Abstract
The role of Streptococcus pneumoniae in the etiology of respiratory tract infections has been studied serologically using microbe-specific antibody and immune complex assays. Serological methods are sensitive in the bacteremic pneumococcal pneumonia of adults. In children, however, pneumococcal pneumonia is seldom bacteremic, and, thus, in the absence of a gold standard for the detection of pneumococcal infection, serological methods are still insufficiently validated. We report here indirect evidence for the sensitivity and specificity of pneumococcal serology in children. Serological evidence of pneumococcal infection has been found in 27% to 38% of children with radiologically confirmed pneumonia, in 7% to 8% of children with viral wheezy bronchitis, and in <1% to 5% of children and young adults with viral upper respiratory infection. Serological findings for pneumococcal infection have been dependent on the study venue, whether in hospital or ambulatory subjects, and on the test panel used. Where both antibody and immune complex assays have been available, the proportion of children with pneumococcal infection has been 32% to 37% in inpatients and 27% to 28% in outpatients. The respective rates have been 10% to 18% by antibody assays alone. Pneumococcal acute otitis media, when present with pneumonia, may confound findings in pneumococcal serology, but pure nasopharyngeal carriage of S. pneumoniae has little effect. In contrast, carriage acquisition of a new serotype may induce significant antibody production. Thus, understandably, significant rises between paired sera in antibodies to pneumococcal capsular polysaccharides and pneumococcal pneumolysin have been found in <1% to 3% of non-symptomatic children and young adults. Findings from the last 20 years indirectly suggest that pneumococcal antibody and immune complex assays are sensitive and specific enough for the detection of pneumococcal infection in children. However, the methods are too complex for routine clinical practice, and, so far, serological methods for S. pneumoniae infections have only been used for research purposes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Streptococcus pneumoniae is the most important bacterial cause of respiratory tract infections in children. Either alone or as a co-pathogen, pneumococcus causes at least a third of community-acquired pneumonia (CAP) in children [1, 2]. The clinical manifestations vary from mild to severe with complications [1, 3, 4]. S. pneumoniae is also common in mixed viral–bacterial infections [5].
Microbe-specific etiological diagnosis of bacterial CAP and other acute lower respiratory infections (ALRI) is difficult. S. pneumoniae grows in blood culture in less than 5% of pediatric CAP cases [1, 2], and in pleural fluid, when present, in less than 20% [1, 2]. Invasive methods allowing the direct detection of pathogens from the infection focus, such as bronchoalveolar lavage, transtracheal aspiration, or transthoracic aspiration, are justified in severe cases only. The carriage of S. pneumoniae, especially in young children, is so common that upper respiratory tract samples, whether studied by culture, antigen detection, or DNA detection, have no role in the investigation of the etiology of lower respiratory infections [1, 2, 6].
In the last 20 years, bacterial antibody and immune complex assays have been used to determine the pneumococcal etiology of CAP and ALRI in children [7–16]. These methods have also been applied to upper and lower respiratory infections, such as the common cold [17], laryngitis [18, 19], and bronchiolitis and wheezy bronchitis [20, 21]. The assumption is, like in the case of many other microbes, that the production of pneumococcal antibodies or the formation of circulating pneumococcal antigen–antibody complexes, indicate that the infection is caused by S. pneumoniae [16, 22, 23]. In these serological studies, the pneumococcal antigens used have been capsular C-polysaccharide, capsular type-specific polysaccharides, and a protein antigen, pneumolysin [24–27]. However, antibody and immune complex assays are still incompletely validated for the microbe-specific diagnosis of pneumococcal infection.
This review summarizes pneumococcal antibody and immune complex findings in studies on the etiology of pediatric CAP and ALRI. The findings are compared with those obtained from children and young adults with viral upper and lower respiratory tract infections. In addition, the available validation data in relation to blood, pleural fluid, and lung aspirate cultures, mainly derived from adults with severe pneumonia, are presented. According to current knowledge, common cold, laryngitis, and wheezy bronchitis in children, as well as bronchiolitis in infants, are caused by viruses. In addition, wheezing may be associated with atypical intracellular bacteria [28–30]. In both viral and atypical bacterial cases, pneumococcal co-infections may occur, but clinically significant serological findings are expected to be rare [31, 32].
