Abstract
The amino acid metabolism in patients with hepatitis B virus (HBV) infection is significantly changed. In this study, we analyzed the relationship between the amino acid profiles and varying clinical stages of HBV infection, and investigated their significance. The plasma amino acid concentrations in 115 patients with HBV infection and 32 healthy donors were detected and analyzed, and the main indicators of liver function were measured. Correlation analysis was performed between the amino acid profiles (Fischer’s ratio, branched-chain amino acid to tyrosine ratio [BTR]) and the key indicators of liver function in patients with HBV infection. Fisher’s ratio and the BTR of patients with HBV infection was found to differ from that of the healthy controls, and was also found to significantly correlate with the stage of HBV infection. Changes in the BTR were closely related to the level of key indicators of liver function, and a significant relationship was detected between the Fischer’s ratio and the BTR (r = 0.928, p < 0.001). These results suggest that Fischer’s ratio and the BTR can indirectly reflect the degree of liver cell injury. Determining and tracking the plasma amino acid profiles could, therefore, be used for the diagnosis, treatment selection, and prognosis of patients with varying stages of HBV infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The liver is a vital organ that plays a major role in metabolism, including amino acid synthesis. The amino acid contents of peripheral blood plasma are frequently changed in patients with hepatitis B virus (HBV) infection. These changes manifest as an increased concentration of aromatic amino acids (AAAs) and a decreased concentration of branched-chain amino acids (BCAAs). BCAAs have been applied to the diagnosis of viral hepatitis B and as an adjuvant therapy for liver disease [1–3].
Fischer’s ratio, an amino acid-based diagnostic index, represents the ratio between BCAAs and AAAs, defined by the formula (Leu + Val + Ile)/(Tyr + Phe). An abnormal Fischer’s ratio has been reported in liver-related diseases [4, 5]. The BCAA/AAA ratio is often significantly lower in patients with HBV infection. However, how these changes in the BCAA/AAA ratio correlate with the various stages of HBV clinical disease has not been well described. Some reports have suggested that, rather, than measuring the BCAA/AAA ratio, it may be more appropriate and straightforward to measure the BCAA to tyrosine ratio (BTR), which correlates well with the severity of liver disease [6, 7]. In this report, automatic colorimetric determination was used to detect the concentration of amino acids in peripheral blood plasma from patients with various degrees (clinical types) of HBV infection. Furthermore, the relationship between liver function indicators in these patients and their amino acid profiles (Fischer’s ratio, BTR) were also analyzed in order to confirm the relationship between the amino acid profile and clinical symptoms in patients with HBV infection.
Subjects and methods
Subjects
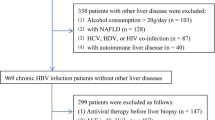
All of the cases included in this study were hospitalized or underwent a follow-up examination in our unit from October 2009 to April 2010. The diagnostic standards for various stages of HBV infection were complied with the diagnostic criteria of the 2000 Xi’an viral hepatitis management scheme [8]. The standards for diagnoses of acute hepatitis B (AHB), chronic hepatitis B (CHB), and chronic severe hepatitis B (CSHB) have been described in detail previously [9–11]. Briefly, AHB patients are defined as those who displayed hepatitis B surface Ag (HBsAg)-negative conversion within 6 months after the initial onset of symptoms due to HBV infection.
Patients with CHB are defined as those who displayed HBsAg-positive, HBeAg-positive, and HBV DNA detectable with abnormal liver function tests. To reflect the degree of liver injury, CHB was subtyped as mild, moderate, and heavy. Their ultrasound diagnostic references are as follows: mild CHB, no significant abnormal evidences in the liver and spleen; moderate CHB, enlargement of the liver echo, slight enlargement of the liver and/or spleen; heavy CHB, significantly enlarged liver echo and uneven distribution, and spleen enlarged. Their laboratory test references are shown in Table 1.
