Abstract
Group A streptococcal (GAS) pharyngitis is responsible for 20–30% of pharyngitis cases in children (Shulman et al. Clin Infect Dis 55(10):e86–e102, 2012). Recommendations for the diagnosis and treatment of GAS pharyngitis have been published by the Italian National Institute of Health guidelines in 2012 (ESCMID Sore Throat Guideline Group et al. Clin Microbiol Infect 18(Suppl 1):1–28, 2012). Adherence to such guidance is relevant for primary prevention of complications of GAS pharyngitis, above all rheumatic fever (RF). The aim of our study was to evaluate the application of Italian guidelines by the family pediatricians from the Abruzzo region. A validated questionnaire was completed by the family pediatricians and used for data collection. The 154 family pediatricians from Abruzzo (88% of the total number of family pediatricians) participated in the study. Out of the 1232 answers, 455 (37%) were wrong. Only 8% of the participants answered correctly all the questions, whereas 0.6% missed all the questions. Through the Spearman’s correlation, our study found an inverse significant correlation between the questions regarding primary prophylaxis (Score B) and the work experience of pediatricians (Rho = − 0.276, p = 0.048). The majority of the family pediatricians from the Abruzzo region, in line with studies from other countries, have significant knowledge gaps about the diagnosis and treatment of GAS pharyngitis. Therefore, strategies to increase the pediatricians’ awareness of the guidelines are needed, in order to reduce the RF incidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Group A streptococcal (GAS) pharyngitis is responsible for 20–30% of pharyngitis cases in children; it occurs most commonly between 5 and 15 years of age [1, 2]. Discrepancies in the management of GAS pharyngitis in children have been reported in Europe and in the USA. The main differences concern the diagnostic approach and the indication for antibiotic therapy; indeed, some national guidelines indicate the use of antibiotic prophylaxis only for high-risk patients with streptococcal pharyngitis [3]. Recommendations for the diagnosis and treatment of GAS pharyngitis have been published by the Infectious Disease Society of America (IDSA) [1] and The European Society for Clinical Microbiology and Infectious Disease (ESCMID) Sore Throat Guidelines[3] in 2012 and endorsed by the Italian National Institute of Health guidelines [4]. Adherence to such guidance is relevant in view of an effective primary prevention of complications of GAS pharyngitis, above all rheumatic fever (RF). RF accounts for most cases of acquired heart disease in children and young adults in developing countries; moreover, in recent years, a resurgence of the disease has been documented also in developed countries [2, 5].
The aims of our study were as follows: i) to evaluate the application of Italian guidelines (IG) by the family pediatricians from the Abruzzo region (central Italy); ii) to investigate the rational use of antibiotic therapy by the pediatricians and the compliance to antibiotic treatment.
Methods
The study was conducted in Abruzzo, a region of central Italy. Abruzzo is a mountainous region, divided into four provinces (L’Aquila, Pescara, Chieti, and Teramo), each one with a Local Health Unit (LHU).The region consists of a population of 1,311,580, of whom about 16.2% are children. A multiple choice questionnaire was used for data collection. It was derived from the Italian guidelines and was reviewed by one general pediatrician, one pediatric rheumatologist, and one statistician. It was firstly validated through a pilot study and completed by the family pediatricians singularly and autonomously. The questionnaire was divided into two parts: the first part included demographic data of gender, age, graduation year, and years of work as a family pediatrician, the second part was composed of eight questions regarding the diagnosis and management of GAS pharyngitis.
After agreeing to participate in the study through a telephone contact, the questionnaires were administered at every pediatrician’s clinic by the same interviewer who also provided explanations for each question. The participants were told that it was possible to provide only a correct answer. A point of one was assigned to each correct answer, while a point of zero was given to the others. The questionnaires were collected in the years 2017–2018 for a total of 6160 data. The collected data were stored in a password-protected database.
The questions administered to the participants in the study and the correct answers are reported below:
- 1.
