Abstract
Candida spp. usually colonize ulcerative lesions of atrophic mucosa in patients with chemotherapy-induced oral mucositis inducing severe inflammation. The spread of antifungal-resistant strains strongly encouraged the search of complementary or alternative therapeutic strategies to cure inflamed mucosa. In this paper, we studied the effects of a near-infrared (NIR) laser system with dual-wavelength emission (808 nm + 904 nm) on the survival and inflammatory potential of C. albicans, C. glabrata, and C. parapsilosis. Laser treatment was performed with a Multiwave Locked System laser. Survival and apoptosis of fungal strains were evaluated by colony-forming units (CFU) counting and annexin V staining. Cytokine production was evaluated by ImmunoPlex array. Laser treatment significantly affected the survival of Candida spp. by inducing apoptosis and induced a lower production of inflammatory cytokines by dendritic cells compared to untreated fungi. No differences in the survival and inflammatory potential were recorded in treated or untreated Saccharomyces cerevisiae cells, used as the control non-pathogenic microorganism. Laser treatment altered the survival and inflammatory potential of pathogenic Candida spp. These data provide experimental support to the use of NIR laser radiation as a co-adjuvant of antifungal therapy in patients with oral mucositis (OM) complicated by Candida infections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chemotherapy-induced oral mucositis (OM) are frequently complicated by infections with Candida spp. [1, 2], in particular with C. albicans. Recently, however, C. glabrata, C. tropicalis, and C. parapsilosis were also shown to be involved in the clinical course of OM [3]. The ulcerative lesions of atrophic mucosa represent an ecological niche optimal for the growth of pathogenic microorganisms, including opportunistic fungi, and the infection-induced inflammatory process significantly worsens the clinical symptomatology, leading to the appearance of white spots over inflamed areas. Pain, mouth irritation, and a burning sensation might have a great impact on the patient’s well-being, affecting taste and the ability to eat and/or speak. Antifungal therapy is the first choice of treatment and it is strongly recommended [4]. However, the spread of resistance to common chemotherapeutics (fluconazole) and the propensity of several fungal strains to form biofilms [2], representing an impermeable barrier to antifungal drugs, increase the difficulty in treating these patients. So, the search for alternative therapeutic strategies is highly encouraged.
Laser therapy, applied to the oropharyngeal area, was reported to be as effective in the prevention of OM and in the reduction of severity, pain, and duration of OM ulcers [5, 6]. In these studies, treatments have been performed by using a wide range of sources, differing in power (class I–III lasers, with power lower than 0.5 W, and class IV lasers, with power higher than 0.5 W), wavelength [mostly in the red and near-infrared (NIR) bands], and emission (single and combined, continuous and pulsed mode). Although some studies reported an increase in the mortality of C. albicans in vitro [7–9], the molecular and cellular mechanisms underlying the effects of laser therapy on microorganisms and host tissues remain largely unknown. Recently, the effects of two treatment protocols differing in wavelength (λ 635 nm versus λ 970 nm) and energy density (0.375 J/cm2 versus 375 J/cm2) have been studied and compared in an animal model of chemotherapy-induced OM. Both treatments were effective in curing OM lesions; however, a better healing and a marked decrease in inflammation was reported in subjects treated with the higher energy density, suggesting its potential clinical application. In this study, however, the treatment parameters have been chosen without considering the direct effect of laser treatment on infectious agents complicating the clinical course of OM. Furthermore, the authors did not discuss that, beside the energy density, the treatments differed also for the wavelength, which is an important parameter in determining the chromophores involved and the therapeutic effects [10].
In the present study, we hypothesize that, beside the homeostasis of host tissues, laser therapy may affect pathogen survival and host inflammatory response, and that the combination of these effects could improve the clinical course of OM. Therefore, prospecting the use of a dual-wavelength, NIR laser system in patients with OM, we explored the effects of such laser emission on the survival and inflammatory potential of those Candida spp. (C. albicans, C. glabrata, C. parapsilosis) which frequently colonize the injured and inflamed tissues in OM patients [1, 2, 11].
