Abstract
Resins (rosin, pitch) are natural products of the coniferous trees and are antimicrobial against a wide range of microbes. The antifungal effectiveness of resin, purified from Norway spruce (Picea abies), was studied against human pathogenic fungi and yeasts with the agar plate diffusion tests and electron microscopy (EM). The fungistatic effect of these resin mixtures (resin salves) was tested against a set of Candida yeasts, dermatophytes, and opportunistic fungi. Transmission and scanning EM was done from samples of fungi (Trichophyton mentagrophytes). In agar diffusion tests, the resin was strongly antifungal against all dermatophytes tested, e.g., against all fungi of the genus Trichophyton, but it was not antifungal against the Candida yeasts or against the opportunistic fungi tested. According to EM, resin caused damages in the cell hyphae and cell wall structures. We conclude that, in the agar plate diffusion test, coniferous resins are strongly fungistatic against the dermatophytic fungi only.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Resins (rosin, pitch) are natural products of the coniferous trees and are used, for example, as raw materials for many technical and cosmetic products worldwide. Home-made resin salve from Norway spruce (Picea abies) has been, for centuries, a part of the folk medicine in various skin infections in Northern Finland and Sweden [1, 2]. In ecology, the resins are considered to play a role in the defense of the coniferous trees against insects and microbial pathogens [3]. Recent observations have suggested that the coniferous resins, and the resin-derived salves, are both in vitro and in vivo antimicrobial against a surprisingly wide range of microbes that are hazardous for human health, and are, therefore, potential tools in the treatment of skin infections and chronic wounds in human medicine [4–6]. Antifungal effects of the resin against clinically important fungi are, however, poorly known.
We performed this in vitro study in order to examine the effectiveness of the spruce resin against different fungi and yeasts with special emphasis on fungi of the genus Trichophyton, which are the main cause of fungal nail and skin infections in humans in the Western countries [7]. We examined the antifungal actions of the traditionally manufactured resin salve and of those where the resin is mixed with biologically inert modern salve. In addition, we carried out an electron microscopy (EM) examination to see by which way the resin may affect the fungi on the agar diffusion plates.
Materials and methods
Purification of the spruce resin
The resin was collected in Kolari, Finnish Lapland, from the trunks of full-grown Norway spruce (Picea abies) with knives by permission from the landowners. The resin was mechanically purified from bark and other impurities, and stored at room temperature until they were used. The resin was finally purified by dissolving the mechanically refined resin with alcohol (ethanol) for several weeks at room temperature, after which the ethanol mixture was filtered (patent pending FI123787). The resin concentration in the final filtrates varied between 50 and 60% (w/w), from which filtrate solid purified resin could be obtained by evaporation of the ethanol by gentle warming.
Acetone extracts of the solid purified resin displayed three major groups of compounds in the gas–liquid chromatography (GLC): (1) p-coumaric acid; (2) group of various resin acids (e.g., abietic acid, pimaric acid, neoabietic acid, palustric acid, levopimaric acid, and their hydroxy derivatives, etc.), and (3) a group of lignans (e.g., matairesinol, isolariciresinol, pinoresinol, lariciresinol, isolariciresinol, etc.). On rough average, 10%, 60%, and 30% of purified trunk resin from Norway spruce are p-coumaric acid, resins acids, or lignans, respectively.
Preparation of the resin salve mixtures
The purified resin was mixed in different concentrations (10%, 20%, 30% and 40% [w/w]) with a formulated modern salve base (composed of sorbitan oleate [17%], hydroxyethyl cellulose [2%], and water [81%]), or by mixing the resin with ordinary butter (animal fat) at a concentration of 50% (w/w), as has been the case in salves used in traditional medicine [2].
Agar plate diffusion tests
The experiments were performed with ordinary procedures [8, 9]. The resin salves were applied as samples of 0.1 ml in 9-mm-diameter holes in the agar gel (agar wells). The RPMI medium (Sigma-Aldrich®, St. Louis, MO, USA) was used as the culture medium. Samples of sterile saline without resin were used as controls. The indifferent salve base (containing sorbitan oleate, hydroxyethyl cellulose, and water) used in the manufacturing of the modern resin salve was not antimicrobial in the microbiological tests performed earlier [10, 11]. Salt-free butter used as a salve base in the traditional resin salve was not antimicrobial either [12].
