of cultured fibroblast cells decreased by 68.1, 75.1, and 80% in response to exposure to curcumin at 5, 10, and 20 μM concentrations, respectively, in combination with blue LED light illumination. Similarly, in a previous study, porphyrin-mediated photodynamic therapy reduced the viability of human dermal fibroblasts by 66.5% and caused photodynamic inactivation of 99.9% of MRSA [14]. Even considering that the reduction of cell metabolism was accentuated in our study, it was not sufficient to cause complete inhibition of the SDH enzyme, suggesting that both MSSA and MRSA strains were more susceptible to PDT than the L929 fibroblasts. Dovigo et al. [24] obtained similar results when the same parameters used for fungal cells were applied for macrophage cell culture. While a complete photokilling was achieved for C. albicans planktonic cells, the macrophages metabolism was not completely reduced. Despite the significant reduction of cell metabolism, the in vitro experiments cannot reproduce all in vivo conditions. In a living organism, in response to the oxidative stress generated by the presence of ROS, the defense the system releases several endogenous antioxidant agents, such as peroxidases and catalases, which promotes an enzymatic degradation of those highly reactive and unstable molecules to avoid excessive tissue damage [25].
The interaction of curcumin with biomolecules and cells has been investigated. Results of recent studies have indicated that curcumin binds preferentially to lipid membrane and some cell proteins [18]. Bruzell et al. [26] observed that PDT using curcumin at 13.5 μM in combination with halogen light illumination (6 J/cm2) resulted in around 80% of necrotic cell death and less the 20% of apoptotic cell death. In the present study, the SEM analysis revealed that the fibroblast cell cultures subjected to PDT exhibited a significant decrease in the number of cells adhered to the glass substrate. In addition, several cytoplasmic rests remained adhered to the glass coverslip, indicating rupture of the cytoplasmic membrane and suggesting necrotic cell death.
Another factor to be considered for the use of curcumin as a PS is the vehicle used to deliver this compound. As curcumin is relatively insoluble in water, various diluents like acetone, DMSO, and ethanol as well as other preparations such as micelles, cyclodextrine, liposomes, and hydrophilic polymers have been proposed as vehicles for curcumin [26]. DMSO is the most commonly used vehicle to evaluate the phototoxic effects of PDT in in vitro studies and it has become a control to evaluate several types of drug vehicles because of its excellent solvent propriety [15, 20]. In the present study, dilution of curcumin in DMSO increased its solubility in aqueous solutions, improving its bioavailability and promoting bacterial photokilling [27]. Bruzell et al. [26] reported that the use of curcumin at 13.5 μM diluted in DMSO was sufficient to reduce by 80% the viability of rat submandibular salivary gland acinar cells. However, preparation of the same curcumin concentration in cyclodextrine or liposome did not cause reduction of enzymatic activity. It is known that DMSO is not an optimal vehicle for in vivo applications because it increases membrane permeability to the drugs and may cause tissue damage and systemic effects [20]. Therefore, further studies should evaluate different vehicles as efficient as DMSO for curcumin to exert photokilling against bacterial strains.
Both essential components of PDT—the PS and the visible light—can alter cell functions. However, in the present study, no significant differences were observed between the groups exposed only to curcumin (C+L−) or blue LED light (C−L+) when compared with the negative control (C−L−). Without illumination, the curcumin concentrations were insufficient to cause toxic effects against the bacteria and the fibroblast cultures. As mentioned before, micromolar concentrations caused cell damage only when used in combination with visible light because of ROS formation. In a similar way, no significant alteration in colony numbers of MSSA and MRSA or in the metabolism of fibroblast cells was detected after the use of LED light without previous photosentization with curcumin. The results of the present investigations are in agreement with those of Ribeiro et al. [13] who did not find significant reduction on the metabolism of L929 fibroblasts and MDPC-23 cells using the same light source (blue LED) at similar light fluence (37.5 J/cm2).