Materials and methods
Reagents
Annexin V was from Roche Diagnostics (Mannheim, Germany). pNiFty2-luc NF-kB-inducible reporter plasmid, Zymosan, and lipopolysaccharide (LPS) were from InvivoGen (San Giuliano Milanese, Italy). RPMI 1640, penicillin/streptomycin (P/S), heat-inactivated fetal bovine serum (FBS), and DMEM 4.5 g/l glucose were from Celbio (Pero, Italy). Solid (YPD-A) and liquid (YPD) yeast culture media were from Sigma-Aldrich (Sigma-Aldrich Chemical Co., St. Louis, MO, USA). The Dual-Glo Luciferase Activity Kit was purchased from Promega (Madison, WI, USA). Human recombinant (hr) IL4 and hr GMCSF were from R&D (R&D Systems, Minneapolis, MN, USA). The multiplex immunoarray kit for cytokines assay was purchased from Millipore (Billerica, MA USA) .
Cultures
Yeasts: C. albicans (SC53-14, ATCC MYA-2876), C. parapsilosis (YA4), C. glabrata (YUC23), and Saccharomyces cerevisiae (S288c) strains were grown in agar plates (YPD-A, bacteriological peptone 20 g/L, yeast extract 10 g/L, glucose 20 g/L, agar 15 g/L) at 28 °C for about 2 days. Fungal colonies were cultured in liquid broth medium (YPD, bacteriological peptone 20 g/L, yeast extract 10 g/L, glucose 20 g/L) at 28 °C for 18 h before the treatment.
Cells: HEK-293-hTLR4/CD14/MD2 and HEK-293-hTLR2 were stably transfected with pNiFty2-luc NF-kB-inducible reporter plasmid by electroporation (355 V for 10 ms) and maintained in DMEM 4.5 g/L supplemented with 10 % FBS.
Laser treatment
The treatments were performed with a Multiwave Locked System (MLS) laser (Mphi, ASA Srl, Arcugnano, VI, Italy), a commercial laser source built in compliance with EC/EU rules, approved by the U.S. Food and Drug Administration (FDA), as previously reported [12]. The MLS is a class IV NIR laser with two synchronized sources (laser diodes). The two modules have different wavelengths, peak power, and emission mode. The first is the pulsed laser diode, emitting at 905 nm, with 25 W peak optical power; each pulse is composed of a pulse train (100 ns single pulse width, 90 kHz maximum frequency). The frequency of the pulse trains may be varied in the range 1–2000 Hz, thus varying the average power delivered to the tissue. The second laser diode (808 nm) may operate in continuous (power 1.1 W) or frequency mode (repetition rate 1–2000 Hz), 550 mW mean optical power output, duty ratio 50 % independently of the repetition rate. The two laser beams work simultaneously, synchronously, and the propagation axes are coincident.
For laser treatment, cells were harvested after 18 h of culture, washed twice in distilled water, and plated in triplicate in 24 well/plates at 107 cells/ml. Plates were placed inside a holder to allow controlled scan treatment; they were aligned with the hand piece, sliding in an overlying track, at a distance of 2 cm from the bottom of the wells, so that the spot of the two superimposed laser beams, impinging perpendicular to the sample surface, had the same diameter as a well (13 mm). A single experienced operator performed all the treatments. The scan of the samples was performed manually by moving the hand piece with a speed of 5.6 cm/s, under the guide of a metronome. The treatment was administered in sterile conditions and included two exposures to laser radiation, with a 1-h interval. The scan mode for treatment was chosen to mime treatment conditions often used in clinics.
Four treatment protocols differing in exposure time and total energy delivered were tested (Table 1).
Count of colony-forming units
Soon after treatment, 100 μL from each fungal culture was diluted to 1:100,000 and plated in triplicate in YPD-A at 28 °C. Colony-forming units (CFU) were counted after 24 and 48 h. Untreated or heat-killed (95 °C for 15 min) fungal cells were used as controls.
Isolation and maturation of dendritic cells
To obtain monocyte-derived dendritic cells (MDDC), CD14+ cells, purified from the peripheral blood of healthy donors, were cultured in the presence of 20 ng/ml of hr IL4 and 50 ng/ml of hr GMCSF (R&D) at 37 °C in a humidified chamber with 5 % CO2 for 5 days [13]. Non-adherent cells were stimulated for 16 h with treated or untreated fungal strains.
