Abstract
Joint replacement surgery has improved the quality of life for hundreds of thousands of patients. However, the infection of a joint implant is an important and serious complication, though the prevalence is low. Staphylococcus epidermidis is the most important pathogen involved in foreign-body infections. S. epidermidis is also a commensal that comprises a substantial part of the normal skin flora of humans. The possibility to demonstrate potential specific virulence markers may facilitate the interpretation of the bacteriological findings, as well as the clinical decision. The prevalence of the ica locus and insertion sequence IS256 by using polymerase chain reaction (PCR) among 32 clinical S. epidermidis isolates from prosthetic joint infections (PJIs) and 24 commensal isolates from nares and skin was investigated. Sixteen (50%) of the 32 PJI isolates harbored the ica operon compared with one-third of the commensal isolates obtained from the samples of the skin and nares of healthy individuals. The IS256 was demonstrated in 26 (81%) out of 32 PJI isolates. By contrast, IS256 was found in one of 24 commensal isolates. In conclusion, IS256 may be superior to the ica operon as a marker of the invasive capacity of S. epidermidis, since it was found in most of the PJI isolates, but rarely among commensals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Staphylococcus epidermidis is a natural constituent of the human skin and mucosal surfaces. With the expanding use of implanted catheters and prosthetic devices, S. epidermidis has emerged as an important nosocomial pathogen. Joint replacement surgery, one of the major medical progresses made during the 20th century, has improved the quality of life for hundreds of thousands of patients. However, the infection of a joint implant is an important and serious complication, though the prevalence is low. Nevertheless, the recovery of S. epidermidis from cultures may be difficult to interpret. The possibility to discriminate between invasive and commensal S. epidermidis isolates would facilitate clinical decision making.
S. epidermidis has the ability to produce biofilm and it has been proposed that this characteristic is the most important pathogenic factor of foreign-body infections caused by S. epidermidis [1]. Biofilm formation in S. epidermidis occurs in two essential steps; initial adherence to the implanted surface is followed by an accumulation process and the production of extracellular polysaccharide substances, such as polysaccharide intercellular adhesion (PIA) [2]. The production of PIA is mediated by the intercellular adhesion (ica) locus comprising four ica genes (icaA, icaB, icaC, and icaD) and a regulatory gene (icaR) [3–5]. Potential virulence-associated genes, such as icaADBC, aap, altE, bhp, fbe, embp, and mecA, and the phenotypic biofilm formation have been investigated to identify pathogenic S. epidermidis strains [6, 7].
The genotypic and phenotypic variability/heterogeneity of clinical S. epidermidis isolates is assumed to hold the advantage of being able to adapt to the changing environment. Genetic factors that may contribute to this development of phase variations, mutations, and chromosomal rearrangements could be mediated by insertion sequence (IS) elements. Of these, IS256 is a mobile genetic element that often resides in multiple copies on the S. epidermidis chromosome [8]. IS256 may express an important virulence factor, probably a transposase, but the mode of action of this transposase has not been elucidated [9]. In addition, IS256 can influence the ica gene expression of biofilm-forming S. epidermidis to undergo a phase variation process to a biofilm-negative phenotype [9]. It has been hypothesized that IS256 may affect the expression of genes associated with pathogenicity, and that multiple copies of IS256 make the genome of S. epidermidis more flexible and adaptable to various environments [6]. Therefore, IS256 seems to be a virulence-associated gene connected to invasive strains [6, 8].
In this study, we investigated 32 clinical S. epidermidis isolates from prosthetic joint infections (PJIs) and 24 commensal isolates from nares and skin. The aim was to determine the prevalence of the ica locus and IS256 as potential virulence markers among S. epidermidis isolated from PJIs.