The diagnostic standard for CSHB is as follows: (1) a history of CHB or liver cirrhosis; (2) serum HBsAg positivity >6 months, serum total bilirubin (TBiL) >10 times the normal level; (3) signs of chronic liver disease, such as liver palm and spider angioma, ultrasound abnormal evidence, and so on; (4) liver biopsy histology findings typical of chronic hepatitis. Patients with decompensated liver cirrhosis are defined as follows: advanced liver cirrhosis, Child–Pugh score being B or C level, significant liver dysfunction, and signs of decompensation (such as albumin [Alb] < 35 g/L, A/G < 1.0, significant jaundice, TBiL > 35 μmol/L, alanine transaminase [ALT] and aspartate aminotransferase [AST] increased, prothrombin activity [PTA] < 60%), based on liver biopsy or obvious findings on ultrasound imaging.
The total number of subjects included was 147, excluding those displaying the combined effects of amino acid metabolism and those cases treated with amino acids or Alb. Among these subjects, 86 were men and 61 were women. Their ages ranged from 23 to 65 years, with an average of 48.2 ± 15.5 years. There were 15 cases with AHB, 40 cases with chronic hepatitis B (moderate CHB, 15 cases; heavy CHB, 25 cases), 30 cases with CSHB, 30 cases with liver cirrhosis (LC), including compensated LC (17 cases) or decompensated LC (13 cases), and 32 healthy donors (HDs) who were included as a control group. There were no significant differences in the gender or age among these groups.
The diagnosis of each liver disease case was based on conventional clinical and biochemical data, histological findings, and imaging and endoscopic criteria. None of the recruited patients were co-infected with HIV-1, HIV-2, HAV, HCV, HDV, HEV, or CMV. The 32 healthy donors used as controls were negative for HBsAg and had no clinical or laboratory evidence of other infectious diseases or immunological disorders, and they were from the international health screening center in our unit (First Affiliated Hospital, College of Medicine, Zhejiang University). This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the medical ethics committee in the First Affiliated Hospital, College of Medicine, Zhejiang University. Verbal informed consent was obtained from all subjects. Verbal consent was witnessed and formally recorded.
Reagents and instruments
Plasma amino acid concentrations were measured by an auto amino acid analyzer (L-8800; Hitachi, Tokyo, Japan) with colorimetric analysis. Enzyme-linked immunosorbent assay (ELISA) kits were used to detect HBV serological markers (HBVMs) according to the manufacturer’s instructions (Kehua Industrial Biotechnology Co. Ltd., Shanghai, China), and the PT (prothrombin time) was determined using an automated coagulation analyzer (Sysmex CA-500 Series, USA). Biochemical indicators of liver function were measured on an automatic biochemical analyzer (Abbott, Chicago, IL, USA).
Specimen collection
Peripheral venous blood samples were obtained as soon as the liver disease was diagnosed, before the anti-viral treatment, from 115 patients with HBV infection after an overnight fast, and the sera were tested for biochemical indicators of liver function and HBV serum markers. Three milliliters of venous blood was placed into a vacuum tube, along with EDTA·Na2 anticoagulant (BD, New Jersey, USA), and centrifuged at 1,100 × g for 10 min, to separate the blood plasma. All samples were stored at −75°C prior to measurement.
Determination of the amino acid spectra and HBV DNA loading
The above cryopreserved plasma (0.5 ml) was added to 4% sulfosalicylic acid (1.5 ml) and mixed well. This mixture was centrifuged at 26,900 × g for 15 min, then 1 ml of the supernatant was placed in a vial (UNK) and applied to an amino acid analyzer (L-8800, HITACHI, Japan), which automatically takes 0.02 ml for amino acid analysis with spectrophotometrical detection after postcolumn reaction with ninhydrin reagent, and the flushing fluid was 0.2 mmol/L citric acid buffer (pH 3.3). Standard products and test kits were provided by Hitachi (Japan). The ammonia is measured using an automatic biochemical analyzer (CX9, Beckman, USA) with enzymatic ammonia determination, according to the manufacturer’s directions.