Methods for detecting specific pneumococcal antibodies and antigens
Table 1 summarizes the serological methods for S. pneumoniae used in the studies included in the present review [7–15, 33, 34]. In the antibody assays, IgG antibodies to capsular C-polysaccharide, to capsular type-specific polysaccharides (the 11 most common strains in children), and IgM and IgG antibodies to a protein antigen, pneumolysin, have been measured by enzyme immunoassay (EIA). On the basis of measurements in healthy children, the cut-off limit has been a ≥3-fold increase in antibodies to C-polysaccharide and type-specific polysaccharides and a ≥2-fold increase in antibodies to pneumolysin between paired sera [7–15, 27, 33–35]. In the immune complex assays, the circulating complexes must first be precipitated, then dissolved, and, thereafter, the antibodies can be measured by EIA [16]. The concentration of ≥2 SD over the mean of samples from healthy children, present in either acute or convalescent serum samples, has been used as a diagnostic limit [10–14, 16]. Pneumococcal surface adhesin A is an immunogenic protein common to all serotypes of S. pneumoniae, and, in some recent studies, antibodies to and immune complexes with adhesin A have been used to diagnose pneumococcal infection [36, 37].
In this review, findings by methods for serum and urine pneumococcal antigens are not reported in detail, since these tests lack sufficient sensitivity and specificity for application to clinical practice or clinical studies in children. The Binax NOW immunochromatographic test detects pneumococcal C- polysaccharide in urine, and has had promising results in adults with pneumonia. Sensitivities of 66% to 100% and specificities of 82% to 100% have been reported from many studies [38–42]. The results in children have been less promising [43–47]. In a study of 346 children, the test was positive in 95% of children with pneumococcal bacteremia, in 15% of children with non-bacteremic infection, and in 8% of controls with no current or recent infection [45]. The main problem in children is that the test has been positive in 25% to 55% of pneumococcal carriers [43, 44, 46, 47].
Pneumonia
As seen in Table 2, evidence of S. pneumoniae infection has been found in 16% to 38% of hospitalized children with CAP [7–15, 33, 34]. Only studies of western child populations with assays of antibodies to S. pneumoniae, atypical bacteria, and respiratory viruses available were included.
The lowest rates (16%) for S. pneumoniae etiology come from the two oldest studies [7, 8], in which chest radiographs were not obtained. Thus, the findings represent all ALRI cases, including both pneumonia and other lower airway infections. In later CAP studies, pneumococcal antibody assays were supplemented by immune complex assays, and serological evidence of S. pneumoniae infection was documented in over 30% of cases [10, 14, 33, 34]. When the proportions of pneumococcal etiology were calculated from those with any etiology detected, the rates were 23% to 52% in hospital studies and 19% to 63% in ambulatory studies (Table 3).
Serum and urine antigens were measured in four hospital studies, whose approaches increased the proportion of pneumococcal findings by 4% to 16% [7–10, 14, 27]. In the only population-based CAP study, the detection of urine antigens did not increase pneumococcal findings [12, 35].
Vuori et al. [48] studied pneumococcal antibodies and immune complexes in 79 children hospitalized for pneumonia and in 30 children hospitalized for ALRI with no pneumonia. Only severely ill patients requiring parental antibiotic therapy were included. Pneumococcal antibodies or immune complexes were present in 36 (46%) and 9 (30%) of the cases, respectively [48]. Esposito et al. [49] measured capsular type-specific antibodies to S. pneumoniae and antibodies to atypical bacteria, but not to viruses, in 196 children hospitalized for CAP, and found evidence for pneumococcal infection in 25% of the cases [49].
Juvén et al. [50] compared clinical and laboratory findings in 38 children with serologically indicated pneumococcal pneumonia, in 26 children with respiratory syncytial virus (RSV) pneumonia, and in 85 children with bacteremic pneumococcal pneumonia. The serological diagnosis of pneumococcal infection was made by measuring IgG antibodies to pneumolysin and C-polysaccharide, and immune complexes containing these antigens and respective antibodies. Serologically indicated pneumococcal pneumonia was significantly associated with alveolar infiltrates on the chest radiograph (76% vs. 15% in RSV pneumonia), elevated white blood cells (20.8×109/L (mean) vs. 12.0×109/L), and elevated serum C-reactive protein (137 mg/L (mean) vs. 28 mg/L) [50]. The results offer indirect evidence for the specificity of pneumococcal serology. However, only 34% of the patients had typical pneumococcal pneumonia (acute onset, high fever, leukocytosis, and lobar infiltrates), compared with 70% of patients with bacteremic pneumonia [50].
