Abstract
Diagnostic uncertainty is common in the emergency room and multidrug-resistant bacteria emerge in the community setting, implying to establish the most efficient empirical antibiotic therapy (eEAT). Our aim was to identify such eEAT, considering that in case of DU with severe clinical presentation, most prescribers would propose an empiric combination (EC). The medical dashboard of our ward records prospectively 28 characteristics of each hospitalization including hospitalization motive, final diagnosis, and all antibiotics prescribed. All patients with community-acquired bacteremia (CAB) were included. DU was defined by a discrepancy between suspected diagnosis in the emergency room and final diagnosis. eEAT was defined by in vitro activity of at least one prescribed compound. Finally, independently from the dashboard, we retrospectively compared 2 CTs: amoxicillin/clavulanic acid (AMC)+gentamicin (G) and cefotaxime (3GC)+G. One thousand thirty-four patients with a final diagnosis of CAB were identified from July 2005 to June 2018, including 357 DU (35%) at baseline. eEAT (n = 553) was associated with a trend towards a lower death rate compared to inefficient therapies: 5.4 vs 10.0% (p = 0.053), and effective antibiotic reassessment was the most protective factor against an unfavorable outcome: 0.34 (0.16–0.71). Bacteria involved in case of UD were resistant to AMC+G and to 3GC+G in 8.1% and 12.8% of patients, respectively. Diagnostic uncertainty was a frequent event requiring antibiotic reassessment. As the latter was not systematically realized, the best eEAT is required and AMC+aminoglycoside should be considered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Patients managed in the emergency room can be considered as having infection and requiring prompt antibiotic treatment because of organ failure. However, frequently the primary focus may remain unknown during the first hours after admission: 10 to 30% of patients do not have a definitive diagnosis following first clinical evaluation, which in turn has a negative impact on the final outcome [1,2,3,4,5]. No guidelines are available to help the clinician in such situation to choose the most appropriate treatment.
Due to antibiotic misuse, multidrug-resistant (MDR) bacteria have become a widespread concern in clinical medicine [6]. Several guidelines now take into consideration the risk of MDR bacteria involvement for antibiotic choice during empirical treatment [7, 8], even in the community setting. However, MDR bacteria prevalence is highly variable, depending on both patient-related and environmental factors [6, 8]. Data on MDR bacteria in the context of community-acquired infections are scarce except for cutaneous infections in the USA and urinary infections worldwide [2, 7, 9, 10].
The conjunction of diagnostic uncertainty with the background of enhanced rate of MDR bacteria leads the clinician to prescribe a combination of antibiotics as empirical treatment, especially if organ dysfunction is observed [11,12,13]. Based on microbiological data of bacteremic patients in the community setting, we aimed to identify the most suitable antibiotic combination for patient with diagnostic uncertainty, therefore at risk for unfavorable outcome.
Methods
Patient selection and characteristics
This was an observational study realized in Nice University Hospital, a tertiary care center with only one infectious diseases department. It was based on our medical dashboard, which was put into practice since July 2005 and previously described in [2, 3]. This dashboard works as a database, declared and approved by the French Data Protection Authority number 1430722.
As the software allows diagnosis or diagnosis-related group (DRG) selection, it is easy to study the main patient’s characteristics and evolution of a specific disease. Regarding severity, terminology used in patient’s final report was translated in the dashboard.
We included all patients with community-acquired bacteremia from July 2005 to June 2018.
Diagnostic uncertainty (DU) was defined by a discrepancy between diagnosis suspected at admission and final diagnosis at discharge. This definition included patients for whom no clear diagnosis appeared as the reason for hospitalization, e.g., mostly fever of unknown origin.
Bacteriological studies
We specifically checked in the patient’s chart the accuracy of the blood culture results and the community-acquired infection characteristics when the bacteria isolated was usually involved in nosocomial infections, such as ESBL-producing Enterobacteriaceae and Pseudomonas aeruginosa. All polymicrobial blood cultures were also assessed in the patient’s chart.
