Abstract
Methicillin-resistant Staphylococcus aureus (MRSA) is a major cause of hospital acquired infection throughout the world especially in wound and burn infections, pneumonia, septicaemia and endocarditis. We describe the effect of a HeNe laser in combination with a TBO dye on the viability of MRSA. A total of 34 isolates of S. aureus were obtained from 100 patients suffering from burns or wounds and from the nasal vestibulum of medical and nonmedical staff as carriers; eight isolates were methicillin-resistant. The isolates were exposed for 5, 10 and 15 min to a HeNe laser at a wavelength of 632.8 nm and 7.5 mW output power in the presence of 50 μg/ml toluidune blue O photosensitizer. The viable count was substantially decreased as determined by the plate count method for the three exposure times, with 100% killing with the 15-min exposure time. No significant effect was observed on MRSA isolates exposed to the laser alone. So MRSA was completely eradicated following 15 min exposure to a 632.8-nm HeNe laser in the presence of 50 μg/ml toluidune blue O photosensitizer under in vitro conditions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The introduction of lasers has led to extensive benefits in many fields of biology and medicine. Photodynamic antimicrobial chemotherapy has been under investigation since the invention of the laser and the development of drug-resistant strains of bacteria. The gram-positive bacterium Staphylococcus aureus is one of the main agents in nosocomial infections, and is the principle surgical killer throughout the world [1]. Staphylococcus aureus lives commensally on human skin, nares and mucosal surfaces, as an opportunistic pathogen able to infect, invade, and persist and replicate in many human tissues [2]. Staphylococcus aureus was sensitive to penicillin when it was introduced in the late 1940s, but resistance developed almost immediately [3] as a result of S. aureus acquiring a β-lactamase capable of inactivating the β-lactam ring. Lactamase-resistant antibiotics (methicillin, oxacillin) remained effective until the early 1960s [4, 5], when S. aureus acquired a new gene that modified its penicillin binding protein [6–10] and therefore became resistant to penicillin, semisynthetic penicillin derivatives and a wide variety of antimicrobials [8, 11–14]. Major outbreaks of methicillin-resistant S. aureus (MRSA) infection quickly occurred in hospitals [15–19] followed by the development of community-acquired strains of MRSA [20, 21].
The multidrug resistance of S. aureus makes it the most notorious of all bacterial pathogens associated with human infections [2]. Accordingly many in vitro studies have focused on the use of photodynamic antimicrobial therapy to eliminate extracellular pathogenic gram-positive bacteria, especially S. aureus. Photodynamic inactivation of microorganisms is based on the localization of a dye, known as a photosensitizer, preferentially in bacteria and not in the surrounding tissues or cells. and subsequent activation of the photosensitizer by low doses of visible light of an appropriate wavelength to generate free radicals or singlet oxygen that are toxic to the target microorganisms [22]. The combined use of a 664-nm diode laser and toluidine blue O (TBO) or methylene blue has been shown to eradicate various bacterial species including S. aureus [23]. In a study by Griffiths et al.,16 epidemic MRSA strains were treated with a combination of aluminium disulphonated phthalocyanine and diode laser light. An 8.5-log10 reduction in MRSA was observed with a light dose of 3.89 J and 6.25 mg/l of the phthalocyanine [24]. Irradiation with 675-nm light in combination with Zn(II)-phthalocyanine peripherally substituted with four bis(N,N,N-trimethyl)amino-2-propyloxy groups has been shown to result in a 5-log or greater decrease in survival of S. aureus and Escherichia coli [25]. The aim of the present study was to determine the bactericidal activity of 632.8-nm HeNe laser light in the presence of 50 μg/ml TBO as photosensitizer against MRSA.
Materials and methods
Isolation and identification of bacteria
A total of 100 swab samples were taken from the surface of burns and wounds, and from the nasal vestibulum of medical and nonmedical staff as carriers. The samples were inoculated directly onto sheep blood agar and mannitol/salt agar and incubated at 37°С for 24 h. Staphylococcus aureus isolates were identified by routine methods [26]. For stock preparations, S. aureus isolates were plated on trypticase soy agar. One isolated colony from each culture was grown to stationary phase in trypticase soy broth and stored at −70°C in sterile glycerol (final concentration 12% v/v). These stocks were called the original stocks and cultures obtained directly from them were designated original cultures [9]
Cefoxitin disk diffusion test
The test was done as recommended by the US National Committee for Clinical Laboratory Standards (NCCLS) [27]. Briefly, a sterile cotton swab dipped into an overnight culture was diluted to 107–108, pressed against the side of a tube to remove any excess fluid, and streaked onto a Muller-Hinton agar plate. The disk was applied and the plate was incubated at 35°C for 16–18 h.