Etiological findings from CAP studies in children seem to depend at least on four factors: study design, age distribution, severity of disease, and the microbe-specific test panel used. In hospital studies, young children and severe cases are over-represented, emphasizing the role of viruses and S. pneumoniae [9–11, 14, 50]. In ambulatory studies, performed in outpatient clinics [7, 13, 15], and especially in population-based studies carried out in primary health care [12, 51], the disease is milder and the patients are older, stressing the role of atypical bacteria, such as M. pneumoniae and C. pneumoniae. Different serological tests for pneumococcal infection seem to find different cases [11, 27, 35]. This may be due to insufficient test sensitivity and specificity. In addition, the timing of sampling may play a role [22, 23]. Finally, the rates of diagnostic findings may simply depend on the size of the test panel used [11, 27, 34, 38].
Common cold, laryngitis, bronchiolitis, and wheezy bronchitis
As seen in Table 4, pneumococcal infection was serologically diagnosed in only one case (0.5%) of 199 young adults with the common cold [17]. S. pneumoniae was cultured from the nasopharynx in an additional eight cases. An antibody response to S. pneumoniae was found in 5% of the 65 children with laryngitis [18]. Another study found no cases of pneumococcal infection in 24 children with acute laryngitis caused by parainfluenza viruses, which are typical causative agents of laryngitis [19]. The figure was slightly higher, 7%, in 188 preschool children hospitalized for infection-associated wheezing [20]. In that study, 42% of the patients had mainly interstitial infiltrates on chest radiographs, and no significant differences were seen in bacterial serology between cases with and without radiological findings. In a recent study, viral etiology was found in 88% of 220 wheezing children [52], and serological evidence of pneumococcal co-infection was present in 17 (8%) cases [21]. The figure was 10% in 40 RSV, 11% in 54 rhinovirus, and 9% in 44 enterovirus-positive cases. Chest radiographs showed interstitial infiltrates in 43% and alveolar infiltrates in 4% of the patients, with no significant association with findings in pneumococcal serology. Pneumococcal infection was found in 9% of the 85 bronchiolitis and in 5% of the 103 wheezy bronchitis patients. Acute otitis media was diagnosed in 96 children, with no association with serological pneumococcal findings [21].
Acute otitis media
Acute otitis media induces both local and systemic antibody production against the causative agent. Koskela et al. [24, 25, 53] found that responses to pneumococcal capsular polysaccharides were rather common, from 21% (IgG responses to C-polysaccharide) to 36% (IgG and/or IgM responses to type-specific polysaccharides) in 114 children with acute otitis media. However, antibody responses to pneumolysin were rare, <10%, and nearly all were IgA responses. Another study found an IgG response to pneumolysin in 2% (IgA in 7%) and an IgG response to capsular polysaccharides in 14% (IgA in 7%) in 121 children with acute otitis media [54].
In a recent study, 329 children were followed from 2 to 24 months of age, and antibodies to capsular polysaccharides, pneumolysin, and surface adhesin A were measured 6 months apart [55, 56]. In addition, the children were examined for otitis media, and paired sera were obtained for antibody measurements during all respiratory infections. Pneumococcal antibodies showed no association with the otitis history [55, 57]. The number of children with acute otitis media was 185, and, among them, 22 (12%) had a ≥2-fold increase in antibodies to type-specific capsular polysaccharides [56], 25 (14%) to surface adhesin A and 17 (9%) to pneumolysin [58]. In the subgroup of children with pneumococcal otitis media, 28% had an antibody response to pneumolysin, and 21% had a homologous and 6% a heterologous antibody response to capsular polysaccharides (Table 5). Thus, the presence of pneumococcal otitis media may confound the serologic diagnosis of pneumococcal CAP.
Healthy children
The data on antibody and immune complex responses in healthy children originate from vaccination studies [24, 25, 53]. Children with ongoing or recent respiratory infections have not been included in these studies. Table 6 shows the validation data of healthy controls. Significant antibody responses to C-polysaccharide and capsular polysaccharides (≥3-fold increase between paired sera) were seen in less than 1% of 200 children and young adults [32], and a significant antibody response to pneumolysin (≥2-fold increase between paired sera) was seen in 2–3% of 188 children attending the studies [23]. Circulating immune complexes with C-polysaccharide, capsular polysaccharides and/or pneumolysin, and respective IgM or IgG antibodies were each seen in 1–2% of 89 non-symptomatic children [16].
