Abstract
Introduction
The study aimed to identify the main prognostic factors in diabetic patients with ischemic stroke undergoing reperfusion therapies (RT).
Methods
This retrospective study included 170 diabetic patients: 62 treated with intravenous thrombolysis (IVT) alone and 108 with mechanical thrombectomy (MT). Among MT patients, 29 underwent IVT. We collected clinical, laboratory, and radiological data. The outcomes were 3-month functional impairment (measured by modified Rankin scale, mRs), discharge neurological severity (measured by National Institutes of Health Stroke Scale score, NIHSS), 3-month mortality, intracranial hemorrhage (ICH), and symptomatic intracranial hemorrhage (SICH). We performed a general analysis for all RT and sub-group analyses for IVT and MT.
Results
A lower mRs was associated with lower glycemia and admission NIHSS (aNIHSS) in all RT and MT; lower aNIHSS and younger age in IVT. Mortality increased with hyperglycemia, aNIHSS, and age in all RT; age and aNIHSS in IVT; hyperglycemia and systolic pressure in MT. A lower discharge NIHSS was related with lower aNIHSS, thrombolysis, and no thrombectomy in all RT; lower aNIHSS in IVT; lower aNIHSS and thrombolysis in MT. ICH was associated with elevated aNIHSS, older age, and lower platelets in all RT; lower platelets and older age in IVT; higher aNIHSS in MT. SICH depended on longer thrombectomy duration in all RT; no metformin use in IVT; higher weight in MT.
Conclusion
The study shed light on diabetic patients and stroke RT highlighting the protective effect of metformin in IVT and the role of glycemia, weight, and combined treatment in MT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type 2 diabetes mellitus (T2DM) is a serious public health concern with a considerable impact on human life and health expenditures. About 462 million people suffer from T2DM, corresponding to 6.28% of the world’s population. The USA and Western Europe show a higher prevalence rate that continues to rise despite public health interventions [1]. The number of people living with diabetes mellitus quadrupled between 1980 and 2014 [2]. The global prevalence could increase from 6000 to about 8000 per 100,000 by 2040 [1]. T2DM is a major risk factor for cerebrovascular disease; a diabetic patient has more than doubled risk to develop an ischemic stroke (IS) [3]. Diabetes prevalence in IS was estimated to be 33% [4].
Reperfusion therapies (RT) represent a fundamental treatment in acute IS, and diabetes has a considerable influence on the outcome of treated patients [5,6,7,8]. Although there are many studies that examined the differences between diabetic and no diabetic patients, only a few evaluated factors determining prognosis among diabetic patients with IS and underwent RT.
The aims of the present study are to identify the main prognostic factors in diabetics treated with RT and to evaluate the reciprocal influence of intravenous thrombolysis (IVT) and mechanical thrombectomy (MT) among these patients.
Methods
Patients
In this retrospective study, we reviewed 962 acute IS patients treated with IVT and/or MT in our hospital between February 2014 and December 2019, and we selected 170 patients with a previous T2DM diagnosis.
Patients underwent IVT within 4.5 h after IS onset. In case of unknown symptom onset, the IVT was also performed if magnetic resonance imaging (MRI) showed an ischemic lesion on diffusion-weighted imaging (DWI) that was not visible on fluid-attenuated inversion recovery (FLAIR).
Patients underwent MT within a time frame from symptom onset to treatment ≤ 6 h for anterior circulation and ≤ 24 h for posterior circulation. Regarding stroke with unknown onset, patients were selected using MRI in order to discern between salvageable and terminally infarcted tissue with the application of DWI, perfusion scanning, and FLAIR.
Main exclusion criteria for RT were large territorial infarction defined as Alberta Stroke Program Early CT Score (ASPECTS) < 5, hospital arrival beyond time window, and elevated bleeding risk for IVT.
Patients suffering from type 1 diabetes mellitus were excluded from the study.