Materials and methods
Bacterial isolates
Thirty-two S. epidermidis isolates obtained from patients with PJIs were analyzed. Eleven isolates were collected from 11 patients during revision operations for prosthetic hip joint infections, with extraction or exchange of the prosthetic device, treated at Linköping University Hospital from 1993 to 2003. A further 21 S. epidermidis isolates were collected from patients with infected hip (n = 13), knee (n = 7), and elbow joint (n = 1) prostheses treated at Örebro University Hospital from 2000 to 2005. During the revision operations, multiple tissue biopsies, usually comprising five or more samples, were taken, most of which displayed growth of S. epidermidis in ≥3 of the samples. In two cases, growth was present in one of three samples and in two of five samples, respectively, but an obvious perioperative clinical infection was present in both cases.
The tissue samples were immediately placed in thioglycollate broth (thioglycollate medium 3.0% w/v; BBL, Sparks, MD, USA) and cultured at 37°C for either 5 days under aerobic conditions or for 10 days under anaerobic conditions or were cultured aerobically and anaerobically for at least 5 days on blood agar plates (Columbia II Agar 4.25% w/v; horse blood, defibrinized, 6% v/v; SVA, Uppsala, Sweden), as well as in enrichment broth (fastidious anaerobe broth 29.7% w/v; Lab M, Lancashire, UK; D+ glucose 10.0% w/v; J.T. Baker, Deventer, Holland) for 7 days.
S. epidermidis representing commensal isolates was isolated from the anterior nares (n = 12) of healthy individuals without any association to health care and the skin of the wrists (n = 12) of healthy individuals (employees at the laboratory).
The isolates were identified by routine methods and characterized to the species level using ID32Staph® (bioMérieux, Marcy l’Etoile, France) and verified by rpoB sequencing [10].
The isolates were stored at −70°C in glycerol storage broth [11] or in preservation medium (yeast extract; Difco Laboratories, Sparks, MD, USA; and horse serum added to trypticase soy broth [TSB]; BBL, Sparks, MD, USA) pending further analysis. The isolates were aerobically subcultured on blood agar plates overnight at 37°C.
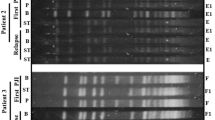
Detection of the ica gene complex and IS256 by PCR
Genomic DNA was extracted from cultures grown on blood agar plates by suspending five or six colonies in 100 μL of sterile water and subjecting them to lysis at 98°C for 15 min. The DNA samples were centrifuged at 420 × g for 5 min at 4°C and the supernatant was used for polymerase chain reaction (PCR). The concentration of DNA in the supernatant was determined using the dsDNA-binding fluorochrome PicoGreen (PicoGreen dsDNA Quantitation Kit; Molecular Probes, Leiden, the Netherlands). Measurements were recorded using a fluorescence reader (FLUOstar OPTIMA, BMG Lab Technologies, Offenburg, Germany).
The presence of the genes icaADB, icaC, icaD, and IS256, respectively, were determined using primers previously reported [6, 9, 12, 13] in all samples. PCR analysis was performed using Eppendorf’s MasterCycle PCR® (Eppendorf, Hamburg, Germany) and reagent mixtures (Roche Diagnostics, Mannheim, Germany) according to the manufacturer’s protocol. Sterile water was used as the negative control and S. epidermidis RP62A (ATCC 35984) as the positive control. See Table 1 for the detailed primer sequences and PCR conditions.