The results of the present study showed the efficiency of curcumin combined with blue LED light in causing photoinactivation of MSSA and MRSA. This therapy also caused a significant reduction of L929 cell metabolism, but was more effective in inactivating the bacterial samples than the fibroblast cell. The planktonic cultures used in this study represent the first step for evaluation of a light-sensitive compound in PDT. In the same way, cell cultures are more susceptible to the photocytotoxic effects of this therapy because they do not present the defense systems existing in a living organism. Therefore, further in vitro studies using biofilms and three-dimensional cultures as well as in vivo investigations are necessary to confirm the potential of curcumin as a PS as well as its clinical application on PDT.
Conclusion
This article demonstrated the efficiency of curcumin in combination with LED in promote photodynamic inactivation of MRSA. Although a significant reduction around 80% on fibroblast metabolism were also observed, this therapy caused photodynamic inactivation of 100% of MRSA showing that PDT was more efficient against bacteria. Therefore, the results obtained encourage the continued evaluation of PDT protocols using natural compounds to eradicate pathogenic bacteria such as MRSA in institutions and hospitals in which these bacteria are responsible for significantly higher morbidity and mortality and increased healthcare costs.
References
Sumi Y, Miura H, Michiwaki Y, Nagaosa S, Nagaya M (2007) Colonization of dental plaque by respiratory pathogens in dependent elderly. Arch Gerontol Geriatr 44:119–124
Smith AJ, Jackson MS, Bagg J (2001) The ecology of Staphylococcus species in the oral cavity. J Med Microbiol 50:940–946
Terpenning M (2005) Geriatric oral health and pneumonia risk. Clin Infect Dis 40:1807–1810
Rossi T, Peltonen R, Laine J, Eerola E, Vuopio-Varkila J, Kotilainen P (1996) Eradication of the long-term carriage of methicillin-resistant Staphylococcus aureus in patients wearing dentures: a follow-up of 10 patients. J Hosp Infect 34:311–320
Buehlmann M, Frei R, Fenner L, Dangel M, Fluckiger U, Widmer AF (2008) Highly effective regimen for decolonization of methicillin-resistant Staphylococcus aureus carriers. Infect Control Hosp Epidemiol 29:510–516
Maeda Y, Kenny F, Coulter WA, Loughrey A, Nagano Y, Goldsmith CE et al (2007) Bactericidal activity of denture-cleaning formulations against planktonic health care-associated and community-associated methicillin-resistant Staphylococcus aureus. Am J Infect Control 35:619–622
Simor AE, Phillips E, McGeer A, Konvalinka A, Loeb M, Devlin HR et al (2007) Randomized controlled trial of chlorhexidine gluconate for washing, intranasal mupirocin, and rifampin and doxycycline versus no treatment for the eradication of methicillin-resistant Staphylococcus aureus colonization. Clin Infect Dis 44:178–185
Loveday HP, Pellowe CM, Jones SR, Pratt RJ (2006) A systematic review of the evidence for interventions for the prevention and control of meticillin-resistant Staphylococcus aureus (1996–2004): report to the Joint MRSA Working Party (Subgroup A). J Hosp Infect 63(Suppl 1):S45–S70
Donnelly RF, McCarron PA, Tunney MM (2008) Antifungal photodynamic therapy. Microbiol Res 163:1–12
Engelhardt V, Krammer B, Plaetzer K (2010) Antibacterial photodynamic therapy using water-soluble formulations of hypericin or mTHPC is effective in inactivation of Staphylococcus aureus. Photochem Photobiol Sci 9:365–369
Konopka K, Goslinski T (2007) Photodynamic therapy in dentistry. J Dent Res 86:694–707