The carriage of S. pneumoniae and development of pneumococcal antibodies were prospectively monitored in 329 children, aged <24 months [55–58]. Nasopharyngeal aspirates were obtained for culture during respiratory infections, and in addition, throat swabs were obtained and serum antibodies to capsular polysaccharides and to protein antigens pneumolysin and surface adhesin A were measured at ages of 6, 12, 18 and 24 months. The concentrations of antibodies to all these antigens increased with age. Earlier contacts with S. pneumoniae, either documented carriage or pneumococcal otitis media, had a significant association with the concentrations of antibodies to protein antigens but not with those to polysaccharide antigens [55, 56]. Pneumococcal carriage was infrequently, in 7% to 10% of the cases, associated with significant increases of pneumococcal antibodies in paired sera (Table 5). Since all children were new carriers, the responses seem to be associated with carriage acquisition.
Validation by blood culture
Serological findings in bacteremic, blood culture-positive, pneumococcal pneumonia have been mainly studied in adults. As Table 7 shows, the sensitivity of bacterial serology, when compared with positive blood culture, seems to be good, from 68% to 92% [26, 59–61]. However, the available data are based on low numbers of patients, and in the absence of a gold standard for non-bacteremic pneumococcal pneumonia, the final performance of pneumococcal serology cannot be calculated. In the four adult studies, pneumococcal serology was positive in 21% to 61% of non-bacteremic pneumonia cases [26, 59–61].
The etiology of infection was studied by blood and lung aspiration cultures and by serology in 74 Gambian children hospitalized for severe pneumonia [62]. The sensitivity of pneumolysin antibodies and immune complexes when compared with 17 culture-positive cases was 47%. In 222 Australian Aboriginal children with 322 ALRI episodes, blood culture was positive for S. pneumoniae in only six cases [63]. Of them, either pneumolysin antibodies or immune complexes were found in four cases (67%).
In the study of Michelow et al. [34] from the USA, paired sera were available from 119 children hospitalized for CAP, and 12 (10%) of them were blood or pleural culture-positive for S. pneumoniae. Eleven (92%) of them were correctly identified by pneumococcal antibody assays, whereas immune complex assays detected only 6 (50%) patients. Antibody assays were negative in 40 (95%) of the 42 controls. These figures mean a 92% sensitivity and 95% specificity in the diagnosis of bacteremic pneumococcal pneumonia. On the other hand, pneumococcal infection was identified by polymerase chain reaction (PCR) as often as in 44% of all cases, having a 100% sensitivity and 63% specificity compared with blood or pleural cultures, and 95% specificity compared with healthy controls [14, 34].
Validation by invasive methods in adults
In adult studies, the use of immune complexes for the diagnosis of pneumococcal pneumonia has been questioned. Musher et al. [64] compared type-specific antibodies to pneumococcal capsular polysaccharides in adults admitted for bacteremic and non-bacteremic pneumonia, as well as in healthy controls, and found that the concentrations were similar in all three groups. In another study, Musher et al. [65] found pneumolysin IgG immune complexes in 60% of 15 patients with non-bacteremic pneumococcal pneumonia, in 63% of 16 healthy carriers, and in 23% of 22 healthy non-carriers. This means a sensitivity of 60% and a specificity of 61% when carriers are included, and a specificity of 77% when carriers are not included. In an older study, Holloway et al. [66] found pneumolysin IgG immune complexes in 85% of 20 adults with bacteremic pneumonia and in 33% of other pneumonia cases. This means a sensitivity of 85% and a specificity of 67%.
In studies from Kenya, serum IgG to pneumococcal surface adhesin A was measured in the paired sera of 109 adults with pneumococcal pneumonia, diagnosed by culture in blood, pleural fluid, or lung aspirates, or by the presence of pneumococcal antigen in urine, and in 47 healthy controls [36, 37]. By a 2-fold or greater increase in antibody concentrations, the sensitivity was 70% and the specificity was 98%.
Serum immune complexes to pneumolysin, C-polysaccharide, and mixed type-specific capsular polysaccharides were measured in 74 adults with pneumococcal pneumonia, diagnosed by blood, pleural fluid, or lung aspirate cultures, and in 97 sick controls with non-pneumococcal diseases [37]. At the specificity level of 90%, sensitivities were low; 32% (pneumolysin), 34% (C-polysaccharide), and 30% (capsular polysaccharide) for the identification of a pneumococcal infection.
Validation by invasive methods in children
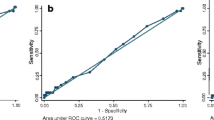
A study from Kenya included 98 children, aged 1 to 7 years, with pneumococcal pneumonia confirmed by blood or pleural fluid cultures. The sensitivity of the serological methods when these children were compared with 97 healthy, age-matched controls was 42% (95% CI 32–52%), and the specificity was 97% (95% CI 91–99%) [67]. The results were not dependent on the nasopharyngeal carriage of S. pneumoniae.