Combined oxacillin and methicillin agar screen
Muller-Hinton agar was supplemented with oxacillin 6 mg/l or methicillin 10 mg/l and NaCl 4% w/v (final concentration).The inoculum was prepared as recommended by the NCCLS guidelines [28]. After incubation at 35°C for 24 h, MRSA should grow on these plates, whereas borderline-resistant and susceptible strains should fail to grow under these conditions.
Susceptibility testing
Susceptibility to antimicrobial agents (vancomycin, rifampicin and gentamicin) was determined by the agar disk diffusion method, following procedures outlined in the guidelines of the NCCLS [27].
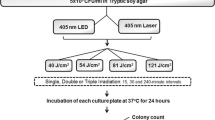
Irradiation procedure
Preparation of bacterial suspensions
Bacterial suspensions were prepared by inoculating one isolated colony in a tube containing 4–5 ml of tryptic soya broth, incubating at 35°C for 16 h. centrifuging, and then resuspending in 0.85% NaCl.
Laser system
The laser used in this study was a HeNe gas laser with a measured output of 7.5 mW. It emitted light in a collimated beam with a diameter of 4 mm and a wavelength of 632.8 nm. The exposure times were 5, 10, 15 and 20 min, and the power density was 59.7 mW/cm2.
Preparation of TBO
The stock of TBO (Sigma, Poole, UK) was prepared by dissolving 5 mg TBO powder in 100 ml distilled water to a concentration of 50 µg/ml. The solution was sterilized through a 0.22-µm Millipore filter, and stored in the dark until use.
Irradiation of bacteria for susceptibility testing
Aliquots (15 µl) of MRSA suspension (1×109 cfu/ml) were transferred to sterile Ependorff tubes and exposed to measured amounts of laser light for 5, 10, 15 and 20 minutes. Control Ependorff tubes were not exposed to the laser light. Following exposure to the light, the suspension from each Ependorff tube was plated onto Muller-Hinton agar using a sterile cotton swab, and after applying the drug disk the plate was placed upside down in an incubator at 35–37°C for 18 h.
Irradiation of bacteria
Aliquots (15 µl) of MRSA suspension (1×109 cfu/ml) were transferred to sterile Ependorff tubes containing an equal volume of filtered sterilized TBO solution with a final concentration of 50 µg/ml. The samples were exposed to measured amounts of laser light for 5, 10, 15 and 20 min (this group of samples is referred to as L+S+). A control group of samples were exposed to laser light without photosensitizer (L+S−). Another group of samples were placed in the dark and 50 µg/ml TBO was added to them (L−S+). A further group of samples acted as a blank, neither sensitized nor exposed to the laser light (L−S−). Following exposure to the laser light, the irradiated samples and the control groups were spread using a cotton swab over the surface of nutrient agar plates, grown overnight at 37°C, and examined carefully under transmitted light for evidence of small colonies.
Statistics
The results were analysed using the Statistical Analysis System (SAS) [29]., Mean least significant differences (LSD) were compared using known conventions.
Results and discussion
A total of 34 isolates (11 from burns, 12 from wounds, and 11 from carriers) of S. aureus species were identified according to their culture characteristics, and by microscopic and biochemical tests. They were categorized as gram-positive, spherical cells, nonmotile cells of about 1 µm in diameter, nonspore-forming cells, and facultative anaerobes. They formed golden yellow colonies on agar, and were haemolytic on blood agar. They were catalase-positive and oxidase-negative, and they fermented mannitol. Staphylococcus aureus grows at temperatures in the range 15–45°C in the presence of NaCl at concentrations as high as 15%. MRSA was detected in 8 (23%) of 34 examined isolates. The inhibition zone diameters for both MRSA and methicillin-susceptible S. aureus isolates were distinct when using 30 µg cefoxitin disks. All MRSA isolates showed cefoxitin inhibition zone diameters of <27 mm, and all methicillin-susceptible S. aureus isolates showed larger diameters. The agar screen (oxacillin 6 mg/l or methicillin 10 mg/l), as recommended by the NCCLS, detected MRSA in all isolates from the carriers.