Toll-like receptors (TLRs) assay
HEK-293-hTLR4/CD14/MD2 and HEK-293-hTLR2 cells, stably transfected with pNiFty2-luc plasmid, plated in DMEM/FBS in 96 wells at 2 × 105/well and stimulated with 105 heat-killed (95 °C for 15 min), laser-treated (200 J, with 1500 Hz frequency), or untreated cells of Candida spp. (C. albicans, C. glabrata, C. parapsilosis) and of S. cerevisiae. Zymosan (100 μg/ml) or LPS (50 ng/ml) were used as positive controls for TLR2 and TLR4, respectively. Luciferase activity was measured 8 h later by the Dual-Glo Luciferase Assay System (Promega).
Cytokines assay
IL1-β, IL6, IL12p70, and IL-23 concentrations in MDDC culture supernatants were determined by using the Milliplex kit and Bio-Plex apparatus, according to the manufacturer’s recommendations.
Annexin V/PI labeling
C. albicans, C. parapsilosis, C. glabrata, and S. cerevisiae strains were cultured overnight in YPD at 28 °C. 100 μl of culture were diluted in 4 ml of YPD for a further 4 h at 28 °C, washed, and split into three aliquots of 2 × 106 cells each. One aliquot was laser-treated (200 J, 1500 Hz). Untreated fungi or fungi treated with 175 mM acetic acid were used as controls. Fungi were treated with Zymolyase (2 μg/ml in H2O-P/S) at 37 °C for 30 min, washed, and stained for 20 min with 100 μl of FITC–annexin V/PI mix. Cytofluorimetric analysis was performed by the Accuri instrument. Ten thousand events for each sample were acquired. Data were analyzed by CFlow Plus software.
Results
Effect of different laser treatments on yeast survival
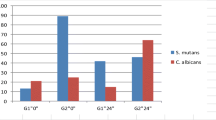
C. albicans (SC53-14, ATCC MYA-2876) and S. cerevisiae S288c strains [14] were used as representatives of pathogenic and non-pathogenic yeasts, respectively, and treated with different laser irradiation protocols, as indicated in Table 1. Figure 1 shows that all the tested protocols were able to decrease the number of CFU of C. albicans, while S. cerevisiae cells were not responsive to the treatments. Regarding C. albicans, the maximum effect in terms of mortality rate was reached with treatment protocol P3 (7 J/cm2).
Candida albicans and Saccharomyces cerevisiae strains were grown in YPD supplemented with 1 % yeast extract, 2 % peptone, and 2 % glucose for 18 h, plated in 24-well plates at 107/ml, and subjected to two exposures to laser radiation, with a 1-h interval. Four protocols differing in energy doses were tested. After treatment, 100 μl of 1:105 cellular dilutions were plated in triplicate in YPD agar and incubated at 28 °C. Data are shown as the mean count of colony-forming units (CFU) determined 2 days after treatment. The results from five different experiments [mean CFU ± standard error (SE)] are reported
Thus, treatment protocol P3 was chosen for the following experiments.
Effect of laser treatment on different Candida spp.
It is known that, besides C. albicans, different Candida spp., such as C. glabrata and C. parapsilosis, even more frequently complicate the clinical course of OM [11]. We, thus, wondered whether laser treatment (protocol P3) could affect the survival of these other Candida spp., as observed for C. albicans.
C. albicans, C. parapsilosis, C. glabrata, and S. cerevisiae cells were cultured and treated as reported above. Figure 2a shows that this treatment significantly reduced (40 %) the number of CFU for C. albicans and C. glabrata and, to a lesser extent (27 %), that of C. parapsilosis; again, S. cerevisiae was totally insensitive to laser radiation.
C. albicans, C. parapsilosis, C. glabrata, and S. cerevisiae cells were grown in YPD supplemented with 1 % yeast extract, 2 % peptone, and 2 % glucose for 18 h, plated in 24-well plates at 107/ml, and subjected to laser treatment (two exposures separated by a 1-h interval, energy density per exposure 7 J/cm2,, 1500 Hz frequency). The results are shown as percentage of decrease in CFU numbers detected 2 days after laser treatment. The data (mean ± SE) from 11 different experiments are shown. Statistical analysis was performed by Student’s t-test. p ≤ 0.05 was considered significant
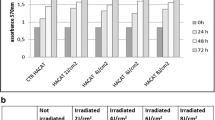
Effect of laser treatment on apoptosis
In order to understand the mechanism underlying the reduction in the CFU number, we investigated whether laser treatment induced apoptosis of fungal strains, evaluating by cytofluorimetric analysis the percentage of annexin V-positive cells. Figure 2b shows that laser radiation significantly increased apoptotic death in C. albicans and C. glabrata strains, while it leaves unaffected the survival of C. parapsilosis. Furthermore, laser treatment did not induce apoptosis in non-pathogenic S. cerevisiae cells.