Question 1: When you have a child with pharyngitis do you perform rapid test for GAS? Answer 1 Yes, I performed it in selected cases.
- 2.
Question 2: What do you think is the best for the diagnosis of GAS pharyngitis? Answer 2 Rapid test for GAS.
- 3.
Question 3: Which antibiotic do you use to treat GAS pharyngitis? Answer 3 Amoxicillin.
- 4.
Question 4: For how many days do you prescribe antibiotic therapy? Answer 4 10 days.
- 5.
Question 5: Do you recommend a microbiologic follow-up in children treated for GAS pharyngitis? Answer 5 No, never.
- 6.
Question 6: When you prescribe a throat swab, do you also, routinely, test antibiotic susceptibility? Answer 6 No, never.
- 7.
Question 7: What is the definition of GAS pharyngeal carrier state? Answer 7 A patient with a positive rapid test or throat swab for GAS and negative Antistreptolysin O titer and DNasi B antibodies.
- 8.
Question 8: How should GAS carrier be managed? Answer 8 No treatment should be performed.
Data analysis
The data collection was analyzed by grouping the family pediatricians in the participating provinces into four groups. The Kruskal–Wallis test was used to estimate the differences among provinces. The Spearmen’s correlation was applied to evaluate the relation between work experience (years) and guidelines adherence.
Data analysis was performed using the Statistical Package for the Social Sciences (SPSS), version 20.
A p value of less than 0.05 was considered as a significant statistical difference.
Results
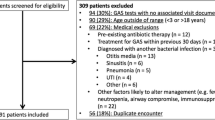
The 154 pediatricians from Abruzzo (88% of the total number of the pediatricians in Abruzzo) participated in the study: 44 were from Chieti, 44 from Pescara, 35 from Teramo, and 31 from L’Aquila.
The pediatricians were from the ages 51–68 years (mean age: 61.6 ± 3.3 years), with 60% of the sample being females. Work experience as family pediatricians ranged between a minimum of 24 years and a maximum of 38 (mean 31.1 ± 3.8 years).
Out of the 1232 answers, 455 (37%) were wrong. Figure 1 shows the percentages of correct and incorrect answers to all the questions. The majority of the pediatricians answered correctly to question 1, regarding the use of rapid test (RADT) for the diagnosis of GAS pharyngitis only in selected cases. 18% of the interviewed gave an incorrect answer to question 1 according to the IG.
The right responders to question 2 were 60% of the pediatricians. Out of the incorrect responders, 32% prescribe directly a culture test, 4% the anti-DNAsi B, and 4% the ASLO titer. For question 3, only 34% of the pediatricians responded correctly, that is, they use amoxicillin to treat GAS pharyngitis. The most of pediatricians (55%) prescribe amoxicillin and clavulanic acid, 9% cephalosporins, and 2% macrolides.
Responses to question 4 were mostly correct as 88% of the pediatricians recommend a 10-day course treatment for GAS pharyngitis, 8% believe that 7 days of therapy are sufficient, 2% prescribe a 6-day therapy, and 1% a 5-days therapy. Only 1% of the respondents prolong the treatment to 15 days.
43% of the pediatricians do not perform a microbiologic follow-up (question 5), after treatment of GAS pharyngitis, 33% perform it in selected cases, 15% prescribe it to every child affected, and 9% sometimes. On question 5, concerning the control swab at the end of the treatment, the pediatricians responded as follows: 42% believe it is useful only in selected cases, 13% believe that it is always essential, and 3% were undecided, whereas only 42% of them gave the correct response.
Question 6 regarded the demand for the antibiotic susceptibility: 58% of the pediatricians interviewed require the test of antibiotic susceptibility, of these 19% in every case, 21% only in selected cases, and 18% only in cases of suspected antibiotic resistance. 42% of the pediatricians responded correctly to question 6. Questions 7 and 8 deal with the diagnosis and management of the GAS carrier state: 73% of the respondents agreed with the guidelines about the definition of carrier state, and 27% gave the wrong response. 81% responded correctly to question 8 regarding the treatment of pharyngeal GAS carrier; they agreed with the guidelines asserting that the carrier state should not be treated, 11% believed it should be treated with amoxicillin, 3%with benzathine penicillin, and the remainders with other antibiotics.