In view of the results presented here, the use of the 30 µg cefoxitin disk diffusion test and agar screen using oxacillin 6 mg/l or methicillin 10 mg/l are strongly recommended for screening MRSA carriers. The eight MRSA isolates were tested for their sensitivity to antimicrobial agents by the disk diffusion method, and 70% of the isolates were resistant to rifampicin and 80% to gentamicin. The isolates were also resistant to cefoxitin and oxacillin, so these antibiotics would be ineffective as therapeutic agents against MRSA. Resistance to vancomycin was not observed, but 50% of the isolates showed intermediate resistance to vancomycin, and thus this bacterium is a great threat to public health and the hospital environment
After irradiation with the HeNe laser for different times (5, 10, 15 or 20 min), the isolates with intermediate resistance to vancomycin before laser irradiation become sensitive to it, while remaining resistant to other antibiotics (Fig. 1).
Exposure of bacterial suspensions to TBO/HeNe laser light for 5, 10 and15 min resulted in significant reductions in viable counts compared with the control group in which the total bacterial count remained unchanged (Fig. 2). All MRSA isolates were killed when exposed to TBO/HeNe laser light for 15 min. Laser irradiation in the presence of TBO killed 99.1% of wound isolate cells, 97.3% of cells from carriers and 95.4% of burn isolate cells (Fig. 3).
Some pathogens accumulate a wide range of photosensitive agents [30] and multidrug-resistant strains are known to be susceptible to host destruction [31]. Recently, the use of light in conjunction with chemical photosensitizers to treat antimicrobial infections has been the subject of several studies [32].
Wilson and Yianni reported a 4.47-log reduction in the viable count of MRSA following irradiation with a low-power HeNe laser in the presence of 12 μg/ml TBO [23]. The ability of TBO to act as a photosensitizer after irradiation with visible light has been demonstrated in several studies. Tang et al. reported that irradiation at 30 J/cm2 in the presence of TBO at 80 µM resulted in 3-log killing of MRSA and 2-log killing of the corresponding ATCC S. aureus strain [33]. Packer et al. reported inactivation of the proteolytic enzymes of the oral microorganism Porphyromonas gingivalis by irradiation with 126 J of red laser light in the presence of 12.5 μg/ml of TBO [34]. Significant inactivation of cells was observed when staphylococcal biofilms were exposed to TBO and laser light simultaneously. The efficacy of photodynamic therapy for biofilm treatment depends mainly on the penetration of the photosensitizer and light to the deeper layers [35]. Photoeradication of organisms implicated in dental carries, such as Streptococcus spp. using TBO or methylene blue as photosensitizers has been reported, but unfortunately the killing percentage achieved and the dose parameters used were not mentioned [30]. In a recent study investigating the effect of toluidine blue-mediated photodynamic therapy on oral wound infections in rats, treatment with toluidine blue at 1 mg/ml in combination with exposure to red light resulted in a kill rate of approximately 97% with a light dose of 48 J/cm2 while bacterial survival was 25% at a light dose of 12 J/cm2 [36]. MRSA may also be killed by exposure to red laser light in the presence of a tin(IV) chlorin e6/IgG conjugate [37], but the lethal effect depended on the strain and the phase of growth.
As do other cationic azine photosensitizers, cationic TBO also remains outside the cell. Thus singlet oxygen contributes to the overall photodynamic process and the damage occurs at the membrane level [38]. After appropriate illumination, the photosensitizer undergoes a transition from a low-energy ground state to a higher energy triplet state, and then falls back to the lower energy state. The emitted energy reacts with cellular oxygen and/or other cellular components to produce reactive species such as singlet oxygen and free radicals. The three main sites of action of the cytotoxic species are the cell membrane, the nucleus, and organelles [34]. TBO is known to be membrane-active, since it causes an increase in permeability [30]. Increasing ion permeability and loss of fluidity results from the transfer of the triplet state photosensitizer energy to molecular oxygen forming singlet oxygen which is the main bactericidal species and is involved in lipid peroxidation, which is highly detrimental to cell membrane structure and function and leads to cell death [39, 40]. Singlet oxygen generated in the photosensitization process has a very short life and limited diffusion distance [37], ensuring localization of the toxic effects to the microbes in the treated region only. In contrast to the effects of systemic treatments, the normal microflora at other body sites are unaffected [41].
Conclusion
Antibiotic resistance among bacteria in general and MRSA in particular is a cause of acute concern. Development of alternative therapeutic approaches is necessary to curtail the inappropriate and wasteful use of antibiotics which encourages drug resistance. This in vitro study demonstrated that exposure to HeNe laser light in the presence of TBO at 50 µg/ml was able to eradicate MRSA in vitro, and may be a good candidate for a novel treatment of MRSA infections. One of the objectives in photodynamic therapy is to direct the dye to the site of infection. For increased selectivity, further experiments are needed to target specific sites of infection in the body.