In 350 Philippine children with pneumonia, immune complexes containing pneumolysin IgG were positive in 39% of cases, those containing capsular polysaccharides in 10%, and those containing C-polysaccharides in 9% of cases, respectively [68]. However, a 2-fold or greater rise between paired sera was found only in 4% to 7% of the patients [68]. The design of the study did not allow any calculation of the diagnostic parameters.
Limitations
Although the sensitivity of pneumococcal serology seems to be rather good in bacteremic pneumonia of adults, the sensitivity in non-bacteremic cases has remained undetermined, mainly owing to the lack of gold standard methods. Over 95% of CAP cases in children are blood culture-negative. Likewise, the diagnostic cut-off limits of the tests, assessed by comparing antibody or immune complex concentrations in patients with pneumonia to those in healthy controls, are not sufficiently validated.
In children, the diagnosis of pneumococcal infection may be even more challenging than in adults, since pneumococcal carriage, and, consequently, carriage acquisition of a new serotype is common before school age. The findings of Musher et al. [69] in military conscripts support the importance of carriage acquisition. The carriage of a new pneumococcal serotype, identified during an outbreak, increased seropositivity by about 30% compared with non-carriers.
The measurement of antibodies to protein antigens, such as pneumolysin or adhesins, seems to make better sense than the measurement of antibodies to polysaccharide antigens. Protein antigens are more immunogenic than polysaccharides. In addition, 5% to 10% of patients do not adequately respond to polysaccharide antigens [70], and some type-specific polysaccharide antigens are weak antigens, particularly in young children [24, 25, 27, 35]. Antibody and immune complex assays mainly detect different cases [16, 33]. This may be due to the timing of the different phases of an immunological cascade. The composition of circulating immune complexes requires both antigens and antibodies in sufficient amounts, and only excess antigens or antibodies are measurable as free, soluble antigens or antibodies. However, the testing of antibodies for capsular polysaccharides, C-polysaccharide, and pneumolysin also seems to detect separate cases, as also do immune complex tests specific for the antigens and their corresponding antibodies [27, 35]. There is no sensible explanation for this, and, therefore, the specificity of both antibody and immune complex assays have been questioned. Finally, the measurements, especially those for immune complexes, have been made in only a few research laboratories, although the samples have originated from many surveys and countries.
Conclusions
Three conclusions seem to be justified on the basis of the currently available literature on pneumococcal serology in respiratory infections in children. First, the proportion of responses in pneumococcal serology shows a significant association with the anatomical level of the respiratory infection. Pneumococcal findings are most common in children with pneumonia, the next most common in children with acute lower respiratory infections (ALRI), rare in children with viral respiratory syndromes like bronchiolitis and wheezy bronchitis, and nearly absent in children and young adults with viral upper respiratory infection. Second, the numbers of pneumococcal findings are dependent on the study venue, whether in a hospital or an ambulatory setting, as well as on the size of the test panel used. Third, studies of pneumococcal carriage, carriage acquisition, and otitis media caused by Streptococcus pneumoniae suggest that community-acquired pneumonia (CAP) studies may be confounded by pneumococcal otitis media and carriage acquisition, but not by pneumococcal carriage alone. Carriage acquisition may play a significant role during outbreaks of S. pneumoniae infections, as seen in military conscripts, and in preschool children, in whom the development of type-specific immunity to the 90 serotypes of S. pneumoniae requires repeated contacts with all of these strains.
When compared with data obtained from blood cultures or from samples obtained by invasive procedures like pleural fluid or lung tissue aspirates, mainly available in adults, pneumococcal serology seems to be rather sensitive in the diagnosis of bacteremic pneumococcal disease. However, the sensitivity and specificity in non-bacteremic pneumonia have remained undetermined, mainly owing to the lack of any gold standard method.