The serum HBV DNA loading in patients was quantitated using a commercial polymerase chain reaction (PCR) diagnostic kit (PG Biotech, Shenzhen, China), with a minimal detection standard of 500 copies/ml, and the HBV genotypes were determined as reported in a previous paper [12].
Statistical analysis
All dosimetric values are presented and were analyzed using SPSS version 16.0 software (SPSS Inc., Chicago, IL, USA), and p-values less than 0.05 were considered to be statistically significant. The correlation between the amino acid profiles (Fischer’s ratio, BTR) and liver function indicators were analyzed using Spearman’s correlation coefficient (r-values) and linear regression analysis.
Results
Characteristics of patients and healthy donors
The main clinical and laboratory key indicators for the patients are shown in Table 2. Patients with HBV infection showed lower Alb levels and higher PT values (p < 0.01 or 0.05) compared with patients with AHB or HDs.
Plasma amino acid profiles
The concentrations of the 18 plasma amino acids in the 115 patients with various stages of HBV infection and the 32 HDs were detected automatically, and are shown in Table 3. The results show that, compared with HDs, in most patients with AHB, the three plasma amino acids Thr, Glu, and Met were significantly increased (p < 0.01 or 0.05), and the amino acid Pro was significantly decreased (p < 0.01); in patients with CHB, the amino acids Thr, Glu, Met, Tyr, and Phe were significantly increased (p < 0.01 or 0.05), and the amino acids Val, Ile, and Leu were significantly decreased (p < 0.01 or 0.05). Furthermore, in heavy CHB patients, the amino acids Lys and Arg were significantly increased (p < 0.01 or 0.05), and the amino acids Ala and Gly were significantly decreased (p < 0.05). In patients with LC or CSHB, the amino acids Thr, Glu, Cys, Met, Tyr, and Phe were significantly increased (p < 0.01 or 0.05), and the amino acids Ala, Gly, Val, Ile, and Leu were significantly decreased (p < 0.01 or 0.05). Furthermore, the amino acids Lys and Arg were significantly increased (p < 0.01) in CSHB patients.
The BCAA/AAA ratio and the BTR were then calculated, and are shown in Fig. 1a, along with the Tyr (tyrosine) concentration (Fig. 1b). When compared with the control group (HDs), the concentration of AAA and Tyr from patients with HBV infection showed significant differences (p < 0.05 or 0.01), with the exception of the CHB-m group (p > 0.05). Furthermore, a significant decrease (p < 0.05 or 0.01) was recorded when the BCAA concentration, the BCAA/AAA ratio, and the BTR from patients with various clinical stages of HBV infection (AHB, CHB-m, CHB-h, LC, and CSHB) were compared with those of the HD group. Moreover, the BCAA/AAA ratio and the BTR were most significantly decreased in the CSHB group (p < 0.001).
Amino acid profile from various statuses of patients with hepatitis B infection. In each cluster, columns from the left to the right are, respectively, healthy donors (HD), acute hepatitis B (AHB), moderate chronic hepatitis B (CHB-m), heavy chronic hepatitis B (CHB-h), liver cirrhosis (LC) (compensated or decompensated), and chronic severe hepatitis B (CSHB). Tyr tyrosine, BCAA branched-chain amino acid, AAA aromatic amino acid, BTR branched-chain amino acid and tyrosine ratio. #p > 0.05; *p < 0.05; **p < 0.01; ***p < 0.001 vs. the HD group
Amino acid profile associated with liver function
Correlation analysis between the amino acid profiles and the key indicators of liver function in the patients with various stages of HBV infection indicated a statistically significant positive correlation between Tyr and PT, but no significant difference between Tyr, TBiL, and Alb. Furthermore, the BCAA/AAA ratio and the BTR showed a significant positive correlation with Alb, and a significant inverse correlation with TBiL and PT, as shown in Table 4.
Fischer’s ratio correlation with the BTR
The Fischer’s ratio for patients with different clinical stages of HBV infection was determined by correlation analysis with their BTR. A significant positive correlation was detected (r = 0.928, p < 0.001), as shown in Fig. 2.