Effect of laser treatment on the inflammatory potential of fungal cells
Infections with Candida spp. always induce the production of proinflammatory cytokines and chemokines by cells of innate immunity, which recruit inflammatory cells at the site of Candida invasion. Since laser treatment could induce biochemical changes in fungal recognition patterns, we investigated how fungal cells stimulate the production of inflammatory cytokines by MDDC before and after the treatment.
MDDC were cultured for 24 h with laser-treated or untreated Candida or S. cerevisiae strains. Heat-killed cells and LPS (50 ng/ml) were used as positive controls. At the end of the incubation, conditioned media were collected and the production of inflammatory cytokines was measured through multiplex immunoarray. Figure 3a shows that Candida spp. and S. cerevisiae were able to induce the production of the inflammatory cytokines IL-1β and IL-6. However, relevant differences in the induction of cytokine production by live, untreated cells from these species were recorded, with C. albicans inducing the lowest amounts, while S. cerevisiae always induced the maximal production of IL-1β and IL-6. As expected, the killed forms of the fungi (positive controls) induced a pattern of cytokine production different from that of their respective live (untreated) forms, likely reflecting changes in the exposure of cell wall components as a consequence of heat killing. Figure 3b shows that laser treatment significantly modulated the ability of C. glabrata and C. parapsilosis to induce IL-1β production by MDDC and further inhibited that of C. albicans cells. The production of IL-6 by MDDC was also decreased following the exposure of MDDC to irradiated pathogenic Candida spp. In contrast, the exposure to laser radiation left unaffected the ability of S. cerevisiae cells to induce IL-1β and IL-6 production by MDDC.
C. albicans, C. parapsilosis, C. glabrata, and S. cerevisiae cells were grown in YPD supplemented with 1 % yeast extract, 2 % peptone, and 2 % glucose for 18 h, plated in 24-well plates at 107/ml, and subjected to laser treatment (two exposures separated by a 1-h interval, energy density per exposure 7 J/cm2,, 1500 Hz frequency). Human monocyte-derived dendritic cells (MDDC), obtained through the differentiation of CD14+ circulating monocytes in the presence of IL-4 and GM-CSF, were cultured for 24 h with laser-treated or untreated C. albicans, C. parapsilosis, C. glabrata, and S. cerevisiae strains at the ratio of 1:10. Heat-killed (95 °C for 15 min) fungi and lipopolysaccharide (LPS; 50 ng/ml) were used as positive controls. At the end of incubation, conditioned media were collected and the production of inflammatory cytokines measured through multiplex immunoarray. a Production of IL-1β and IL-6 by dendritic cells stimulated with untreated (white columns) or heat-killed (black columns) Candida spp. S. cerevisiae. The results are shown as the mean cytokine production ± SE of six different experiments. b Box-and-whisker plots show IL1 and IL6 production by MDDC cultured with laser-treated (gray boxes) or untreated (white boxes) C. albicans, C. parapsilosis, C. glabrata, and S. cerevisiae strains. The data are representative of six different experiments. The boxes extend from the 25th percentile to the 75th percentile, with a horizontal line at the median (50th percentile). The whiskers indicate outliers. Statistical analysis was performed by the non-parametric Mann–Whitney test; p ≤ 0.05 was considered significant
Beside a species-dependent variability in inducing the production of inflammatory cytokines by cells of innate immunity, these data indicate that laser treatment could affect the inflammatory potential of pathogenic Candida spp., while leaving unaffected that of harmless yeast.
We also measured in the same culture supernatants the production of IL-12p70 and IL-23, two cytokines involved in T-helper (TH)-1 and TH-17 differentiation response, respectively [15]. We could not observe significant differences in the production of these cytokines by MDDC exposed to treated and untreated different fungal strains, suggesting that the development of the immune specific response could not be affected at least in immunocompetent hosts.
Effect of laser treatment on the ability of fungal cells to activate the TLR2 and TLR4 pathways
In MDDC, recognition of C. albicans at the level of the cell membrane is mediated by TLRs and C-type lectin receptors (CLRs). TLR4 mainly induces proinflammatory signals, while TLR2 induces a moderate proinflammatory response and a strong IL-10 production [16].