Sequencing the PCR product
The PCR products were verified and sequenced by an ABI PRISM BigDye Terminator, version 1.1, Ready Reaction Cycle Sequencing Kit (Applied Biosystems, Stockholm, Sweden), and a Gene-Amp PCR System 2700 (Applied Biosystems), using the same primers as for the PCR. Before sequencing, the products were purified with a High Pure PCR Product Purification Kit (Roche Diagnostics, Mannheim, Germany). Both strands were sequenced. Cycle sequencing was performed by 25 cycles consisting of 96°C denaturation for 10 min, annealing for 5 s at each primer’s annealing temperature, 60°C of extension for 4 min, and then cooling at +4°C. Reaction products were purified using a Qiagen DyeEx 2.0 Spin kit (VWR International, Stockholm, Sweden) and then separated on an ABI PRISM 310 Genetic Analyzer (Applied Biosystems). The nucleotide sequences were analyzed using ABI PRISM Auto Assembler DNA Sequence Assembly 1.4.0 software, and were then compared with the BLAST database at NCBI. The S. epidermidis RP62A yielded a 516 bp amplification product for icaADB, a 282 bp product for icaD (GenBank accession number U43366), a 534 bp product for icaC (AY138959.1), and a 657 bp product for IS256 (CP000029.1), and the sequences of these amplicons were identical at the levels of 100%, 100%, 97%, and 98%, respectively.
Determination of biofilm production by microtiter plate assay
Quantitative determination of biofilm production was performed using a microtiter plate (MTP) assay, as previously described [14, 15], with some modifications. In brief, S. epidermidis (five to ten colonies) isolates were inoculated in 4 mL of TSB (Trypticase Soy Broth Agar II, 4% w/v; BBL, Becton Dickinson, Sparks, MD, USA) supplemented with 0.25% glucose, and incubated overnight with shaking (30 rpm, orbital shaker; IKA-Werke, Staufen, Germany) at 37°C. This broth was then diluted 1:100 in TSB with 0.25% glucose, and 200 μL of this solution was incubated in 96-well plates overnight at 37°C. The plates were carefully washed four times with sterile phosphate-buffered saline (PBS) and air-dried before being stained with 200 μL of 0.1% safranin stain (Sigma, Stockholm, Sweden) for 30 s. The wells were washed four times with 200 μL PBS. The optical density of the adherent biofilm was determined at 490 nm, using an MTP reader (Multiscan MS, version 4.0; Labsystems, Helsinki, Finland). Each plate contained S. epidermidis RP62A (ATCC 35984) as a positive control. Pure TSB with 0.25% glucose was used as the negative control (background absorbance). The absorbance was taken to be the optical density for the isolate, minus the mean of the background control values for the same plate. Each isolate was tested in triplicate. The cut-off was set as the mean optical density of a mock-treated MTP, i.e., the background absorbance ± 3 standard deviations.
Determination of biofilm production by Congo red agar method
The isolates were cultured on Congo red agar (CRA) plates according to Freeman et al. [16], i.e., using brain heart infusion broth (Oxoid Ltd., Basingstoke, England) 37 g/L, sucrose 50 g/L, Agar No. 1 (BDH Ltd, Poole, England) 10 g/L, and Congo red (Merck KgaA, Darmstadt, Germany) 0.8 g/L. The plates were incubated aerobically for 24 h at 37°C and, subsequently, overnight at room temperature. The results regarding biofilm production were determined as positive (+) if the colonies appeared black, indeterminate (+/−) if they had a dark color, and negative (−) if they were red or pink. S. epidermidis RP62A was used as the positive control. The assessment was carried out blinded.
Results and discussion
The finding of S. epidermidis in tissue samples from foreign-body infections, such as PJIs, raises the question of how to differentiate isolates that cause infection from contaminating commensals. The possibility to demonstrate potential specific genetic markers for the invasiveness or virulence of S. epidermidis would probably facilitate the interpretation of the bacteriological findings, as well as the clinical decision.
Sixteen (50%) of the 32 S. epidermidis isolates obtained from patients with PJIs carried the ica operon. The ica operon was also found in 33% of the commensal isolates obtained from the samples of the skin and nares of healthy individuals, but the difference compared with PJI isolates was not significant (P > 0.05; Fisher’s exact test) (Table 2). In addition, there was complete congruence regarding the presence of the various ica genes, icaADB, icaC, and icaD, among the isolates that carried the ica operon.
