Abstract
The case reported here concerns an alcoholic pork-butcher who presented with severe colitis with peritonitis, caused by the only ciliate protozoan capable of infecting humans, Balantidium coli. This parasite is common in a variety of domestic and wild mammals, mainly pigs; however, its prevalence rate in humans is very low—particularly in industrialised, northern countries, including France. The infection is most frequently acquired by ingesting food or water contaminated by pig faeces, and it may be asymptomatic or may cause acute diarrhoea. Specific antibiotic treatment is efficacious, and it is important to consider the risk of this parasitic disease in susceptible patients presenting with bloody diarrhoea.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In France, the most common parasites isolated from stools are Giardia intestinalis and nonpathogenic amoeba such as Entamoeba coli and Entamoeba hartmanni. Since the onset of the AIDS epidemic, some unusual parasitic organisms, such as Isospora belli, Microsporidia spp. or Cryptosporidium parvum, have emerged in HIV-infected patients [1]. Balantidiasis, an anthropozoonosis due to Balantidium coli, is exceptional as a cause of dysentery in industrialised countries [2], but it may occur in susceptible or immunocompromised individuals; thus, it is important to consider the risk of this parasitic disease in this particular patient population.
Case report
A 54-year-old male patient was admitted to hospital for diarrhoea associated with fever. This patient was a pork-butcher, and had suffered for many years from hypertension and moderate bronchial asthma, without requiring steroids. Four years previously, bilateral aseptic osteonecrosis had led to total bilateral hip arthroplasty. The patient was addicted to alcohol but lived in standard hygienic conditions. Two years prior to presentation, the patient underwent colonoscopy for chronic diarrhoea without loss of weight. The resulting diagnosis was nonspecific congestive colitis. A few days before admission, he experienced acute diarrhoea with fever (38.8°C) and stools containing blood and mucus appeared.
At presentation, the patient was in a weakened state due to severe dehydration (he had lost 8 kg in 1 week). On physical examination, the abdomen was painful and distended, but it remained soft with moderate tenderness, and the intestinal peristalsis was active. Laboratory tests showed severe hypokaliaemia (1.9 mmol/l) and an elevated C-reactive protein level (456 mg/l). Neither hyperleukocytosis nor anaemia was present. Abdominal ultrasound displayed some calcified areas in a heterogeneous liver, whereas liver function tests were normal. Stool examination revealed numerous trophozoites and cysts of B. coli with a large number of neutrophils (Fig. 1).
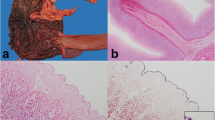
Treatment with doxycycline (200 mg/day) was initiated. After 3 days, the patient experienced sudden, upper-right quadrant abdominal pain and fever associated with pneumoperitoneum. Laparotomy revealed diffuse peritonitis caused by bowel perforation. The right colon was necrotizing dramatically, as to a lesser extent was the transverse colon (Fig. 2). Subtotal colectomy and anastomosis connecting the ileum and the sigmoid flexure were performed. Microscopic examination of the anatomic colon specimen showed parietal necrosis with submucosal B. coli (Fig. 3). After 6 weeks of treatment, the patient completely recovered, and stool examination was negative.
Discussion
B. coli is the largest and only ciliate protozoan that infects humans. Two stages of this parasite can be observed. In the ovoid trophozoite stage, the parasite’s size ranges from 30 to 300 μm in length, and it has a large macronucleus and two contractile vacuoles where food (bacteria, red cells, other parasites, etc.) is digested [3]. Characteristic cilia, observed under phase contrast illumination, enable locomotion and propel food particles into the peristome [4, 5]. The cyst is smaller and can remain viable at room temperature for at least 2 weeks, while mobile trophozoites can only be observed in fresh stool samples. After inoculation, trophozoites penetrate through the epithelium, chiefly from the bottom of crypts. They multiply within the mucosa and submucosa, without always causing necrosis or ulceration. Superficial or deeper ulcers may appear secondarily and lead to haemorrhagic lesions, perforation, and local or generalised peritonitis [4].
Numerous animal species are known to be infected with B. coli, including nonhuman primates, cats, dogs and rats; but pigs are probably the main source of infection in humans [6]. Most of the human cases described thus far involved patients with a history of contact with pigs and poor hygiene conditions [7]. Although B. coli has a worldwide distribution, the incidence in humans is low [8]. This ciliate parasite is exceptional as a cause of dysentery in humans in industrialised countries (including France) [2]. In Denmark, no human cases of balantidiasis have been described, despite a high prevalence of B. coli in pigs in this country [9]. Foci of high incidence have been described and a few outbreaks have been reported from tropical areas [10]. There is little evidence of human-to-human transmission of this infection, although one case was reported in a mental health institution [4].