Discussion
The liver plays a central role in amino acid metabolism, and AAAs are mainly metabolized in the liver by the enzymes phenylalanine hydroxylase and tyrosine aminotransferase in hepatocytes. BCAAs, however, are mainly metabolized in skeletal muscle, where they react with alpha-ketoglutaric acid and are converted to glutamine by transamination [13]. The plasma amino acid concentration is determined by the rate at which amino acids appear in plasma and other pools, as well as the rate at which they disappear via conversion to other amino acids, breakdown, excretion, and incorporation into proteins. Thus, HBV patients with liver dysfunction frequently present with increased plasma AAA levels; a large number of endogenous proteins decompose in plasma, which further increases the plasma AAA levels [5].
In 1979, James et al. proposed a unified hypothesis on the pathogenesis of hepatic encephalopathy (HE) [14], based on the observation that, during hepatic failure, the plasma levels of BCAAs decreased and those of AAAs increased. Numerous literature reports have confirmed an imbalance between AAA and BCAA in both experimental and clinical liver failure, and this leads to a decrease in Fischer’s ratio [3, 12, 15]. However, there are few reports on detailed plasma amino acid profiles in peripheral blood from patients with various clinical types of chronic hepatitis B. Our results show that the profile of 18 amino acids differed among patients with various clinical types of hepatitis B compared to healthy donors. These findings may help in diagnosing and prescribing adjuvant therapy for patients with HBV [2, 16, 17].
There was no significant difference in the PT between AHB patients and HDs, although the plasma amino acid profile of the HD group was altered, and AHB patients showed increased BCAA and Try levels and lower BTR and BCAA/AAA ratios compared to the HD group. This may be because acute liver damage leads to increases in BCAA levels and, to a larger extent, AAA levels in plasma. This may be attributed to the following events [18]: (1) when hepatocytes are damaged, they may not be able to metabolize amino acids absorbed from the intestine; (2) the capacity of the body to absorb sugar, protein, and fat is decreased, which leads to decomposition of the body’s own tissues to produce large amounts of amino acids for energy metabolism; and (3) when heavier inflammation of the liver occurs, leading to liver cell death, more amino acids may be released into the blood.
Tyr concentrations in plasma from patients with moderate chronic hepatitis B (CHB-m), heavy chronic hepatitis B (CHB-h), or LC were higher than those in the HD group, and the differences were significant. Furthermore, the Tyr concentrations in plasma from patients with CSHB significantly increased. Although there is a general opinion that a decrease in Fischer’s ratio is a typical finding only in patients with liver cirrhosis, the BCAA/AAA ratio and BTR in patients with various stages of HBV infection were significantly decreased. These two ratios were lowest for the CSHB group among all of the groups, while the Tyr and PT levels were significantly higher compared with the HD group, which, to the best of our knowledge, has not been reported previously. The discrepancy between previous opinions and our findings may be attributed to differences in technique, reagents, blood samples, and the potential number of HE cases in the LC and CSHB groups. The number of cases needs to be expanded in order to validate our conclusion.
During HBV infection, histological changes occur in liver cells that lead to the development of severe necrosis, necrotic debris, bridging necrosis, and interstitial fibrosis. As liver function decreases, plasma amino acid levels tend to increase, especially AAAs. Plasma Thr levels were elevated in patients with various clinical stages of HBV, which may be related to a change in the activity of threonine-degrading enzymes. Moreover, when liver cells are damaged, their regeneration capacity and, thus, the amount of amino acids needed for protein synthesis decreases, which could explain the increase in Thr levels in peripheral blood. A higher concentration of amino acids induces the excitation of pancreatic alpha cells, leading to an increase in blood glucagon and prompting muscle and adipose tissues to increase their uptake of BCAAs. When the liver is seriously damaged, inactivation of insulin in the liver is decreased, resulting in a significant increase in glucagon levels, which further promote BCAA metabolism in muscle. This results in a decrease in BCAA levels and a gradual decrease in the BCAA/AAA ratio [19].