The agar diffusion plates were incubated at 35°C in ambient air for 24–48 h (yeasts) or 7 days (dermatophytes and yeasts) before the final inspection. The size of the inhibition zone was used as the criterion of the antifungal activity.
Yeasts and fungi tested
The yeasts and fungi tested in this study are listed and shown in Table 1.
TEM and SEM
For transmission electron microscopy (TEM) and scanning electron microscopy (SEM), the samples were taken from Trichophyton mentagrophytes agar diffusion plates from sites where: (1) no inhibition was observed in the growth of the fungi and (2) from the transitional zone between areas of inhibition and normal growth (margin of the inhibitory zone).
The samples for thin sections in TEM and SEM were prepared as described by Lounatmaa [13].
The samples for TEM were removed from the cultures and prefixed in phosphate-buffered (pH 7.2) 2.5% glutaraldehyde for 2 h at room temperature. The fixed cells were collected by centrifugation and washed three times with phosphate buffer. All samples were postfixed with phosphate-buffered 1% osmium tetroxide, dehydrated, and embedded in Epon. After polymerization of the Epon, thin sections were prepared with a ultramicrotome and the sections were collected on grids and poststained with uranyl acetate and lead citrate. The TEM micrographs were taken with a JEM-1200EX (Jeol, Tokyo, Japan) device at 60 kV.
The samples for SEM were prefixed on plates in phosphate-buffered (pH 7.2) 2.5% glutaraldehyde for 2 h at room temperature. The fixed cells were washed three times with phosphate buffer. All samples were postfixed with phosphate-buffered 1% osmium tetroxide, dehydrated, and, finally, dried using the critical point method.
SEM micrographs were taken with a JSM-6335F field emission scanning electron microscope (Jeol, Tokyo, Japan) at 5 to 15 kV.
Results
Agar plate diffusion tests
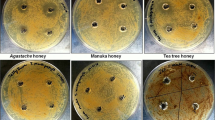
The test results from the agar plate diffusion tests are presented in Table 1. An antifungal effect with both traditional and formulated resin salve was found against all the dermatophytes tested, including all the Trichophyton fungi tested. However, the resin showed practically no antimycotic effect against Candida yeasts. Exceptions were plates of C. glabrata and C. krusei, where a narrow inhibition zone occurred. No antifungal influence of the resin against the two opportunistic fungi tested was observed (Table 1).
Inhibition of the fungi of the genus Trichophyton (T. rubrum, T. mentagrophytes, and T. tonsurans) with resin was dependent on the concentration of the resin in the salve mixture (Fig. 1). Salve with resin at a concentration of 10% showed a slight antifungal action, whereas the salve with a resin concentration of 20% or more caused a significant fungicidal effect that roughly corresponded to that with the 50% resin salve (Fig. 1).
TEM and SEM
The samples from the margin of the inhibition zone in agar plates demonstrated in TEM and SEM destructive injuries in fungal cells (T. mentagrophytes). The injured and normal fungi are illustrated in Figs. 2, 3, 4, and 5. Inside the inhibition zone, the fungal cells were dead or appeared as remnants of short cell hyphae. Outside the inhibition zone, the fungal hyphae were intact, with plentiful spores. The cells at the margin area did show injuries in the cell wall structures. The affected hyphae were folded and irregular, and the cell walls were granular and flaky. Some hyphae were short and looked “amputated” and the resin seemed to destroy the fungal hyphae segment by segment. In short, the changes observed in TEM and SEM were considered to indicate unspecific destructive and toxic actions of resin in the cell walls of the fungal hyphae.
Discussion
This in vitro study shows that the resin purified from Norway spruce (Picea abies) trunk is clearly antifungal, against dermatophytes and against the fungi of Trichophyton species in particular. This antifungal action was independent of whether the resin was mixed as salve with the traditional (fat/butter) way or the “modern” (formulated salve base) way, suggesting that the observed antifungal influences are, indeed, due to the resin and not to other ingredients in the salve or animal fat.