We, thus, investigated whether the exposure to laser radiation impaired the ability of Candida spp. and/or S. cerevisiae to activate TLR4 and TLR2 in specific assays, using HEK293 cells transfected with huTLR4 or huTLR2. Figure 4 shows that untreated Candida and S. cerevisiae fungal cells induced a slight stimulation of TLR4 activity. Laser treatment of fungal cells always decreases the ability to stimulate TLR4, but the differences between treated and untreated cells reached statistical significance only using C. albicans cells. In contrast, no differences were detected in TLR2 stimulation by treated fungal cells of any species compared to untreated cells (data not shown).
HEK-293-hTLR4/CD14/MD2 cells stably transfected with pNiFty2-luc NF-kB-inducible reporter plasmid were plated in 96 wells (2 × 105/well) and stimulated with 105 heat-killed (HK, black columns), laser-treated (gray columns), or untreated (white columns) cells of Candida spp. (C. albicans, C. glabrata, C. parapsilosis) and of S. cerevisiae for 8 h. Lipopolysaccharide (LPS) was used as the positive control. The data are shown as the TLR4 stimulation index calculated as the luciferase activity of stimulated HEK-293 cells by treated versus untreated yeast cells. Statistical analysis was performed by Student’s t-test and p ≤ 0.05 was considered significant
Discussion
Laser therapy, performed by using different laser sources and treatment parameters (low- or high-power laser sources, red or NIR wavelengths, continuous or pulsed modality), has been applied to the oropharyngeal area for the prevention and treatment of OM. The efficacy of treatment was reported in different studies with differences depending on sources and treatment parameters; laser therapy has been shown to be effective in the prevention of OM and in the reduction of the severity, pain, and duration of OM ulcers [5, 6], even in those induced by chemotherapy [10]. However, the direct effects of laser therapy on pathogens colonizing the atrophic mucosae have not been detailed and clinical studies do not consider this point in the choice of protocols.
This paper describes the effects of a dual-wavelength, NIR laser source (MLS laser) on the survival and inflammatory potential of C. albicans, C. glabrata, and C. parapsilosis, representing the most frequent pathogens complicating the clinical course of chemotherapy- or radiotherapy-induced OM. Our data clearly show that the selected treatment parameters (P3) significantly affected the survival of pathogenic Candida spp., while they left unaffected that of S. cerevisiae cells. A further increase in energy density (P4) did not correspond to an increase of effect (see Fig. 1).
The generation of reactive oxygen species (ROS), resulting from the absorption of laser radiation at the mitochondrial level, has been proposed as a major molecular mechanism underlying the photoinactivating action of laser therapy on microbial species, including C. albicans and Staphylococcus [9]. Indeed, increased ROS generation might be responsible for the induction of apoptosis observed in our experiments. This mechanism, however, could not explain the different outcomes in terms of survival activity (or residual CFU activity) induced by laser treatment in Candida spp. and S. cerevisiae, since common core mechanisms for oxidative stress response are shared by these fungal species [17–19]. In our opinion, the different sensitivities of fungal species to laser treatment could, at least in part, reside in structural and physicochemical features involved in the survival as well as in the virulence of pathogenic Candida spp. The fungal wall composition, easily to be involved in treatment sensitivity, varies between different fungal species and even among their strains. It also varies between filamentous fungus and yeast. The yeast-to-hypha transition, which does not occur in S. cerevisiae, leads to a major increase in the distribution, adhesion, unfolding, and extension of adhesins and their associated mannans [20, 21], and the process is usually accompanied by an increase in the exposure of mannosylation [20, 21]. It is reasonable that laser treatment affects the composition of structures which are more exposed during the transition from yeast to hyphae cells. Supporting this hypothesis are preliminary data, obtained in our laboratory, showing that cultures of Candida spp. in Sabouraud’s medium, which strongly prevents hyphae formation, are not sensitive to laser radiation in terms of survival impairment. Furthermore, clinical isolates of C. albicans with different capacities to form hyphae also differ in sensitivity to laser treatment (data not shown).