By contrast, Galdbart et al. [17] found that the ica operon was present in 44 out of 54 isolates (81.5%), causing PJI in 14 subjects, compared with four out of 23 skin-flora strains (17.4%) from healthy individuals. In that study, S. epidermidis isolates from 12 out of 14 PJI patients were found to be ica-positive. However, our findings are in agreement with previous studies of prosthesis-associated infections [3, 18], and it has been concluded that the ica operon is not a useful diagnostic marker for PJIs [18].
Additional studies analyzing S. epidermidis isolates originating from sources other than PJIs, such as catheter-related infections, have reported diverging results, with a prevalence of the ica operon ranging from 45% to 81.5% [6, 12, 19, 20]. Also, contradictory results regarding the prevalence of the ica operon among S. epidermidis isolates from catheter-related bloodstream infections and skin isolates have been reported [13, 21]. It has been concluded that genetic markers such as the ica operon do not distinguish invasive strains from blood culture contaminants [22], since they are probably recruited from the same genetic background of strains prevalent in the hospital environment.
Biofilm production, demonstrated by the MTP assay, was found in 47% of the PJI isolates. Thirteen isolates that were ica-positive had produced biofilm, while three ica-positive isolates had not. In addition, two isolates were found to be biofilm-positive, but no ica genes could be detected by PCR. Among the commensals, seven isolates were found to be congruent regarding the presence of ica genes and biofilm production. One additional isolate was ica-positive but did not produce biofilm, and three isolates did produce biofilm, but no ica genes could be detected.
The CRA plate method, interpreted as +, +/−, or −, demonstrated seven PJI isolates that were positive (+) and also ica-positive, six that were undetermined (+/−) regarding CRA but ica-positive, and three that were negative (−) on CRA but carried the ica genes. Positive and undetermined results on CRA were also found in five and two ica-negative isolates, respectively. Among commensals, five out of eight ica-positive isolates were CRA-positive, two were +/−, and one was negative. In addition, one isolate was interpreted as +/−, despite the lack of ica genes. No statistically significant differences were found.
Consequently, a comparison of the results of the MTP assay and the CRA method for the presence of the ica operon and the phenotypic determination of biofilm production showed some discrepancies. Incongruence between the presence of the ica operon genes and the biofilm production has previously been reported [23, 24–26]. In addition, biofilm production, independently of the presence of the ica operon, has been reported for both S. aureus and S. epidermidis, as has the possibility that genes other than the ica operon may encode additional biofilm components [27–29]. However, the interpretation of the results of the CRA method is subjective and is not straightforwardly standardized.
Biofilm formation has been recognized as a major virulence determinant in S. epidermidis infections, and especially regarding foreign body infections [9]. However, despite the lack of the ica operon and/or the absence of phenotypic biofilm production, these S. epidermidis isolates are capable of producing serious and difficult-to-treat PJIs, necessitating revision and exchange operations.
In a recent study [19], a high prevalence of the ica locus was found among S. epidermidis isolated from infections of implanted devices, but there was a much lower prevalence of both the production of PIA and the formation of biofilm. This discrepancy could, in part, be explained by the presence of an insertion of IS256 within the ica operon [9].
Phenotypic variation in biofilm production may be caused by different mechanisms, such as the insertion and excision of the insertion element IS256 [9], down-regulation of ica transcript levels, or random mutation within the ica operon in IS256-negative S. epidermidis [30]. The presence of IS256 may play a role in the flexibility of the genome of S. epidermidis [3, 6, 8].
In our study, the insertion sequence IS256, determined by PCR, was demonstrated in the majority of PJI isolates (81%) (Table 2) and a statistically significant difference compared with the commensals was found (P < 0.0001). Fifty-eight percent (15/26) of the PJI isolates that carried IS256 were also found to harbor the ica operon, i.e., the concordance between the presence of the ica operon and that of IS256 was 94% (15/16) (Table 2).
By contrast, IS256 was found in one of 24 commensal isolates.