Blood cultures were collected directly during the venipuncture procedure using aerobic (Bact/AERT® FA Plus, Biomérieux, France) and anaerobic (Bact/AERT® FN Plus, Biomérieux, France) blood culture bottles, and were then sent to the laboratory and processed with an automated Bact/ALERT 3D system (BioMérieux, France). Specific culture for Mycobacterium spp. was also performed if clinically suspected. Bottles that showed a positive signal in the Bact/ALERT 3D system were routinely subjected to Gram staining and subcultured at least on blood agar plates and upon results of Gram on Drigalski agar or on chocolate agar. Colonies were identified using the API system (bioMérieux) and, since 2013, MALDI-TOF MS Microflex LT (Bruker Daltonics GmbH, Bremen, Germany) according to the manufacturer’s recommendation. Antibiograms were carried out by the diffusion method in Mueller-Hinton agar (MH BioMerieux SA, Marcy-l’Étoile, France) with BioRad discs (Marnes-la-Coquette, France) and interpreted according to the Antibiogram Committee of the French Microbiology Society recommendations using the Sirweb (I2A) software. Synergy was observed by placing third generation cephalosporin discs around discs containing clavulanic acid.
We specifically recorded microbial data regarding in vitro susceptibility to amoxicillin/clavulanic acid (AMC), cefotaxime or ceftriaxone (3GC), gentamicin (G), and their combinations, AMC+G and 3GC+G.
According to recent consensual definitions [14], inappropriate antibiotic therapy was defined as the use of antimicrobials to which the pathogen was resistant.
An effective antibiotic reassessment was defined as any modification (including the first introduction) of the initial antibiotic treatment, irrespective of the time of change.
Unfavorable outcome was defined as patient death during the hospital stay.
Statistical analysis
Data were analyzed with StatView software version 5.0 and statistical significance was established at α = 0.05. Continuous variables were compared with the Student’s t test or the Mann–Whitney non-parametric test. Proportions were compared with the χ2 statistic or Fisher’s exact test when appropriate. Logistic regression was used to determine in multivariate analysis the risk factor for all-cause in-hospital mortality. The results are presented as adjusted odds ratios (AORs), along with their 95% confidence intervals (CIs).
Results
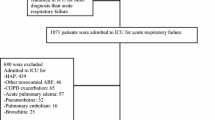
Patient selection is described in Fig. 1. A total of 1034 CAB were included from July 2005 to June 2018, representing 8.7% of all community-acquired infections admitted in our department that had blood cultures collected.
Main patient characteristics are presented in Table 1, according to diagnostic accuracy. Diagnostic uncertainty was observed for 357 patients (35%), mainly in respiratory infections DRG: 57/149 (38%). Also, these diagnostic uncertainties included 164/357 (46%) patients presented with fever of unknown origin. Regarding antibiotic treatment, 7 patients died before any therapeutic prescriptions, including 2 patients benefiting of palliative care; there were analyzed as inefficient treatment. Efficient empirical antibiotic treatment (eEAT) was observed in 924 cases (89%) and was less frequent in case of uncertain diagnosis: 87% vs 91%, p = 0.055. The rate of antibiotic reassessment (2 antibiotic treatments prescribed successively) was 53% (see Table 1).
Unfavorable outcome was observed in 61 cases (5.8%). Risk factors for unfavorable outcome are shown in Table 2. eEAT (n = 553) was associated with a lower death rate compared to inefficient therapies without reaching statistical significance: 5.4 vs 10.0% (p = 0.053). Urinary source of CAB and effective antibiotic reassessment were protective factors of unfavorable outcome: AOR = 0.42, p = 0.003 and 0.34, p = 0.012 respectively. In contrast, neurological and/or psychiatric co-morbid conditions were associated with unfavorable outcome: AOR = 3.05, p < 0.001, as well as severe forms of infections: AOR = 5.09, p < 0.001, and ESBL positive strains bacteremia: AOR = 7.48, p < 0.001.
As eEAT was consistent with a protective factor for unfavorable outcome, but was also inconstant, the question was the determination of the best empirical therapy. Blood culture results as well as susceptibility to both antibiotic combinations AMC+G and 3GC+G are indicated in Table 3. As expected, Enterobacteriaceae were predominant, accounting for 437 cases (42%), including 56 ESBL-producing strains (13%). Streptococci were more frequently isolated (21%) than Staphylococcus aureus (16%), among which only 3 cases of methicillin resistant S. aureus were detected. Of note, polymicrobial CAB amounted to 10% of the cases. In vitro data indicates that 250 bacteria were resistant to AMC (24%), 201 were resistant to 3GC (19%) and 376 were resistant to G (36%). Among the 56 ESBL-producing strains, 24 were also resistant to G, but all were susceptible to amikacin. Considering antibiotic combination, 5.8% of bacteria were resistant to AMC+G and 10.1% were resistant to 3GC+G (see Tables 1 and 3). A total of 47 (4.5%) strains was resistant to both antibiotic combinations, in particularly 24 ESBL producing Enterobacteriaceae. Accordingly, based on in vitro antibiotic susceptibility data, the most efficient antibiotic combination in the subgroup of uncertain diagnosis was AMC+G compared with 3GC+G: 92% vs 87%.