Interestingly, the spruce resin was not antifungal against Chrysosporium keratinophilum, which is a species closely related with dermatophytes and may be a human opportunistic pathogen in toe nails [14]. In addition, the Fusarium species tested [15], which are more distantly related to Trichophyton fungi, were also totally resistant to resin in the present diffusion test. Furthermore, even though the resin inhibited the growth of all dermatophytes studied, it did not definitely affect the most common Candida yeasts.
The present observation that the resin was microbicidal against all dermatophytes tested but not against the yeasts and opportunistic fungi may indicate that the mechanisms by which the resin inhibits the growth of the microbes are “specific”. Correspondingly, in the earlier studies with bacteria, the resin was microbicidal against Gram-positive bacteria but not against Gram-negative bacteria [12]. However, in the European Pharmacopoeia (EP) challenge test, the resin was microbicidal also against the Gram-negative bacteria, such as Escherichia coli or Pseudomonas aeruginosa [11]. Interestingly also, the Candida yeasts were insensitive to the coniferous resin in the present agar test, but these yeasts were sensitive to resin in the EP challenge test [11]. The authors cannot explain why these controversies occur between the tests (agar plate diffusion test vs. challenge test) and microbes. One explanation may be methodological. Coniferous resins are poorly water-soluble [10] and may not, therefore, diffuse in agar plates in concentrations that are sufficient to induce proper microbicidal actions against less sensitive microbes (e.g., C. albicans). Based on this assumption, the dermatophytes are more sensitive to resin than Candida species and induce, therefore, a clear inhibition zone in the agar plate.
In the challenge tests, the micro-organisms are inoculated into the challenge medium (resin salve) directly, where diffusion and water solubility may not be critical issues, and the microbicidal effectiveness of the resin may become more easily demonstrable also against the less sensitive microbes. This explanation is supported by the present study with agar diffusion tests, according to which the fungistatic effect of resin against the T. mentagrophytes fungi was dependent on the resin concentration in the salve applied. A clear fungistatic inhibition zone against the dermatophytes was visible if the resin concentration in the salve was 20% (w/w) or more, but this zone was minimal if the concentration was 10%.
In the SEM of T. mentagrophytes fungi, morphological damages in fungal hyphae were observed in cells in the samples prepared from the area of the inhibition zone on the agar plate. Inside the inhibition zone, all cells were dead, whereas the fungal cells outside the inhibition zone looked morphologically normal. In cells at the inhibition zone (in both TEM and SEM), the most remarkable damages were observed in the cell walls of hyphae, indicating that the destructive actions of resin in fungi are similar to those in bacterial cells, and are targeted to the cell wall and membrane structures [10]. The studies with bacteria suggest that this action is an unspecific damage, obviously mediated by terpenic resin acids [10].
In the present study, the Candida yeasts were observed to be quite resistant to resin, although the Candida yeasts are usually more susceptible micro-organisms to antimicrobial agents than the dermatophytes. The reason for this observation is unknown. One explanation may be the structural and biological differences between the Candida yeasts and dermatophytic fungi. The Candida yeasts are unicellular eukaryotic micro-organisms which grow by pseudohyphae-like buddings, whereas the dermatophytic fungi are real hyphae-forming tubular and multicellular fungi.
An important observation in the present study was that all the dermatophytes tested were sensitive to the coniferous resin. This suggests that the resin salves (resin concentration of 20% [w/w] or more) could be a tool for the treatment of dermatophytic Trichophyton infections. These infections are common skin and nail infections worldwide and affect millions of people, which makes the search and innovation of new effective antifungal therapies reasonable [16].
Resin salve has been used in Northern Europe for centuries in traditional medicine for the treatment of wounds, scratches, and nail infections, without major side effects. On average, 1–3% of people were reported to be allergic to rosin (colophony) and may develop allergic contact dermatitis when coming into contact with natural resins [17, 18]. However, none of the 38 patients with onychomycosis treated in an observational trial with 30% resin lacquer for several months had allergic reactions (article in preparation). In fungal nail infections, the use of effective topical preparations with per oral medications are an accepted treatment option, and this is likely the case with the resin containing salves or lacquers as well [19, 20].