According to the scores obtained, only 8% of the participants answered correctly to all the questions, obtaining a score of 8/8 (Score A), whereas 0.6% obtained a score of 0/8, missing all the questions. 40.8% of the pediatricians answered to half or less of the questions (Score A ≤ 4), whereas 52.2% responded correctly to more than half of them (Score A ≥ 4). When strictly analyzing questions regarding primary prophylaxis (question numbers 1, 3, and 4, Score B), 26% of the participants responded correctly to all the questions (Score B 3/3), while 0.6% missed all the three questions (Score B 0/3).
Guidelines adherence was stratified on the basis of the belonging LHU. The statistical analysis showed a significant difference for question numbers 2, 3, 5, 6, and 7 (Table 1). We analyzed the relationship of the work experience (years) on the guidelines adherence through the Spearman’s correlation, and no difference was found (Rho = − 0.020, p = 0.808); on the other hand, an inverse significant correlation was found between the Score B and the work experience (Rho = − 0.276, p = 0.048).
Discussion
In our study we found that only 8% of the family pediatricians from the Abruzzo region have 100% adherence to IG for the diagnosis and treatment of GAS pharyngitis. Questions strictly regarding primary prophylaxis of RF obtained 26% of adherence (score B). These data are in line with the previous studies showing low adherence rates of the pediatricians and physicians from different countries [6,7,8,9].
Hedin et al., in an interview study of 25 selected pediatricians from Sweden, demonstrated that only one-third of the interviewed were adherent to the current Swedish guidelines for sore throat [6]. Similar results were found by Alkhazi et al. in another interview study of the 243 physicians of the Pediatric Emergency Department from Saudi Arabia [7]. The authors conclude emphasizing the importance of local guideline implementation to reduce GAS pharyngitis sequelae, the most important being RF [6, 7]. RF and rheumatic heart disease remain significant issues in developing countries although a re-emergence of the disease in industrialized countries has been documented in recent years [2, 10,11,12]. Another issue emerging from our study regards the antibiotic used for the treatment of GAS pharyngitis. The IG recommend penicillin or amoxicillin as the first choice in non-allergic patients and recommend first generation cephalosporin, clindamycin, and macrolides as alternatives in allergic patients [4]. The results of the present study show that only 34% of the respondents utilize amoxicillin, whereas more than 50% use amoxicillin and clavulanic acid. Moreover, 63% of the interviewed tend to prescribe a microbiologic follow-up. IG do not recommend microbiologic follow-up as the majority of children with GAS pharyngitis respond clinically to penicillin/amoxicillin treatment, and GAS is eradicated from the pharynx [4].
The most important limitation of our study is that there is no report of actual sore throat management by the interviewed pediatricians: a link between what one says and what one does may not always be coherent. However, the study offers an overall view of the problem especially if we consider that Abruzzo, according to epidemiologic studies performed in the last 20 years, is a region with a medium–high incidence of RF [2].
In conclusion, the majority of the family pediatricians from the Abruzzo region, in line with studies from other countries, have significant knowledge gaps about the diagnosis and treatment of GAS pharyngitis.
Implementation of guidelines through repeated information among the family pediatricians would be desirable in order to reduce the cases of rheumatic carditis and improve the current problem of antibiotic resistance. Further studies are needed to determine the most effective strategies to increase pediatricians’ awareness and improve guideline adherence.