The decreased BCAA/AAA ratio observed in patients with HBV infection positively correlates with the degree of liver function damage [20]. Therefore, the BCAA/AAA ratio may be used to judge disease severity and prognosis for patients with HBV infection [2, 3]. In agreement with this, the BTR in the present study was significantly decreased in LC and CH patients compared with healthy subjects. The findings suggest that BTR may be a useful marker of the severity of liver dysfunction in patients with chronic liver disease.
When chronic liver disease progresses to the LC stage, the reduced ability of liver cells to dispose of ammonia is compensated by increased metabolism in skeletal muscles. Increased metabolism of BCAA in skeletal muscles causes a reduction in the plasma levels of these amino acids and in the BCAA/AAA ratio in patients with liver cirrhosis [21]. The capability of sclerotic liver to degrade AAAs decreases, and this is accompanied by increased catabolism of amino acids in patients with HBV infection, resulting in a significant decrease in the BCAA/AAA ratio and BTR. The change in amino acid content in patients with liver cirrhosis is related to liver metabolism changes, liver cell necrosis, and the presence of hormone metabolic abnormalities [22, 23].
The results for amino acid profiles and key indicators of liver function reveal that Tyr and Alb showed a significant inverse correlation, and that Tyr was significantly positively correlated with TBiL and PT. Tyrosine is the predominant AAA, and Tyr concentrations correlate with liver disease development [24, 25]. The relationship between the BCAA/AAA ratio, BTR, and Alb showed a significant positive correlation, whereas a significant inverse correlation was observed for TBiL and PT. In the liver, Alb, PT, and TBiL levels reflect the generation of liver cells and inflammation and necrosis. The higher the level of TBiL and PT, the lower the level of Alb, which usually implies more severe liver cell damage [25]. Therefore, BTR also indirectly reflects the degree of liver cell damage, and may be an alternative index to the BCAA/AAA ratio.
BTR can be used to determine the degree of liver fibrosis in patients with HCV infection [6] and to evaluate liver disease prognosis [26]. Furthermore, among patients with HBV, changes in the BCAA/AAA ratio correlate well with liver pathology, which may indirectly reflect the degree of liver cell damage or clinical liver disease severity, and could, thus, be used as an independent prognostic factor [17, 27]. Therefore, for patients with HBV infection, the measurement and monitoring of plasma amino acid profiles, in particular, for BCAAs (Leu, Val, and Ile) and Try (BTR), could be used not only for the typing and staging of HBV diagnosis and evaluating the nutritional status of HBV patients, but also to gain a better understanding of pathological changes in the liver, especially in the scope of liver cell necrosis. Plasma amino acid profiles and Tyr concentrations may be associated with fatigue in patients with primary biliary cirrhosis and primary sclerosing cholangitis [24]. For patients with hepatitis, BCAA supplementation appears to be associated with a lower frequency of cirrhosis complications and better nutritional status, and can significantly improve the quality of life and the prognosis of hepatic disease [16, 28].
In conclusion, plasma amino acid profiles or BTR for patients with HBV infection vary depending on the degree of liver damage. Liver cell inflammation, necrosis, and liver function are all closely related to BTR changes, and this ratio can, therefore, indirectly reflect the degree of liver cell damage. The BTR is also simple to determine by an enzymatic method [29]. Therefore, the measurement and monitoring of plasma amino acid profiles or BTR is proposed as a promising alternative method to aid in the clinical diagnosis, selection of appropriate nutritional adjuvant therapy, and prognosis assessment for patients with HBV infection. This method is also a suitable non-invasive approach for the diagnosis of CHB [30].