Discussion
Our work confirms previous studies showing that uncertain diagnosis is frequent and associated with a trend towards inappropriate empirical antibiotic therapy [1, 2, 12, 13]. Also, effective antibiotic reassessment is associated with a better outcome [1, 12, 15, 16]. Therefore, our study designates the vicious circle between uncertain diagnosis, inappropriate empirical antibiotic therapy, and unfavorable outcome in the absence of antibiotic reassessment. Thus, defining the best empirical antibiotic combination for patients with uncertain diagnosis is of paramount importance, especially because antibiotic reassessment is still limited in real-life practice [1, 15]. As the first criteria of drug choice in empirical antibiotic therapy is determined through the in vitro susceptibility of the suspected bacteria, our data indicated that AMC+G was superior to 3GC+G. Moreover, the superiority of AMC+G was significant in the subgroup of patients with uncertain diagnosis, at least in part due to the resistance of enteroccocal infections and polymicrobial bacteremia to 3GC+G (see Tables 1 and 3).
One limit of our study is the monocentric characteristic of the resistance epidemiology, so the resluts will be applicable to geographical areas and health care facilities displaying the same rate of MDR bacteria in the community setting with a similar CAB epidemiology. For example, our results will be not relevent in the USA, where methicillin-resistant S. aureus is common, especially in skin and soft tissue infections [7]. Also, the choice for the aminoglycoside compound is not unequivocal: gentamicin is certainly a major molecule in combination with a penicillin for Gram-positive cocci such as streptococci, but amikacin is usually a more effective drug for ESBL-positive strains [17]. The negative impact of MDR bacteria such as ESBL-positive strains on the outcome has been reported and have to be considered even in the community settings [9, 18]. Lastly, in accordance with our results, the bacteremic urinary infections was associated with a better outcome compared to the digestive tract infections [18, 19]. We have previously reported that the AMC+aminoglycoside combination is also a good choice for primary bacteremia, defined by the absence of clinical diagnosis and fruitless investigations [20].
Conclusion
Our studies and others suggest that in front of diagnostic uncertainty, but still in the community setting, the empirical treatment of choice could be AMC+aminoglycosides. These results have to be further validated in a prospective comparative study in order to reduce the negative impact of diagnostic uncertainty.
Abbreviations
- AMC:
-
amoxicilline-clavulanic acid
- 3GC:
-
cefotaxime
- EC:
-
empiric combination
- CAB:
-
community acquired bacteremia
- DRG:
-
diagnosis-related group
- DU:
-
diagnostic uncertainty
- eEAT:
-
efficient empirical antibiotic therapy
- G 3GC:
-
gentamicin cefotaxime
- MDR:
-
multidrug-resistant
References
Aillet C, Jammes D, Fribourg A, Léotard S, Pellat O, Etienne P, et al (2018) Bacteraemia in emergency departments: effective antibiotic reassessment is associated with a better outcome. Eur J Clin Microbiol Infect Dis 37:325–31. https://doi.org/10.1007/s10096-017-3136-z
Roger P-M, Demonchy E, Risso K, Courjon J, Leroux S, Leroux E, et al (2017) Medical table: A major tool for antimicrobial stewardship policy. Med Mal Infect 47:311–8. https://doi.org/10.1016/j.medmal.2017.03.005
Denis E, Martis N, Guillouet-de-Salvador F (2016) Bacteraemic urinary tract infections may mimic respiratory infections: a nested case-control study. Eur J Clin Microbiol Infect Dis 1601–1605
Gavazzi G, Krause K-H (2002) Ageing and infection. Lancet Infect Dis 2:659–666
Filice AG, Drekonja DM, Thurn H JR, GM M, T J JR (2015) Diagnostic errors that lead to inappropriate antimicrobial use. Infect Control Hosp Epidemiol 949–956
Roca I, Akova M, Baquero F, Carlet J, Cavaleri M, Coenen S, et al (2015) The global threat of antimicrobial resistance: science for intervention. New Microbes New Infect 6:22–9. https://doi.org/10.1016/j.nmni.2015.02.007
Sartelli M, Malangoni MA, May AK, Viale P, Kao LS, Catena F, et al (2014) World Society of Emergency Surgery (WSES) guidelines for management of skin and soft tissue infections. World J Emerg Surg 9:57. https://doi.org/10.1186/1749-7922-9-57