Balantidiasis can have a variable presentation. In some carriers the infection may be asymptomatic, and when it is detected all carriers should be treated, to avoid dissemination. The acute, bloody and mucoid form of infection may be mild, severe or fulminating with numerous trophozoites in stools [4]. The chronic form presents as intermittent episodes of diarrhoea leading to inconstant excretion of trophozoites and cysts [11]. This protozoan usually affects the large intestine from caecum to rectum. The rectosigmoidal segment is more commonly and more severely affected. Parasite invasion can extend to the appendix and ileum, or it may involve some extradigestive locations such as mesenteric lymph nodes, peritoneum, liver or lung [12].
Many co-factors are involved in the pathogenesis of this disease. The host’s intestinal bacterial flora, the intrinsic virulence of the strain, and the host’s susceptibility are all factors that may influence the development of balantidiasis. Symptomatic infection may be observed in cases of malnutrition, alcoholism, hypochlorhydria, concomitant helminthiasis and immunodeficiency [4]. However, the nature of the relationship between the severity of balantidiasis and HIV infection is unknown. Nonetheless, it should be noted that, while very few cases have been reported in the past decade, four recent publications have described balantidiasis in debilitated, HIV-infected or leukaemic patients [1, 13–15].
Differential diagnoses, such as cryptogenetic disease, bacillary or amoebic dysentery, are generally debated, and association with other infectious agents sometimes occurs. I. belli, Microsporidia spp. or C. parvum are usually isolated from HIV-infected patients. In France, G. intestinalis is the most frequent protozoan isolated from stools (unpublished data). However, its pathogenicity is limited and it never injures the large intestine. Amoebic and balantidial colitis are indistinguishable by clinical signs or macroscopic lesions. The parasitological diagnosis can be established by repeated microscopic examination of fresh stool samples and of tissue scrapings obtained during endoscopy [11].
Antibiotics are used as specific treatment for balantidiasis, and cyclin (100 mg/day) appears to be the drug of choice. Preventive measures are chiefly a matter of maintaining good hygiene [4–6]. When haemorrhagic or severe diarrhoea is observed in a patient working or living in close contact with pigs, B. coli should always be suspected, since early diagnosis and treatment could improve outcome.
References
Cermeno JR, Hernandez De Cuesta I, Uzcategui O, Paez J, Rivera M, Baliachi N (2003) Balantidium coli in an HIV-infected patient with chronic diarrhoea. AIDS 17(6):941–942
Picot S, De Monbrison F (2002) Balantidium coli. Encycl Med Biol VIII–004
Zaman V (1970) Activity of contractile vacuole in the parasitic ciliate, Balantidium coli. Experientia 26:806–807
Arean V, Koppisch E (1956) Balantidiasis. A review and report of cases. Am J Pathol 32:1089–1107
Zaman V (1993) Parasitic protozoa. Academic, London, pp 43–63
Nakauchi K (1999) The prevalence of Balantidium coli infection in fifty-six mammalian species. J Vet Med Sci 61:63–65
Keystone JS, Kozarsky P (2000) Mandell, Douglas and Bennett’s principles and practice of infectious diseases, 5th edn. Churchill Livingstone, Edinburgh, p 2916
Urbina D, Arzuza O, Young G, Parra E, Castro R, Puello M (2003) Rotavirus type A and other enteric pathogens in stool samples from children with acute diarrhea on the Colombian northern coast. Int Microbiol 6:27–3
Hindsbo O, Nielsen CV, Andreassen J, Willingham AL, Bendixen M, Nielsen MA, Nielsen NO (2000) Age-dependent occurrence of the intestinal ciliate Balantidium coli in pigs at a Danish research farm. Acta Vet Scand 41:79–83
Esteban JG, Aguirre C, Angles R, Ash LR, Mas-Comas S (1998) Balantidiasis in Aymara children from the northern Bolivian Altiplano. Am J Trop Med Hyg 59:922–927
Kamberoglou D, Savva S, Adraskelas N, Yannitsiotis A, Cocca E (1990) Balantidiasis complicating a case of ulcerative colitis. Am J Gastroenterol 85:765–766
Vidan JR, Frauca A, Martinez B, Borda F (1885) Hepatic parasitosis caused by Balantidium coli. Med Clin (Barc) 85:299–300
Clyti E, Aznar C, Couppie P, El Guedj M, Carme B, Pradinaud R (1998) A case of coinfection by Balantidium coli and HIV in French Guiana. Bull Soc Pathol Exot 91:309–311
Vasilakopoulos A, Dimarongona K, Samakovli A, Papadimitris K, Avlami A (2003) Balantidium coli pneumonia in an immunocompromised patient. Scand J Infect Dis 35:144–146
Anargyrou K, Petrikkos GL, Suller MTE, Skiada A, Siakantaris MP, Osuntoyinbo RT, Pangalis G, Vaiopoulos G (2003) Pulmonary Balantidium coli infection in a leukemic patient. Am J Hematol 73:180–183
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ferry, T., Bouhour, D., De Monbrison, F. et al. Severe peritonitis due to Balantidium coli acquired in France. Eur J Clin Microbiol Infect Dis 23, 393–395 (2004). https://doi.org/10.1007/s10096-004-1126-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-004-1126-4