References
Holecek M (2010) Three targets of branched-chain amino acid supplementation in the treatment of liver disease. Nutrition 26(5):482–490
Tom A, Nair KS (2006) Assessment of branched-chain amino acid status and potential for biomarkers. J Nutr 136(1 Suppl):324S–330S
Roth E, Druml W (2011) Plasma amino acid imbalance: dangerous in chronic diseases? Curr Opin Clin Nutr Metab Care 14(1):67–74
James JH (2002) Branched chain amino acids in heptatic encephalopathy. Am J Surg 183(4):424–429
Dejong CH, van de Poll MC, Soeters PB, Jalan R, Olde Damink SW (2007) Aromatic amino acid metabolism during liver failure. J Nutr 137(6 Suppl 1):1579S–1585S; discussion 1597S–1598S
Ninomiya T, Yoon S, Sugano M, Kumon Y, Seo Y, Shimizu K, Nagano H, Kasuga M, Hayashi Y (1999) Improvement of molar ratio of branched-chain amino acids to tyrosine (BTR) associated with liver fibrosis in chronic hepatitis C patients treated with interferon-alpha. Dig Dis Sci 44(5):1027–1033
Kawamura-Yasui N, Kaito M, Nakagawa N, Fujita N, Ikoma J, Gabazza EC, Watanabe S, Adachi Y (1999) Evaluating response to nutritional therapy using the branched-chain amino acid/tyrosine ratio in patients with chronic liver disease. J Clin Lab Anal 13(1):31–34
Chinese Society of Infectious Diseases and Parasitic Diseases CSoH, Chinese Medical Association (2000) Management scheme of diagnostic and therapy criteria of viral hepatitis [in Chinese]. Zhonghua Gan Zang Bing Za Zhi (Chin J Hepatol) 8(6):324–329
Xu D, Fu J, Jin L, Zhang H, Zhou C, Zou Z, Zhao JM, Zhang B, Shi M, Ding X, Tang Z, Fu YX, Wang FS (2006) Circulating and liver resident CD4+CD25+ regulatory T cells actively influence the antiviral immune response and disease progression in patients with hepatitis B. J Immunol 177(1):739–747
Xu XW, Lu MH, Tan DM (2005) Association between tumour necrosis factor gene polymorphisms and the clinical types of patients with chronic hepatitis B virus infection. Clin Microbiol Infect 11(1):52–56
Ke WM, Ye YN, Huang S (2003) Discriminant function for prognostic indexes and probability of death in chronic severe hepatitis B. J Gastroenterol 38(9):861–864
Chen Y, Li X, Ye B, Yang X, Wu W, Chen B, Pan X, Cao H, Li L (2011) Effect of telbivudine therapy on the cellular immune response in chronic hepatitis B. Antiviral Res 91(1):23–32
Cynober LA (2002) Plasma amino acid levels with a note on membrane transport: characteristics, regulation, and metabolic significance. Nutrition 18(9):761–766
James JH, Ziparo V, Jeppsson B, Fischer JE (1979) Hyperammonaemia, plasma aminoacid imbalance, and blood–brain aminoacid transport: a unified theory of portal-systemic encephalopathy. Lancet 2(8146):772–775
Benjamin IS, Engelbrecht GH, Saunders SJ, van Hoorn-Hickman R (1988) Amino acid imbalance following portal diversion in the rat. The relevance of nutrition and of hepatic function. J Hepatol 7(2):208–214
Charlton M (2006) Branched-chain amino acid enriched supplements as therapy for liver disease. J Nutr 136(1 Suppl):295S–298S
Noguchi Y, Zhang QW, Sugimoto T, Furuhata Y, Sakai R, Mori M, Takahashi M, Kimura T (2006) Network analysis of plasma and tissue amino acids and the generation of an amino index for potential diagnostic use. Am J Clin Nutr 83(2):513S–519S
Holm E, Sedlaczek O, Grips E (1999) Amino acid metabolism in liver disease. Curr Opin Clin Nutr Metab Care 2(1):47–53
Schön MR, Heil W, Lemmens HP, Padval D, Matthes M, Puhl G, Neuhaus P, Hammer C (1999) Xenogeneic, extracorporeal liver perfusion in primates improves the ratio of branched-chain amino acids to aromatic amino acids (Fischer’s ratio). Eur Surg Res 31(3):230–239