References
McIntosh K (2002) Community-acquired pneumonia in children. N Engl J Med 346:429–437
Korppi M (2003) Community-acquired pneumonia in children: issues in optimizing antibacterial treatment. Paediatr Drugs 5:821–832
Byington CL, Spencer LY, Johnson TA et al (2002) An epidemiological investigation of a sustained high rate of pediatric parapneumonic empyema: risk factors and microbiological associations. Clin Infect Dis 34:434–440
Toikka P, Virkki R, Mertsola J et al (1999) Bacteremic pneumococcal pneumonia in children. Clin Infect Dis 29:568–572
Korppi M (2002) Mixed microbial aetiology of community-acquired pneumonia in children. APMIS 110:515–522
Korppi M, Katila M-L, Kalliokoski R et al (1992) Pneumococcal finding in a sample from upper airways does not indicate pneumococcal infection of lower airways. Scand J Infect Dis 24:445–451
Claesson B, Trollfors B, Brolin I et al (1989) Etiology of community-acquired pneumonia in children based on antibody responses to bacterial and viral antigens. Pediatr Infect Dis J 8:856–862
Nohynek H, Eskola J, Laine E et al (1991) The causes of hospital-treated acute lower respiratory tract infection in children. Am J Dis Child 145:618–622
Ruuskanen O, Nohynek H, Ziegler T et al (1992) Pneumonia in childhood: etiology and response to antimicrobial therapy. Eur J Clin Microbiol Infect Dis 11:217–223
Korppi M, Heiskanen-Kosma T, Jalonen E et al (1993) Aetiology of community-acquired pneumonia in children treated in hospital. Eur J Pediatr 152:24–30
Juvén T, Mertsola J, Waris M et al (2000) Etiology of community-acquired pneumonia in 254 hospitalized children. Pediatr Infect Dis J 19:293–298
Heiskanen-Kosma T, Korppi M, Jokinen C et al (1998) Etiology of childhood pneumonia: serologic results of a prospective, population-based study. Pediatr Infect Dis J 17:986–991
Wubbel L, Muniz L, Ahmed A et al (1999) Etiology and treatment of community-acquired pneumonia in ambulatory children. Pediatr Infect Dis J 18:98–104
Michelow IC, Olsen K, Lozano J et al (2004) Epidemiology and clinical characteristics of community-acquired pneumonia in hospitalized children. Pediatrics 113:701–707
Don M, Fasoli L, Paldanius M et al (2005) Aetiology of community-acquired pneumonia: serological results of a paediatric survey. Scand J Infect Dis 37:806–812
Korppi M, Leinonen M (1998) Pneumococcal immune complexes in the diagnosis of lower respiratory tract infections in children. Pediatr Infect Dis J 17:992–995
Mäkelä M, Puhakka T, Ruuskanen O et al (1998) Viruses and bacteria in the etiology of the common cold. J Clin Microbiol 36:539–542
Korppi M, Launiala K, Leinonen M et al (1990) Bacterial involvement in laryngeal infections in children. Acta Paediatr Scand 79:564–565
Korppi M, Leinonen M, Mäkelä PH et al (1990) Bacterial involvement in parainfluenza virus infection in children. Scand J Infect Dis 22:307–312
Korppi M, Leinonen M, Koskela M et al (1991) Bacterial infection in under school age children with expiratory difficulty. Pediatr Pulmon 10:254–259
Lehtinen P, Jartti T, Virkki R et al (2006) Bacterial coinfections in children with viral wheezing. Eur J Clin Microbiol Infect Dis 25:463–469
Leinonen M (1994) Serological diagnosis of pneumococcal pneumonia—will it ever become a clinical reality? Semin Respir Infect 9:189–191
Nohynek H, Eskola J, Kleemola M et al (1995) Bacterial antibody assays in the diagnosis of acute lower respiratory tract infection in children. Pediatr Infect Dis J 14:478–484
Koskela M (1986) Antibody response of young children to parenteral vaccination with pneumococcal capsular polysaccharides: a comparison between antibody levels in serum and middle ear effusion. Pediatr Infect Dis 5:431–434
Koskela M (1987) Serum antibodies to pneumococcal C polysaccharide in children: response to acute pneumococcal otitis media or to vaccination. Pediatr Infect Dis J 6:519–526
Jalonen E, Paton J, Koskela M et al (1989) Measurement of antibody responses to pneumolysin—a promising method for the presumptive aetiological diagnosis of pneumococcal pneumonia. J Infect 19:127–134
Korppi M, Koskela M, Jalonen E et al (1992) Serologically indicated pneumococcal respiratory infection in children. Scand J Infect Dis 24:437–443
Freymyth F, Vabret A, Brouard J et al (1999) Detection of viral, Chlamydia pneumoniae and Mycoplasma pneumoniae infections in exacerbations of asthma in children. J Clin Virol 13:131–139