Abbreviations
- GAS:
-
Group A streptococcus
- IDSA:
-
Infectious Disease Society of America
- IG:
-
Italian guidelines
- LHU:
-
Local Health Unit
- RADT:
-
Rapid antigen detection test
- RF:
-
Rheumatic fever
- SPSS:
-
Statistical Package for the Social Sciences
References
Shulman ST, Bisno AL, Clegg HW, Gerber MA, Kaplan EL, Lee G, Martin JM, Van Beneden C (2012) Clinical practice guideline for the diagnosis and Management of Group a Streptococcal Pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis 55(10):e86–e102
ESCMID Sore Throat Guideline Group, Pelucchi C, Grigoryan L, Galeone C, Esposito S, Huovinen P, Little P, Verheij T. Guideline for the management of acute sore throat. Clin Microbiol Infect. 2012 Apr;18 Suppl 1:1–28
Chiappini E, Principi N, Mansi N et al (2012) Italian panel management of acute pharyngitis in children: summary of the Italian National Institute of health guidelines. Clin Ther 34:1442–1458
Breda L, Marzetti V, Gaspari S, Del Torto M, Chiarelli F, Altobelli E (2012) Population-based study of incidence and clinical characteristics of rheumatic fever in Abruzzo, Central Italy, 2000-2009. J Pediatr 160:832–836
Pastore S, De Cunto A, Benettoni A, Berton E, Taddio A, Lepore L (2011) The resurgence of rheumatic fever in a developed country area: the role of echocardiography. Rheumatology 50:396–400
Hedin K, Strandberg EL, Gröndal H, Brorsson A, Thulesius H, André M (2014 Dec) Management of patients with sore throats in relation to guidelines: an interview study in Sweden. Scand J Prim Health Care 32(4):193–199
Alkhazi AA, Alessa KM, Almutairi AM, Almadi HA, Akkam A, Almutairi MK, Alhamad OA, Ghazal HS (2018 Nov 16) Improving pediatric emergency department physicians' adherence to clinical practice guidelines on the diagnosis and management of group a betahemolytic streptococcal pharyngitis-a cross-sectional study. Int J Emerg Med 11:49
Brennan-Krohn T, Ozonoff A, Sandora TJ (2018 Feb 9) Adherence to guidelines for testing and treatment of children with pharyngitis: a retrospective study. BMC Pediatr 18(1):43
Norton LE, Lee BR, Harte L, Mann K, Newland JG, Grimes RA, Myers AL. Improving guideline-based streptococcal pharyngitis testing: a quality improvement initiative. Pediatrics. 2018 Jul;142(1). pii: e20172033
Milne RJ, Lennon DR, Stewart JM, Vander Hoorn S, Scuffham PA (2012) Incidence of acute rheumatic fever in New Zealand children and youth. J Paediatr Child Health 48:685–691
Lawrence JG, Carapetis JR, Griffiths K, Edwards K, Condon JR (2013) Acute rheumatic fever and rheumatic heart disease: incidence and progression in the Northern Territory of Australia, 1997 to 2010. Circulation 128:492–501
Karthikeyan G, Guilherme L (2018) Acute rheumatic fever. Lancet 392:161–174
Author information
Authors and Affiliations
Contributions
DM I: Collected the data.
d’ADM: Wrote the paper.
DB C: Wrote the paper.
L G: Collected the data.
Z I: Performed the analysis.
B L: Conceived and designed the analysis.
AE: Contributed data or analysis tools.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all the individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
What is known:
• Adherence to recommendations for the management of GAS pharyngitis is relevant for an effective primary prevention of rheumatic fever (RF).
• In recent years, a resurgence of RF has been documented also in developed countries.
What is new:
• The majority of the family pediatricians from the Abruzzo region in Italy, in line with other countries, have significant knowledge gaps about the adherence to pharyngitis guidelines.
• Repeated information among the family pediatricians is needed in order to prevent rheumatic heart disease.
Rights and permissions
About this article
Cite this article
Di Muzio, I., d’Angelo, D.M., Di Battista, C. et al. Pediatrician’s approach to diagnosis and management of group A streptococcal pharyngitis. Eur J Clin Microbiol Infect Dis 39, 1103–1107 (2020). https://doi.org/10.1007/s10096-020-03821-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-020-03821-y