A long-range PCR was also performed, using the icaADB forward primer and the icaC reverse primer, resulting in a product of ca. 2,000 kb (BLAST accession number CP000029.1 position 2335352 to 2337579, corresponding to 2208 bp). No difference in amplicon size was found between ica-positive isolates with and ica-positive isolates without detected IS256 elements, indicating that the IS256 that was prevalent among PJI isolates was not found to be inserted within the ica locus.
The prevalence of IS256 among S. epidermidis obtained from prosthesis-associated infections has previously been reported to be 41% [3]. However, a higher prevalence has been reported in studies of catheter-related infections [6, 20]. In addition, S. epidermidis isolated from blood cultures in general [8], from bone marrow transplant patients [7], and from very-low-birth-weight neonates [22] carried IS256 in 87%, 94%, and 67% of cases, respectively. In these studies, 4%, 0%, and 0% of the commensal strains were IS256-positive, respectively.
IS256 has been shown to be inserted into the ica operon, and, thereby, turn a biofilm-forming S. epidermidis into a PIA-negative phase variant [9]. The insertion of an IS256 element into the ica operon would affect the amplicon size of the ica long-range PCR product. We could not detect any difference in the size of the long-range PCR product in any of the ica-positive strains. This is in agreement with previous studies investigating clinical S. epidermidis isolates [3, 20, 22, 30], none of which were able to demonstrate the insertion of IS256 into the ica operon. The mechanism for switching on/off the biofilm production seems not to be regulated by the insertion/excision of IS256 in the ica operon [3]. In our isolates, IS256 was inserted somewhere in the genome, except in the ica complex, and seemed to be a characteristic of pathogenic S. epidermidis strains. Generally, point mutations, mobile genetic elements, gene transfer, and recombination are mechanisms that generate genotypic and phenotypic variants. S. epidermidis is a common pathogen established in the hospital environment [8], and invasive strains seem to display a complex interplay between biofilm formation, virulence-associated genes, insertion elements, and antibiotic resistance.
In conclusion, 50% of the investigated S. epidermidis isolates lacked the ica operon, but they were still able to generate prosthetic device infections. Insertion sequence IS256 may be superior to the ica operon as a marker of the invasive capacity of S. epidermidis since it was found in most of the PJI isolates, but rarely among commensals. The reason for the high prevalence of IS256 is not fully understood and needs to be further investigated.
References
Mack D, Becker P, Chatterjee I, Dobinsky S, Knobloch JK, Peters G et al (2004) Mechanisms of biofilm formation in Staphylococcus epidermidis and Staphylococcus aureus: functional molecules, regulatory circuits, and adaptive responses. Int J Med Microbiol 294:203–212. doi:10.1016/j.ijmm.2004.06.015
Vuong C, Otto M (2002) Staphylococcus epidermidis infections. Microbes Infect 4:481–489. doi:10.1016/S1286-4579(02)01563-0
Arciola CR, Campoccia D, Gamberini S, Rizzi S, Donati ME, Baldassarri L et al (2004) Search for the insertion element IS256 within the ica locus of Staphylococcus epidermidis clinical isolates collected from biomaterial-associated infections. Biomaterials 25:4117–4125. doi:10.1016/j.biomaterials.2003.11.027
Gerke C, Kraft A, Süssmuth R, Schweitzer O, Götz F (1998) Characterization of the N-acetylglucosaminyltransferase activity involved in the biosynthesis of the Staphylococcus epidermidis polysaccharide intercellular adhesin. J Biol Chem 273:18586–18593. doi:10.1074/jbc.273.29.18586