Esposito S, Blasi F, Arosio C et al (2000) Importance of acute Mycoplasma pneumoniae and Chlamydia pneumoniae infections in children with wheezing. Eur Respir J 16:1142–1146
Biscardi S, Lorrot M, Marc E et al (2004) Mycoplasma pneumoniae and asthma in children. Clin Infect Dis 38:1341–1346
Hall CB, Powell KR, Schnabel KC et al (1988) Risk of secondary bacterial infection in infants hospitalized with respiratory syncytial viral infection. J Pediatr 113:266–271
Korppi M, Leinonen M, Koskela M et al (1989) Bacterial coinfection in children hospitalized with respiratory syncytial virus infections. Pediatr Infect Dis J 8:687–692
Korppi M, Leinonen M (1997) Pneumococcal pneumonia in children; new data from circulating immune complexes. Eur J Pediatr 156:341–342
Michelow IC, Lozano J, Olsen K et al (2002) Diagnosis of Streptococcus pneumoniae lower respiratory infection in hospitalized children by culture, polymerase chain reaction, serological testing, and urinary antigen detection. Clin Infect Dis 34:E1–E11
Heiskanen-Kosma T, Korppi M, Leinonen M (2003) Serologically indicated pneumococcal pneumonia in children: a population-based study in primary care settings. APMIS 111:945–950
Scott JA, Hall AJ, Leinonen M (2000) Validation of immune-complex enzyme immunoassays for diagnosis of pneumococcal pneumonia among adults in Kenya. Clin Diagn Labor Immunol 7:64–67
Scott JA, Obiero J, Hall AJ et al (2002) Validation of immunoglobulin G enzyme-linked immunosorbent assay for antibodies to pneumococcal surface adhesin A in the diagnosis of pneumococcal pneumonia among adults in Kenya. J Infect Dis 186:220–226
Gutiérrez F, Masiá M, Rodríguez J et al (2003) Evaluation of the immunochromatographic Binax NOW assay for detection of Streptococcus pneumoniae urinary antigen in a prospective study of community-acquired pneumonia in Spain. Clin Infect Dis 36:286–292
Marcos MA, Jiménez de Anta MT, de la Bellecasa JP et al (2003) Rapid urinary antigen test for diagnosis of pneumococcal community-acquired pneumonia in adults. Eur Respir J 21:209–214
Smith MD, Derrington P, Evans R et al (2003) Rapid diagnosis of bacteremic pneumococcal infections in adults by using the Binax NOW Streptococcus pneumoniae urinary antigen test: a prospective, controlled clinical evaluation. J Clin Microbiol 41:2810–2813
Rosón B, Fernández-Sabé N, Carratalà J et al (2004) Contribution of a urinary antigen assay (Binax NOW) to the early diagnosis of pneumococcal pneumonia. Clin Infect Dis 38:222–226
Strålin K, Kaltoft M, Konradsen H et al (2004) Comparison of two urinary antigen tests for establishment of pneumococcal etiology of adult community-acquired pneumonia. J Clin Mirobiol 42:3620–3625
Dowell S, Garman R, Liu G et al (2001) Evaluation of Binax NOW, an assay for the detection of pneumococcal antigen in urine samples, performed among pediatric patients. Clin Infect Dis 32:824–825
Hamer DH, Egas J, Estrella B et al (2002) Assessment of the Binax NOW Streptococcus pneumoniae urinary antigen test in children with nasopharyngeal pneumococcal carriage. Clin Infect Dis 34:1025–1028
Neuman MI, Harper MB (2003) Evaluation of a rapid urine antigen assay for the detection of invasive pneumococcal disease in children. Pediatrics 112:1279–1282
Domínguez J, Blanco S, Rodrigo C et al (2003) Usefulness of urinary antigen detection by an immunochromatographic test for diagnosis of pneumococcal pneumonia in children. J Clin Microbiol 41:2161–2163
Esposito S, Bosis S, Colombo R et al (2004) Evaluation of rapid assay for detection of Streptococcus pneumoniae urinary antigen among infants and young children with possible invasive pneumococcal disease. Pediatr Infect Dis J 23:365–367
Vuori E, Peltola H, Kallio M et al (1998) Etiology of pneumonia and other common childhood infections requiring hospitalization and parenteral antimicrobial therapy. Clin Infect Dis 27:566–572
Esposito S, Bosis S, Cavagna R et al (2002) Characteristics of Streptococcus pneumoniae and atypical bacterial infections in children 2–5 years of age with community-acquired pneumonia. Clin Infect Dis 35:1345–1352
Juvén T, Mertsola J, Toikka P et al (2001) Clinical profile of serologically diagnosed pneumococcal pneumonia. Pediatr Infect Dis J 20:1028–1033