Dovigo LN, Pavarina AC, Mima EG, Giampaolo ET, Vergani CE, Bagnato VS (2011) Fungicidal effect of photodynamic therapy against fluconazole-resistant Candida albicans and Candida glabrata. Mycoses 54:123–130
Ribeiro AP, Pavarina AC, Trindade FZ, Inada NM, Bagnato VS, de Souza Costa CA (2010) Photodynamic therapy associating Photogem and blue LED on L929 and MDPC-23 cell culture. Cell Biol Int 34:343–351
Grinholc M, Szramka B, Kurlenda J, Graczyk A, Bielawski KP (2008) Bactericidal effect of photodynamic inactivation against methicillin-resistant and methicillin-susceptible Staphylococcus aureus is strain-dependent. J Photochem Photobiol B 90:57–63
Epstein J, Sanderson IR, Macdonald TT (2010) Curcumin as a therapeutic agent: the evidence from in vitro, animal and human studies. Br J Nutr 103:1545–1557
Martins CV, da Silva DL, Neres AT, Magalhães TF, Watanabe GA, Modolo LV et al (2009) Curcumin as a promising antifungal of clinical interest. J Antimicrob Chemother 63:337–339
Dahl TA, McGowan WM, Shand MA, Srinivasan VS (1989) Photokilling of bacteria by the natural dye curcumin. Arch Microbiol 151:183–185
Priyadarsini KI (2009) Photophysics, photochemistry and photobiology of curcumin: studies from organic solutions, bio-mimetics and living cells. J Photoch Photobio C 10:81–95
Wang Y, Lu Z, Wu H, Lv F (2009) Study on the antibiotic activity of microcapsule curcumin against foodborne pathogens. Int J Food Microbiol 136:71–74
Haukvik T, Bruzell E, Kristensen S, Tønnesen HH (2009) Photokilling of bacteria by curcumin in different aqueous preparations. Studies on curcumin and curcuminoids XXXVII. Pharmazie 64:666–673
Shen L, Jia HF, Zhang HY (2005) A TD-DFT study on triplet excited-state properties of curcumin and its implications in elucidating the photosensitizing mechanisms of the pigment. Chem Phys Lett 409:300–303
Tsai T, Yang YT, Wang TH, Chien HF, Chen CT (2009) Improved photodynamic inactivation of gram-positive bacteria using hematoporphyrin encapsulated in liposomes and micelles. Lasers Surg Med 41:316–322
Szpakowska M, Lasocki K, Grzybowski J, Graczyk A (2001) Photodynamic activity of the haematoporphyrin derivative with rutin and arginine substituents (HpD-Rut(2)-Arg(2)) against Staphylococcus aureus and Pseudomonas aeruginosa. Pharmacol Res 44:243–246
Dovigo LN, Pavarina AC, Ribeiro AP, Brunetti IL, Costa CA, Jacomassi DP, Bagnato VS, Kurachi C (2011) Investigation of the photodynamic effects of curcumin against Candida albicans. Photochem Photobiol 87:895–903
Esposito P, Varvara G, Caputi S, Perinetti G (2003) Catalase activity in human healthy and inflamed dental pulps. Int Endod J 36:599–603
Bruzell EM, Morisbak E, Tønnesen HH (2005) Studies on curcumin and curcuminoids. XXIX. Photoinduced cytotoxicity of curcumin in selected aqueous preparations. Photochem Photobiol Sci 4:523–530
Kurien BT, Scofield RH (2009) Heat-solubilized curcumin should be considered in clinical trials for increasing bioavailability. Clin Cancer Res 15:747
Acknowledgments
The authors would like to acknowledge the Center of Study in Optics and Photonics (CEPOF) ant the Physics Institute of São Carlos (IFSC) of the University of São Paulo (USP) for developing the LED prototype used in this study. This work was supported by FAPESP—São Paulo Research Foundation (Grants 2008/03994-9 and 2010/05425-1).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ribeiro, A.P.D., Pavarina, A.C., Dovigo, L.N. et al. Phototoxic effect of curcumin on methicillin-resistant Staphylococcus aureus and L929 fibroblasts. Lasers Med Sci 28, 391–398 (2013). https://doi.org/10.1007/s10103-012-1064-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-012-1064-9