Heilmann C, Schweitzer O, Gerke C, Vanittanakom N, Mack D, Götz F (1996) Molecular basis of intercellular adhesion in the biofilm-forming Staphylococcus epidermidis. Mol Microbiol 20:1083–1091. doi:10.1111/j.1365-2958.1996.tb02548.x
Gu J, Li H, Li M, Vuong C, Otto M, Wen Y et al (2005) Bacterial insertion sequence IS256 as a potential molecular marker to discriminate invasive strains from commensal strains of Staphylococcus epidermidis. J Hosp Infect 61:342–348. doi:10.1016/j.jhin.2005.04.017
Rohde H, Kalitzky M, Kröger N, Scherpe S, Horstkotte MA, Knobloch JK et al (2004) Detection of virulence-associated genes not useful for discriminating between invasive and commensal Staphylococcus epidermidis strains from a bone marrow transplant unit. J Clin Microbiol 42:5614–5619. doi:10.1128/JCM.42.12.5614-5619.2004
Kozitskaya S, Cho SH, Dietrich K, Marre R, Naber K, Ziebuhr W (2004) The bacterial insertion sequence element IS256 occurs preferentially in nosocomial Staphylococcus epidermidis isolates: association with biofilm formation and resistance to aminoglycosides. Infect Immun 72:1210–1215. doi:10.1128/IAI.72.2.1210-1215.2004
Ziebuhr W, Krimmer V, Rachid S, Lössner I, Götz F, Hacker J (1999) A novel mechanism of phase variation of virulence in Staphylococcus epidermidis: evidence for control of the polysaccharide intercellular adhesin synthesis by alternating insertion and excision of the insertion sequence element IS256. Mol Microbiol 32:345–356. doi:10.1046/j.1365-2958.1999.01353.x
Hellmark B, Söderquist B, Unemo M (2008) Simultaneous species identification and detection of rifampicin resistance in staphylococci by sequencing of the rpoB gene. Eur J Clin Microbiol Infect Dis. Aug 21. Epub
Feltham RK, Power AK, Pell PA, Sneath PA (1978) A simple method for storage of bacteria at −76 degrees C. J Appl Bacteriol 44:313–316
Frebourg NB, Lefebvre S, Baert S, Lemeland JF (2000) PCR-based assay for discrimination between invasive and contaminating Staphylococcus epidermidis strains. J Clin Microbiol 38:877–880
de Silva GD, Kantzanou M, Justice A, Massey RC, Wilkinson AR, Day NP et al (2002) The ica operon and biofilm production in coagulase-negative staphylococci associated with carriage and disease in a neonatal intensive care unit. J Clin Microbiol 40:382–388. doi:10.1128/JCM.40.02.382-388.2002
Christensen GD, Simpson WA, Younger JJ, Baddour LM, Barrett FF, Melton DM et al (1985) Adherence of coagulase-negative staphylococci to plastic tissue culture plates: a quantitative model for the adherence of staphylococci to medical devices. J Clin Microbiol 22:996–1006
Cramton SE, Gerke C, Schnell NF, Nichols WW, Götz F (1999) The intercellular adhesion (ica) locus is present in Staphylococcus aureus and is required for biofilm formation. Infect Immun 67:5427–5433
Freeman DJ, Falkiner FR, Keane CT (1989) New method for detecting slime production by coagulase negative staphylococci. J Clin Pathol 42:872–874. doi:10.1136/jcp.42.8.872
Galdbart JO, Allignet J, Tung HS, Rydèn C, El Solh N (2000) Screening for Staphylococcus epidermidis markers discriminating between skin-flora strains and those responsible for infections of joint prostheses. J Infect Dis 182:351–355. doi:10.1086/315660
Frank KL, Hanssen AD, Patel R (2004) icaA is not a useful diagnostic marker for prosthetic joint infection. J Clin Microbiol 42:4846–4849
Chokr A, Watier D, Eleaume H, Pangon B, Ghnassia JC, Mack D et al (2006) Correlation between biofilm formation and production of polysaccharide intercellular adhesin in clinical isolates of coagulase-negative staphylococci. Int J Med Microbiol 296:381–388. doi:10.1016/j.ijmm.2006.02.018