References
Takahashi S, Tanaka T, Ashiki A (1990) Clinical studies of methicillin resistant S. aureus (MRSA) infections during the recent 10 months in our department. Nippon Hinyokika Gakkai Zasshi 81(10):1480–1486
Bae T, Banger AK, Wallace A, Glass EM, Aslund F, Schneewind O, Missiakas DM (2004) Staphylococcus aureus virulence genes identified by bursa aurealis mutagenesis and nematode killing. Proc Natl Acad Sci U S A 101(33):12312–12317
Bass SE, Joshi SS, Nuttall D, Sazinsky SL, Scharschmidt T, Spencer RB (2001) Staphylococcus. Course Biotechnology and Its Social Impact (MOL 427), Princeton University
Collignon PJ (2002) 11. Antibiotic resistance. Med J Aust 177:325–329
Diekema DJ, Pfaller MA, Schmitz FJ, Smayevsky J, Bell J, Jones RN, Beach M; SENTRY participants group (2001) Survey of infections due to Staphylococcus species: frequency of occurrence and antimicrobial susceptibility of isolates collected in the United States, Canada, Latin America, Europe, and the Western Pacific region for the SENTRY Antimicrobial Surveillance Program, 1997-1999. Clin Infect Dis 32:S114–S132
Thornsberry C (1988) The development of antimicrobial resistance in staphylococci. J Antimicrob Chemother 21(Suppl C):9–17
Wielders CL, Fluit AC, Brisse S, Verhoef J, Schmitz FJ (2002) mecA gene is widely disseminated in Staphylococcus aureus population. J Clin Microbiol 40(11):3970–3975
Grisold AJ, Leitner E, Muhlbauer G, Marth E, Kessler HH (2002) Detection of methicillin-resistant Staphylococcus aureus and simultaneous confirmation by automated nucleic acid extraction and real-time PCR. J Clin Microbiol 40:2392–2397
Falcao MH, Texeira LA, Ferreira-Carvalho BT, Borges-Neto AA, Figueiredo AM (1999) Occurrence of methicillin-resistant and -susceptible Staphylococcus aureus within a single colony contributing to MRSA mis-identification. J Med Microbiol 48:515–521
Rosato AE, Kreiswirth BN, Craig WA, Eisner W, Climo MW, Archer GL (2003) mecA-blaZ corepressors in clinical Staphylococcus aureus isolates. Antimicrob Agents Chemother 47:1460–1463
Bren L (2002) The battle of the bugs: fighting antibiotic resistance. FDA Consum 36(4):28–34
Musser JM, Kapur V (1992) Clonal analysis of methicillin-resistant Staphylococcus aureus strains from intercontinental sources: association of the mec gene with divergent phylogenetic lineages implies dissemination by horizontal transfer and recombination. J Clin Microbiol 30:2058–2063
Blumberg HM, Rimland D, Carroll DJ, Terry P, Wachsmuth IK (1991) Rapid development of ciprofloxacin resistance in methicillin-susceptible and -resistant Staphylococcus aureus. J Infect Dis 163:1279–1285
Hu ZQ, Zhao WH, Asano N, Yoda Y, Hara Y, Shimamura T (2002) Epigallocatechin gallate synergistically enhances the activity of carbapenems against methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother 46:558–560
Shanson DC, Kensit JC, Duke R (1976) Outbreak of hospital infection with a strain of Staphylococcus aureus resistant to gentamicin and methicillin. Lancet 2:1347–1348
Cookson BD, Phillips I (1988) Epidemic methicillin-resistant Staphylococcus aureus. J Antimicrob Chemother 21(Suppl C):57–65
Cafferkey MT, Hone R, Coleman D, Pomeroy H, McGrath B, Ruddy R, Keane CT (1985) Methicillin-resistant Staphylococcus aureus in Dublin 1971–84. Lancet 2:705–708
Schaefler S, Jones D, Perry W, Ruvinskaya L, Baradet T, Mayr E, Wilson ME (1981) Emergence of gentamicin- and methicillin-resistant Staphylococcus aureus strains in New York City hospitals. J Clin Microbiol 13:754–759
Pavillard R, Harvey K, Douglas D (1982) Epidemic of hospital-acquired infection due to methicillin-resistant Staphylococcus aureus in major Victorian hospitals. Med J Aust 1:451–454
Okuma K, Iwakawa K, Turnidge JD, Grubb WB, Bell JM, O'Brien FG, Coombs GW, Pearman JW, Tenover FC, Kapi M, Tiensasitorn C, Ito T, Hiramatsu K (2002) Dissemination of new methicillin-resistant Staphylococcus aureus clones in the community. J Clin Microbiol 40:4289–4294