Beside the effects on survival of Candida spp., our data also show how laser treatment affects the inflammatory potential of Candida spp., while it leaves unaffected that of S. cerevisiae. According to different reports [22], we found relevant differences in the production of two inflammatory cytokines (IL-1β and IL-6) by human mature MDDC exposed to live fungal strains. In this system, C. albicans induced the lowest amounts of IL-1β and IL6, while S. cerevisiae induced much higher production of these cytokines. The fungal cell wall structure is composed of chitin, β-glucans, and mannoproteins, proteins with mannans covalently attached via ester linkages (O-linked mannans) or by amide bonds (N-linked mannans). Cells of innate immunity, including conventional mature MDDC, recognize fungal pathogen-associated molecular patterns (PAMPs) through TLRs and CLRs [23]. Since the hyphae formation process is accompanied by an increase in the exposure of mannans, different pattern recognition receptors (PRRs) could be engaged [20, 21]. Thus, once more, the dimorphic state of Candida spp., but not that of S. cerevisiae, could account for differences in cytokine production by mature MDDC. Recently, however, sugar moieties as β-1,2-mannosides of N-linked mannan, present in C. albicans but not in S. cerevisiae [24], have been reported as being responsible for the lower inflammatory potential of C. albicans compared to S. cerevisiae. C. albicans mutants lacking the N-linked mannan β-1,2-mannosides induced much higher production of inflammatory cytokines compared to wild-type strains [25]. These structures could account for the lower inflammatory potential of Candida spp. compared to S. cerevisiae in a manner not dependent on morphological status [25]. Since these premises, we also take into account the possibility that N-linked mannan β-1,2-mannosides might be a target of laser treatment; indeed, MDDC cultured with laser-treated Candida spp. further decreased their cytokine production compared to untreated Candida strains and to S. cerevisiae. This hypothesis, however, needs to be investigated further. Laser treatment slightly decreased the ability of Candida spp. to activate TLR4 pathways, but the irradiation did not affect TLR4 activation by S. cerevisiae. The TLR2 activation was unaffected by laser radiation, suggesting, once more, that laser effects could not involve deeper layers of the fungal wall, but, rather, the more external ones.
In summary, limited to source, parameters, and mode of irradiation evaluated in this study, laser treatment was able to induce apoptosis in Candida spp. and impair fungal cell survival. Treatment-induced changes in external cell wall structures, as well as changes in membrane permeability and ROS accumulation, could cause apoptosis of fungal cells, thus limiting the release of proinflammatory molecules and increasing the possibility of being phagocytized by macrophages and MDDC.
Furthermore, while laser treatment significantly affected the production of IL-1β and IL-6, it did not modify the production of IL-23 and IL-12, suggesting that TH-17 and TH-1 response needed for the clearance of pathogens [26] could proceed normally, at least in immunocompetent hosts.
Thus, we concluded that NIR laser treatment, performed with the source and parameters proposed here, was able to modify the survival and inflammatory potential of pathogenic Candida spp. It is conceivable that these effects are attributable, at least in part, to structural modifications of N- and O-linked mannans of the fungal cell wall. This hypothesis will be verified in future studies.
On the basis of the presented results, laser treatment could be helpful as an alternative to, or as a co-adjuvant of, antibiotic therapy in immunocompromised hosts with OM complicated with Candida infections. The combined effect of reduced fungal cell survival and inflammation could help to decrease the severity of symptoms and the duration of OM ulcers. Furthermore, since mannose-rich structures, and cell surface mannoproteins in particular, are also involved in mediating biofilm formation in Candida infection, the proposed treatment could also be helpful in Candida infections of different anatomic districts.
However, further studies are needed to better elucidate (i) how laser radiation affects fungal cell survival and what are the chromophores involved and (ii) how laser radiation affects the response/homeostasis of host tissues, i.e., behavior of immune cells, evolution of inflammation, and wound healing in diseased tissue. Indeed, it is known that laser radiation promotes wound healing [27–29]. Moreover, applying the same NIR laser source used in the present study (that is, the same wavelengths and emission mode), we have recently demonstrated the overexpression of NLRP10, a protein involved in the activation of anti-inflammatory pathway, by animal myoblast cells [12, 30, 31], suggesting that such mechanisms can contribute to the overall therapeutic efficacy.