Petrelli D, Zampaloni C, D’Ercole S, Prenna M, Ballarini P, Ripa S et al (2006) Analysis of different genetic traits and their association with biofilm formation in Staphylococcus epidermidis isolates from central venous catheter infections. Eur J Clin Microbiol Infect Dis 25:773–781. doi:10.1007/s10096-006-0226-8
Vandecasteele SJ, Peetermans WE, Merckx R, Van Eldere J (2003) Expression of biofilm-associated genes in Staphylococcus epidermidis during in vitro and in vivo foreign body infections. J Infect Dis 188:730–737. doi:10.1086/377452
Bradford R, Abdul Manan R, Daley AJ, Pearce C, Ramalingam A, D’Mello D et al (2006) Coagulase-negative staphylococci in very-low-birth-weight infants: inability of genetic markers to distinguish invasive strains from blood culture contaminants. Eur J Clin Microbiol Infect Dis 25:283–290. doi:10.1007/s10096-006-0130-2
Cafiso V, Bertuccio T, Santagati M, Campanile F, Amicosante G, Perilli MG et al (2004) Presence of the ica operon in clinical isolates of Staphylococcus epidermidis and its role in biofilm production. Clin Microbiol Infect 10:1081–1088. doi:10.1111/j.1469-0691.2004.01024.x
Klingenberg C, Aarag E, Rønnestad A, Sollid JE, Abrahamsen TG, Kjeldsen G et al (2005) Coagulase-negative staphylococcal sepsis in neonates. Association between antibiotic resistance, biofilm formation and the host inflammatory response. Pediatr Infect Dis J 24:817–822. doi:10.1097/01.inf.0000176735.20008.cd
Arciola CR, Campoccia D, Baldassarri L, Donati ME, Pirini V, Gamberini S et al (2006) Detection of biofilm formation in Staphylococcus epidermidis from implant infections. Comparison of a PCR-method that recognizes the presence of ica genes with two classic phenotypic methods. J Biomed Mater Res A 76:425–430. doi:10.1002/jbm.a.30552
Chaieb K, Mahdouani K, Bakhrouf A (2005) Detection of icaA and icaD loci by polymerase chain reaction and biofilm formation by Staphylococcus epidermidis isolated from dialysate and needles in a dialysis unit. J Hosp Infect 61:225–230. doi:10.1016/j.jhin.2005.05.014
Henning S, Peter-Katalinić J, Pohlentz G (2007) Structure elucidation of glycoproteins by direct nanoESI MS and MS/MS analysis of proteolytic glycopeptides. J Mass Spectrom 42:1415–1421. doi:10.1002/jms.1265
Fitzpatrick F, Humphreys H, O’Gara JP (2005) Evidence for icaADBC-independent biofilm development mechanism in methicillin-resistant Staphylococcus aureus clinical isolates. J Clin Microbiol 43:1973–1976. doi:10.1128/JCM.43.4.1973-1976.2005
Rohde H, Burandt EC, Siemssen N, Frommelt L, Burdelski C, Wurster Set al (2007) Polysaccharide intercellular adhesin or protein factors in biofilm accumulation of Staphylococcus epidermidis and Staphylococcus aureus isolated from prosthetic hip and knee joint infections. Biomaterials 28:1711–1720. doi:10.1016/j.biomaterials.2006.11.046
Handke LD, Conlon KM, Slater SR, Elbaruni S, Fitzpatrick F, Humphreys H et al (2004) Genetic and phenotypic analysis of biofilm phenotypic variation in multiple Staphylococcus epidermidis isolates. J Med Microbiol 53:367–374. doi:10.1099/jmm.0.05372-0
Acknowledgments
We are sincerely obliged to Carolina Berglund for her excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Koskela, A., Nilsdotter-Augustinsson, Å., Persson, L. et al. Prevalence of the ica operon and insertion sequence IS256 among Staphylococcus epidermidis prosthetic joint infection isolates. Eur J Clin Microbiol Infect Dis 28, 655–660 (2009). https://doi.org/10.1007/s10096-008-0664-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-008-0664-6