Vandenesch F, Naimi T, Enright MC, Lina G, Nimmo G, Hefferman H, Liassine N, Bes B, Greenl T, Reverdy ME, Etienne J (2003) Community-acquired methicillin-resistant Staphylococcus aureus carrying Panton-Valentine leukocidin genes: worldwide emergence. Emerg Infect Dis 9(9):978–984
Maisch T (2007) Anti-microbial photodynamic therapy: useful in future? Lasers Med Sci 22:83–91
Wilson M, Yianni C (1995) Killing of methicillin-resistant Staphylococcus aureus by low power laser light. J Med Microbiol 42:62–66
Griffiths MA, Wren BW, Wilson M (1997) Killing of methicillin-resistant Staphylococcus aureus in vitro using aluminium disulphonated phthalocyanine, a light-activated antimicrobial agent. J Antimicrob Chemother 40:873–876
Segalla A, Borsarelli CD, Braslavsky SE, Spikes JD, Roncucci G, Dei D, Chiti G, Jori G, Reddi E (2002) Photophysical, photochemical and antibacterial photosensitizing properties of a novel octacationic Zn(II)-phthalocyanine. Photochem Photobiol Sci 1:641–648
Kloos WE, Bannerman TL (1995) Staphylococcus and micrococcus. In: Murray PR, Baron JE, Pfaller AM, Tenover CF, Yolken RH (eds) Manual of clinical microbiology, 6th edn. American Society for Microbiology, Washington, DC, pp 282–259
National Committee for Clinical Laboratory Standards (2002) Performance standards for antimicrobial susceptibility testing. Approved standard M100-S12. Twelfth informational supplement. NCCLS, Wayne, PA
National Committee for Clinical Laboratory Standards (1993) Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Approved standard M7-A2, 2nd edn. Villanova, PA
SAS Institute (2004) Statistical analysis system user's guide, 7th edn. SAS Institute, Cary, NC
Wainwright M (1998) Photodynamic antimicrobial chemotherapy (PACT). J Antimicrob Chemother 42:13–28
Wilson M, Pratten J (1995) Lethal photosensitization of Staphylococcus aureus in vitro: effect of growth phase, serum, and pre-irradiation time. Lasers Surg Med 16:272–276
Wilson M, Burns T, Pratten J, Pearson GJ (1995) Bacteria in supragingival plaque samples can be killed by low-power laser light in the presence of a photosensitizer. J Appl Bacteriol 78:569–574
Tang HM, Hamblin MR, Yow CM (2007) A comparative in vitro photoinactivation study of clinical isolates of multidrug-resistant pathogens. J Infect Chemother 13(2):87–91
Packer S, Bhatti M, Burns T, Wilson M (2000) Inactivation of proteolytic enzymes from Porphyromonas gingivalis using light-activated agents. Lasers Med Sci 15:24–30
Sharma M, Visai L, Bragheri F, Cristiani I, Gupta PK, Speziale P (2008) Toluidine blue-mediated photodynamic effects on staphylococcal biofilms. Antimicrob Agents Chemother 52(1):299–305
Lin J, Bi LJ, Zhang ZG, Fu YM, Dong TT (2010) Toluidine blue-mediated photodynamic therapy of oral wound infections in rats. Lasers Med Sci 25(2):233–238
Embleton ML, Nair SP, Cookson BD, Wilson M (2002) Selective lethal photosensitization of methicillin-resistant Staphylococcus aureus using an IgG-tin (IV) chlorin e6 conjugate. J Antimicrob Chemother 50:857–864
Wakayama Y, Takagi M, Yano K (1980) Photosensitized inactivation of E. coli cells in toluidine blue-light system. Photochem Photobiol 32:601–605
Girotti AW (1990) Photodynamic lipid peroxidation in biological systems. Photochem Photobiol 51:497–509
Miranda MA (2001) Photosensitization by drugs. Pure Appl Chem 73:481–486
Komerik N, Nakanishi H, MacRobert AJ, Henderson B, Speight P, Wilson M (2003) In vivo killing of Porphyromonas gingivalis by toluidine blue-mediated photosensitization in an animal model. Antimicrob Agents Chemother 47:932–940
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hajim, K.I., Salih, D.S. & Rassam, Y.Z. Laser light combined with a photosensitizer may eliminate methicillin-resistant strains of Staphylococcus aureus . Lasers Med Sci 25, 743–748 (2010). https://doi.org/10.1007/s10103-010-0803-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-010-0803-z