Korppi M, Heiskanen-Kosma T, Kleemola M (2004) Incidence of community-acquired pneumonia in children caused by Mycoplasma pneumoniae: serological results of a prospective, population-based study in primary health care. Respirology 9:109–114
Jartti T, Lehtinen P, Vuorinen T et al (2004) Respiratory picornaviruses and respiratory syncytial virus as causative agents of acute expiratory wheezing in children. Emerg Infect Dis 10:1095–1101
Koskela M, Leinonen M, Luotonen J (1982) Serum antibody response to pneumococcal otitis media. Pediatr Infect Dis 1:245–252
Virolainen A, Jero J, Chattopadhyay P et al (1996) Comparison of serum antibodies to pneumolysin with those to pneumococcal capsular polysaccharides in children with acute otitis media. Pediatr Infect Dis J 15:128–133
Soininen A, Pursiainen H, Kilpi T et al (2001) Natural development of antibodies to pneumococcal capsular polysaccharides depends on the serotype: association with pneumococcal carriage and acute otitis media in young children. J Infect Dis 184:569–576
Soininen A, Lahdenkari M, Kilpi T et al (2002) Antibody response to pneumococcal capsular polysaccharides in children with acute otitis media. Pediatr Infect Dis J 21:186–192
Rapola S, Jäntti V, Haikala R et al (2000) Natural development of antibodies to pneumococcal surface protein A, pneumococcal surface adhesin A, and pneumolysin in relation to pneumococcal carriage and acute otitis media. J Infect Dis 182:146–152
Rapola S, Kilpi T, Lahdenkari M et al (2001) Antibody response to the pneumococcal proteins pneumococcal surface adhesin A and pneumolysin in children with acute otitis media. Pediatr Infect Dis J 20:482–487
Kalin M, Kanclerski K, Granström M et al (1987) Diagnosis of pneumococcal pneumonia by enzyme-linked immunosorbent assay of antibodies to pneumococcal hemolysin (pneumolysin). J Clin Microbiol 25:226–229
Kanclerski K, Blomquist S, Granström M et al (1988) Serum antibodies to pneumolysin in patients with pneumonia. J Clin Microbiol 26:96–100
Porath A, Schlaeffer F, Pick N et al (1997) Pneumococcal community-acquired pneumonia in 148 hospitalized adult patients. Eur J Clin Microbiol Infect Dis 16:863–870
Forgie I, O’Neill K, Lloyd-Evans N et al (1991) Etiology of acute lower respiratory tract infections in Gambian children. II: acute lower respiratory tract infection in children ages one to nine years presenting at the hospital. Pediatr Infect Dis J 10:42–47
Torzillo P, Dixon J, Manning K et al (1999) Etiology of acute lower respiratory tract infection in Central Australian Aboriginal children. Pediatr Infect Dis J 18:714–721
Musher DM, Phan HM, Watson DA et al (2000) Antibody to capsular polysaccharide of Streptococcus pneumoniae at the time of hospital admission for pneumococcal pneumonia. J Infect Dis 182:156–167
Musher DM, Mediwala R, Phan HM et al (2001) Nonspecificity of assaying for IgG antibody to pneumolysin in circulating immune complexes as a means to diagnose pneumococcal pneumonia. Clin Infect Dis 32:534–538
Holloway Y, Snijder JA, Boersma WG (1993) Demonstration of circulating pneumococcal immunoglobulin G immune complexes in patients with community-acquired pneumonia by means of an enzyme-linked immunosorbent assay. J Clin Microbiol 31:3247–3254
Scott JA, Mlacha Z, Nyiro J et al (2005) Diagnosis of invasive pneumococcal disease among children in Kenya with enzyme-linked immunosorbent assay for immunoglobulin G antibodies to pneumococcal surface adhesin A. Clin Diagn Labor Immunol 12:1195–1201
Lankinen KS, Ruutu P, Nohynek H et al (1999) Pneumococcal pneumonia diagnosis by demonstration of pneumolysin antibodies in precipitated immune complexes: a study in 350 Philippine children with acute lower respiratory infection. Scand J infect Dis 31:155–161
Musher DM, Groover JE, Reichler MR et al (1997) Emergence of antibody to capsular polysaccharides of Streptococcus pneumoniae during outbreaks of pneumonia: association with nasopharyngeal colonization. Clin Infect Dis 24:441–446
Musher DM, Groover JE, Watson DA et al (1997) Genetic regulation of the capacity to make immunoglobulin G to pneumococcal capsular polysaccharides. J Investig Med 45:57–68
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Korppi, M., Leinonen, M. & Ruuskanen, O. Pneumococcal serology in children’s respiratory infections. Eur J Clin Microbiol Infect Dis 27, 167–175 (2008). https://doi.org/10.1007/s10096-007-0436-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-007-0436-8