Barlam TF, Cosgrove SE, Abbo LM, MacDougall C, Schuetz AN, Septimus EJ, et al (2016) Implementing an Antibiotic Stewardship Program: Guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis 62:e51-77. https://doi.org/10.1093/cid/ciw118
Zahar J-R, Lesprit P, Ruckly S, Eden A, Hikombo H, Bernard L, et al (2017) Predominance of healthcareassociated cases among episodes of community-onset bacteraemia due to extended-spectrum ß-lactamase-producing Enterobacteriaceae. Int J Antimicrob Agents 49:67–73. https://doi.org/10.1016/j.ijantimicag.2016.09.032
Rogers BA, Sidjabat HE, Paterson DL (2011) Escherichia coli O25b-ST131: a pandemic, multiresistant, community-associated strain. J Antimicrob Chemother 66:1–14. https://doi.org/10.1093/jac/dkq415
Vazquez-Grande G, Kumar A (2015) Optimizing antimicrobial therapy of sepsis and septic shock: focus on antibiotic combination therapy. Semin Respir Crit Care Med 36:154–66. https://doi.org/10.1055/s-0034-1398742
Vallés J, Rello J, Ochagavía A, Garnacho J, Alcalá MA (2003) Community-acquired bloodstream infection in critically ill adult patients: impact of shock and inappropriate antibiotic therapy on survival. Chest 123:1615–24
Marchaim D, Zaidenstein R, Lazarovitch T, Karpuch Y, Ziv T, Weinsberger M (2008) Epidemiology of bacteremia episodes in a single center: increase in gram-negative isolates, antibiotics resistance and patient age. Eur J Mircobiol Infect Dis 27(11):1045–51. https://doi.org/10.1007/s10096-008-0545-z
Spivak ES, Cosgrove SE, Srinivasan A (2016) Measuring Appropriate Antimicrobial Use: Attempts at Opening the Black Box. Clin Infect Dis 63:1639–44. https://doi.org/10.1093/cid/ciw658
Braykov N, Morgan DJ, Schweizer. ML et al (2014) Assessment of empirical therapy in six hospitals: an observational cohort study. Lancet Infect Dis 1220–7
Shallcross LJ, Freemantle N, Nisar S, Ray D (2016) A cross-sectional study of blood cultures and antibiotic use in patients admitted from the Emergency Department: missed opportunities for antimicrobial stewardship BMC Infect Dis 16:166. https://doi.org/10.1186/s12879-016-1515-1
Winokur PL, Canton R. Casellas JM, Legakis N. (2001) Variations in the prevalence of strains expressing an extended-spectrum beta-lactamase phenotype and characterization of isolates from Europe, the Americas, and the Western Pacific region. Clin Infect Dis 32(Suppl 2):s94–103
Russo A, Falcone M, Gutiérrez-Gutiérrez B, Calbo E, Almirante B, Viale PL, et al (2018) Predictors of outcome in patients with severe sepsis or septic shock due to extended-spectrum ß-lactamase-producing Enterobacteriaceae. Int J Antimicrob Agents 52:577–85. https://doi.org/10.1016/j.ijantimicag.2018.06.018
Lefort A, Panhard X, Clermont O, Woerther P-L, Branger C, Mentré F, et al (2011) Host factors and portal of entry outweigh bacterial determinants to predict the severity of Escherichia coli bacteremia. J Clin Microbiol 49:777–783. https://doi.org/10.1128/JCM.01902-10
Courjon J, Demonchy E, Degand N, Risso K, Ruimy R, Roger P-M (2017) Patients with community-acquired bacteremia of unknown origin: clinical characteristics and usefulness of microbiological results for therapeutic issues: a single-center cohort study. Ann Clin Microbiol Antimicrob 16:40. https://doi.org/10.1186/s12941-017-0214-0
Availability of data
The dataset used during the current study is available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
Study concept and design, PMR; acquisition of subjects, JC, ED, DC, CM, ND; analysis and interpretation of data, JC, PMR; preparation of manuscript, JC, ND, PMR.
Corresponding author
Ethics declarations
Conflict of interest
All of the authors declare that they have no conflicts of interest.
Ethical approval and consent to participate
The antibiotic audit was sponsored by the French National Health Agency. The patients or their relatives provided written consent for computerization of their personal data for hospitalization purposes and clinical research.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Courjon, J., Chirio, D., Demonchy, E. et al. Amoxicillin/clavulanic acid+aminoglycoside as empirical antibiotic treatment in severe community-acquired infections with diagnostic uncertainty. Eur J Clin Microbiol Infect Dis 38, 895–901 (2019). https://doi.org/10.1007/s10096-019-03496-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-019-03496-0