References
Lalla RV, Saunders DP, Peterson DE (2014) Chemotherapy or radiation-induced oral mucositis. Dent Clin North Am 58:341–349
Rautemaa R, Ramage G (2011) Oral candidosis—clinical challenges of a biofilm disease. Crit Rev Microbiol 37:328–336
Pfaller MA, Diekema DJ (2007) Epidemiology of invasive candidiasis: a persistent public health problem. Clin Microbiol Rev 20:133–163
Lalla RV, Patton LL, Dongari-Bagtzoglou A (2013) Oral candidiasis: pathogenesis, clinical presentation, diagnosis and treatment strategies. J Calif Dent Assoc 41:263–268
Gobbo M, Ottaviani G, Perinetti G, Ciriello F, Beorchia A, Giacca M, Di Lenarda R, Rupel K, Tirelli G, Zacchigna S, Biasotto M (2014) Evaluation of nutritional status in head and neck radio-treated patients affected by oral mucositis: efficacy of class IV laser therapy. Support Care Cancer 22:1851–1856
Maver-Biscanin M, Mravak-Stipetic M, Jerolimov V (2005) Effect of low-level laser therapy on Candida albicans growth in patients with denture stomatitis. Photomed Laser Surg 23:328–332
Basso FG, Oliveira CF, Fontana A, Kurachi C, Bagnato VS, Spolidório DM, Hebling J, de Souza Costa CA (2011) In vitro effect of low-level laser therapy on typical oral microbial biofilms. Braz Dent J 22:502–510
Souza RC, Junqueira JC, Rossoni RD, Pereira CA, Munin E, Jorge AO (2010) Comparison of the photodynamic fungicidal efficacy of methylene blue, toluidine blue, malachite green and low-power laser irradiation alone against Candida albicans. Lasers Med Sci 25:385–389
Bornstein E, Hermans W, Gridley S, Manni J (2009) Near-infrared photoinactivation of bacteria and fungi at physiologic temperatures. Photochem Photobiol 85:1364–1374
Chermetz M, Gobbo M, Ronfani L, Ottaviani G, Zanazzo GA, Verzegnassi F, Treister NS, Di Lenarda R, Biasotto M, Zacchigna S (2014) Class IV laser therapy as treatment for chemotherapy-induced oral mucositis in onco-haematological paediatric patients: a prospective study. Int J Paediatr Dent 24:441–449
Collins CD, Cookinham S, Smith J (2011) Management of oropharyngeal candidiasis with localized oral miconazole therapy: efficacy, safety, and patient acceptability. Patient Prefer Adherence 5:369–374
Monici M, Cialdai F, Ranaldi F, Paoli P, Boscaro F, Moneti G, Caselli A (2013) Effect of IR laser on myoblasts: a proteomic study. Mol Biosyst 9:1147–1161
Clemente AM, Fadigati G, Caporale R, Marchese DG, Castronovo G, Sannella AR, Severini C, Verra F, Garaci E, Cozzolino F, Torcia MG (2013) Modulation of the immune and inflammatory responses by Plasmodium falciparum schizont extracts: role of myeloid dendritic cells in effector and regulatory functions of CD4+ lymphocytes. Infect Immun 81:1842–1851
Brachmann CB, Davies A, Cost GJ, Caputo E, Li J, Hieter P, Boeke JD (1998) Designer deletion strains derived from Saccharomyces cerevisiae S288C: a useful set of strains and plasmids for PCR-mediated gene disruption and other applications. Yeast 14:115–132
Rizzetto L, Kuka M, De Filippo C, Cambi A, Netea MG, Beltrame L, Napolitani G, Torcia MG, D’Oro U, Cavalieri D (2010) Differential IL-17 production and mannan recognition contribute to fungal pathogenicity and commensalism. J Immunol 184:4258–4268
Netea MG, Sutmuller R, Hermann C, Van der Graaf CAA, Van der Meer JWM, van Krieken JH, Hartung T, Adema G, Kullberg BJ (2004) Toll-like receptor 2 suppresses immunity against Candida albicans through induction of IL-10 and regulatory T cells. J Immunol 172:3712–3718
Da Silva Dantas A, Day A, Ikeh M, Kos I, Achan B, Quinn J (2015) Oxidative stress responses in the human fungal pathogen, Candida albicans. Biomolecules 5:142–165
Ikner A, Shiozaki K (2005) Yeast signaling pathways in the oxidative stress response. Mutat Res 569:13–27