Nijveldt RJ, Wiezer MJ, Meijer C, Prins HA, Statius Muller MG, Gouma DJ, Teerlink T, van Gulik TM, Borel Rinkes IH, Tilanus HW, van de Velde CJ, Wiggers T, Zoetmulder FA, Scotté M, Cuesta MA, Meijer S, van Leeuwen PA (2001) Major liver resection results in a changed plasma amino acid pattern as reflected by a decreased Fischer ratio which improves by bactericidal/permeability increasing protein. Liver 21(1):56–63
Doi J, Shiraishi K, Haida M, Matsuzaki S (2004) Abnormality of energy metabolism in the skeletal muscle of patients with liver cirrhosis and changes under administration of glucose and branched-chain amino acids. Tokai J Exp Clin Med 29(4):191–198
Moriwaki H, Miwa Y, Tajika M, Kato M, Fukushima H, Shiraki M (2004) Branched-chain amino acids as a protein- and energy-source in liver cirrhosis. Biochem Biophys Res Commun 313(2):405–409
Tessari P, Kiwanuka E, Vettore M, Barazzoni R, Zanetti M, Cecchet D, Orlando R (2008) Phenylalanine and tyrosine kinetics in compensated liver cirrhosis: effects of meal ingestion. Am J Physiol Gastrointest Liver Physiol 295(3):G598–G604
ter Borg PC, Fekkes D, Vrolijk JM, van Buuren HR (2005) The relation between plasma tyrosine concentration and fatigue in primary biliary cirrhosis and primary sclerosing cholangitis. BMC Gastroenterol 5:11
Suzuki K, Suzuki K, Koizumi K, Ichimura H, Oka S, Takada H, Kuwayama H (2008) Measurement of serum branched-chain amino acids to tyrosine ratio level is useful in a prediction of a change of serum albumin level in chronic liver disease. Hepatol Res 38(3):267–272
Zhang Q, Takahashi M, Noguchi Y, Sugimoto T, Kimura T, Okumura A, Ishikawa T, Kakumu S (2006) Plasma amino acid profiles applied for diagnosis of advanced liver fibrosis in patients with chronic hepatitis C infection. Hepatol Res 34(3):170–177
Kano T, Nagaki M, Takahashi T, Ohnishi H, Saitoh K, Kimura K, Muto Y (1991) Plasma free amino acid pattern in chronic hepatitis as a sensitive and prognostic index. Gastroenterol Jpn 26(3):344–349
Plauth M (2006) Branched chain amino acids as oral supplements in liver cirrhosis. Z Gastroenterol 44(2):207–208
Nakamura T, Mori M, Yoshida T, Murakami N, Kato T, Sugihara J, Saito K, Moriwaki H, Tomita E, Muto Y et al (1989) Enzymatic determination of a molar ratio of free branched-chain amino acids to tyrosine (BTR) and its clinical significance in plasma of patients with various liver diseases. Rinsho Byori 37(8):911–917
Ayonrinde OT, Olynyk JK (2010) PAHA model: an alternative non-invasive predictor of liver cirrhosis in patients with chronic hepatitis B infection. J Gastroenterol Hepatol 25(1):3–4
Acknowledgments
This work was supported by the Team of Key Science and Technology Innovation of Zhejiang Province (2009R50041), People’s Republic of China, the National High-technology R&D Program of China (2009CB522406), the Zhejiang Medical Health Foundation of China (2009B069), and the Major National S&T Projects for infectious diseases (11th Five Year) (2008ZX10002-007, 2009ZX10004-309).
Competing interests
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 34.0 kb)
Rights and permissions
About this article
Cite this article
Yang, J., He, J., Cao, H. et al. Correlation between plasma amino acid profiles and the various stages of hepatitis B infection. Eur J Clin Microbiol Infect Dis 31, 2045–2052 (2012). https://doi.org/10.1007/s10096-011-1538-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-011-1538-x