References
Olai B (1578) Een Nyttigh Läkere Book. Stockholm
Sipponen A, Lohi J (2003) Lappilainen Pihkahoito—“uusi” painehaavaumien hoitokeino? Kansanparannusta parhaimmillaan. Suom Lääkäril 58:3775–3776
Trapp S, Croteau R (2001) Defensive resin biosynthesis in conifers. Annu Rev Plant Physiol Plant Mol Biol 52:689–724
Mahady GB (2005) Medicinal plants for the prevention and treatment of bacterial infections. Curr Pharm Des 11:2405–2427
Sipponen A, Jokinen JJ, Sipponen P, Papp A, Sarna S, Lohi J (2008) Beneficial effect of resin salve in treatment of severe pressure ulcers: a prospective, randomized and controlled multicentre trial. Br J Dermatol 158:1055–1062
Sipponen A, Jokinen JJ, Lohi J (2007) Resin salve from the Norwegian spruce tree: a “novel” method for the treatment of chronic wounds. J Wound Care 16:72–74
Mügge C, Haustein UF, Nenoff P (2006) Causative agents of onychomycosis—a retrospective study. J Dtsch Dermatol Ges 4:218–228
Murray PR, Baron EJ, Jorgensen JH, Landry ML, Pfaller MA (2007) (eds) Manual of clinical microbiology, 9th edn. ASM (American Society for Microbiology) Press, Washington, D.C.
Clinical and Laboratory Standards Institute (CLSI) (2008) Reference Method for Broth Dilution Antifungal Susceptibility Testing of Filamentous Fungi; Approved Standard—Second Edition. Document M38-A2. CLSI, Wayne, PA, USA
Sipponen A, Peltola R, Jokinen JJ, Laitinen K, Lohi J, Rautio M, Männistö M, Sipponen P, Lounatmaa K (2009) Effects of Norway spruce (Picea abies) resin on cell wall and cell membrane of Staphylococcus aureus. Ultrastruct Pathol 33:128–135
Sipponen A, Laitinen K (2011) Antimicrobial properties of natural coniferous rosin in the European Pharmacopoeia challenge test. APMIS 119:720–724
Rautio M, Sipponen A, Peltola R, Lohi J, Jokinen JJ, Papp A, Carlson P, Sipponen P (2007) Antibacterial effects of home-made resin salve from Norway spruce (Picea abies). APMIS 115:335–340
Lounatmaa K (1985) Electron microscopic methods for the study of bacterial surface structures. In: Korhonen T, Dawes EA, Mäkelä PH (eds) Enterobacterial surface antigens: methods for molecular characterization. Elsevier, Amsterdam, pp 243–261
Abdel-Hafez AI, el-Sharouny HM (1990) Keratinophilic and saprophytic fungi isolated from students’ nails in Egypt. J Basic Microbiol 30:3–11
Gupta AK, Baran R, Summerbell RC (2000) Fusarium infections of the skin. Curr Opin Infect Dis 13:121–128
Gupta AK, Jain HC, Lynde CW, Macdonald P, Cooper EA, Summerbell RC (2000) Prevalence and epidemiology of onychomycosis in patients visiting physicians’ offices: a multicenter Canadian survey of 15,000 patients. J Am Aced Dermatol 43:244–248
Estlander T, Jolanki R, Alanko K, Kanerva L (2001) Occupational allergic contact dermatitis caused by wood dusts. Contact Dermatitis 44:213–217
Färm G (1998) Contact allergy to colophony. Clinical and experimental studies with emphasis on clinical relevance. Acta Derm Venereol Suppl (Stockh) 201:1–42
Rodgers P, Bassler M (2001) Treating onychomycosis. Am Fam Physician 63:663–672, 677–678
Finch JJ, Warshaw EM (2007) Toenail onychomycosis: current and future treatment options. Dermatol Ther 20:31–46
Acknowledgment
The authors thank Riitta Hakola for the skilful technical assistance.
Conflicts of interest
M.R., A.S., and J.L. are shareholders of Repolar Oy, which is a new Finnish company established to develop and market coniferous resin-based products for medical practices.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rautio, M., Sipponen, A., Lohi, J. et al. In vitro fungistatic effects of natural coniferous resin from Norway spruce (Picea abies). Eur J Clin Microbiol Infect Dis 31, 1783–1789 (2012). https://doi.org/10.1007/s10096-011-1502-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-011-1502-9