Brown AJ, Budge S, Kaloriti D, Tillmann A, Jacobsen MD, Yin Z, Ene IV, Bohovych I, Sandai D, Kastora S, Potrykus J, Ballou ER, Childers DS, Shahana S, Leach MD (2014) Stress adaptation in a pathogenic fungus. J Exp Biol 217:144–155
Beaussart A, Alsteens D, El-Kirat-Chatel S, Lipke PN, Kucharíková S, Van Dijck P, Dufrêne YF (2012) Single-molecule imaging and functional analysis of Als adhesins and mannans during Candida albicans morphogenesis. ACS Nano 6:10950–10964
Cheng SC, van de Veerdonk FL, Lenardon M, Stoffels M, Plantinga T, Smeekens S, Rizzetto L, Mukaremera L, Preechasuth K, Cavalieri D, Kanneganti TD, van der Meer JW, Kullberg BJ, Joosten LA, Gow NA, Netea MG (2011) The dectin-1/inflammasome pathway is responsible for the induction of protective T-helper 17 responses that discriminate between yeasts and hyphae of Candida albicans. J Leukoc Biol 90:357–366
Doğan MD, Ataoğlu H, Ataoğlu O, Akarsu ES (1999) Polysaccharide mannan components of Candida albicans and Saccharomyces cerevisiae cell wall produce fever by intracerebroventricular injection in rats. Brain Res Bull 48:509–512
Cheng SC, Joosten LA, Kullberg BJ, Netea MG (2012) Interplay between Candida albicans and the mammalian innate host defense. Infect Immun 80:1304–1313
Mille C, Bobrowicz P, Trinel PA, Li H, Maes E, Guerardel Y, Fradin C, Martínez-Esparza M, Davidson RC, Janbon G, Poulain D, Wildt S (2008) Identification of a new family of genes involved in beta-1,2-mannosylation of glycans in Pichia pastoris and Candida albicans. J Biol Chem 283:9724–9736
Ueno K, Okawara A, Yamagoe S, Naka T, Umeyama T, Utena-Abe Y, Tarumoto N, Niimi M, Ohno H, Doe M, Fujiwara N, Kinjo Y, Miyazaki Y (2013) The mannan of Candida albicans lacking beta-1,2-linked oligomannosides increases the production of inflammatory cytokines by dendritic cells. Med Mycol 51:385–395
Santamaría R, Rizzetto L, Bromley M, Zelante T, Lee W, Cavalieri D, Romani L, Miller B, Gut I, Santos M, Pierre P, Bowyer P, Kapushesky M (2011) Systems biology of infectious diseases: a focus on fungal infections. Immunobiology 216:1212–1227
Carvalho RL, Alcântara PS, Kamamoto F, Cressoni MD, Casarotto RA (2010) Effects of low-level laser therapy on pain and scar formation after inguinal herniation surgery: a randomized controlled single-blind study. Photomed Laser Surg 28:417–422
Güngörmüş M, Akyol U (2009) The effect of gallium–aluminum–arsenide 808-nm low-level laser therapy on healing of skin incisions made using a diode laser. Photomed Laser Surg 27:895–899
Silveira PC, Silva LA, Fraga DB, Freitas TP, Streck EL, Pinho R (2009) Evaluation of mitochondrial respiratory chain activity in muscle healing by low-level laser therapy. J Photochem Photobiol B 95:89–92
Imamura R, Wang Y, Kinoshita T, Suzuki M, Noda T, Sagara J, Taniguchi S, Okamoto H, Suda T (2010) Anti-inflammatory activity of PYNOD and its mechanism in humans and mice. J Immunol 184:5874–5884
Wang Y, Hasegawa M, Imamura R, Kinoshita T, Kondo C, Konaka K, Suda T (2004) PYNOD, a novel Apaf-1/CED4-like protein is an inhibitor of ASC and caspase-1. Int Immunol 16:777–786
Acknowledgments
We thank Prof. G. Mancuso, University of Messina for the generous gift of HEK-293-hTLR4/CD14/MD2 and HEK-293-hTLR2 cells.
This work was supported by grants from the Italian Ministry of Education. Ann Maria Clemente was supported by a grant from Istituto Toscano Tumori.
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
A. M. Clemente and L. Rizzetto contributed equally to this work.
Rights and permissions
About this article
Cite this article
Clemente, A.M., Rizzetto, L., Castronovo, G. et al. Effects of near-infrared laser radiation on the survival and inflammatory potential of Candida spp. involved in the pathogenesis of chemotherapy-induced oral mucositis. Eur J Clin Microbiol Infect Dis 34, 1999–2007 (2015). https://doi.org/10.1007/s10096-015-2443-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-015-2443-5