Data collection and clinical assessment
The following baseline information and risk factors were assessed in all participants: age, gender, weight, smoke, arterial hypertension, dyslipidemia, coronary heart disease, prior stroke or transitory ischemic attack, chronic kidney disease. Collected data regarding T2DM were antidiabetic drugs (metformin/no metformin) and duration of T2DM. Laboratory test data were admission glucose, creatinine, leucocytes, neutrophils, lymphocytes, and platelets. Admission systolic and diastolic pressures were included. Collected stroke data were etiology according to the Trial of Org 10,172 in Acute Stroke Treatment classification [9], IVT, recombinant tissue plasminogen activator (rtPA) dosage, MT, stroke-to-treatment time (interval between first symptom onset and the beginning of IVT or femoral artery puncture), duration of MT treatment (interval between femoral artery puncture and last contrast bolus injection), neurological severity on admission and discharge using the National Institutes of Health Stroke Scale (NIHSS), intracranial hemorrhage (ICH), symptomatic intracranial hemorrhage (SICH) according to the European-Australian Cooperative Acute Stroke Study 2 (ECASS2) [10], 3-month functional impairment using modified Rankin scale (mRs), and 3-month mortality.
Outcome measures
The main outcome is the mRs at 3 months.
The secondary outcomes are:
-
Neurological severity on discharge
-
3-month mortality
-
ICH
-
SICH
All data were retrospectively obtained using our center database and medical charts. We performed a main analysis on all RT and two subanalyses focusing on patients treated with IVT alone and patients underwent MT, respectively.
Ethics approval and study consent
The research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. The study protocol had been approved by the research institute’s committee on human research. Every patient or a legal representative provided a written informed consent to data collection for scientific purposes.
Statistical analysis
All statistical analyses were performed using R software. Continuous variables were expressed as mean ± standard deviation or median and interquartile range (IQR); categorical variables were expressed as absolute frequencies and percentages. Data were analyzed by Shapiro–Wilk test to evaluate normal distribution. Mann–Whitney U or Student’s t test for independent samples was used for comparison between categorical variables with two levels and continuous variables as appropriate. ANOVA test or Kruskal–Wallis test was used for comparison between categorical variables with more than 2 levels and continuous variables on the basis of normal distribution. The chi-square test was used for comparison between categorical variables. The method of partitioning the degrees of freedom was applied to refuse H0 hypothesis as appropriate. Spearman’s Rank or Pearson’s correlation coefficient was used for comparison between continuous variables as appropriate. In multivariate analyses (MA), we used binomial logistic regression model or multiple linear regression model. A binomial logistic regression was used for binary-dependent variables (3-month mortality, ICH and SICH) whereas a multiple linear regression was used for quantitative outcomes (mRs at 3 months and neurological severity on discharge). The goodness of fit tests used were Hosmer–Lemeshow for C and H statistic, Osius-Rojek’s, Stukel’s, and Le Cessie-Van Houwelingen-Copas-Hosmer [11]. A value of P ≤ 0.05 was considered significant.
Results
Descriptive analysis
The study cohort comprised 170 diabetic patients. The mean age was 76.72 years, eighty-four (49.4%) were males, and the median admission NIHSS was 14 (IQR 8–18). The median functional outcome at 3 months measured by mRs was 4 (IQR 2–6). The median discharge NIHSS was 5 (IQR 2–10). Forty-six patients (27.1%) died within 3 months. Fifty-nine patients (34.7%) had an ICH, and fifteen (8.8%) a SICH.
Patients who underwent IVT alone were 62. The mean age was 76.89 years, thirty-three (53.2%) were males, and the median admission NIHSS was 10 (IQR 6–15). The mRs at 3 months was 3 (IQR 1–5). The median discharge NIHSS was 3 (IQR 1–5). Fourteen patients (24.6%) died within 3 months. Twenty-two patients (35.5%) had an ICH, and seven (11.5%) a SICH.
MT was performed in 108 patients. Among these, only 29 patients underwent IVT, whereas the others were not treated in most cases because of delay in hospital arrival and the unknown onset with a no permissive MRI. They had a mean age of 76.62 years, the males were 51 (47.2%), and the median admission NIHSS was 14 (IQR 10.75–18.25). The mRs at 3 months was 4 (IQR 2–6). The median discharge NIHSS was 6 (IQR 3–12). Thirty-two patients (29.6%) died within 3 months; thirty-seven patients (34.3%) had an ICH, and eight (7.4%) a SICH.
The present data, remaining baseline characteristics, and treatment information are summarized in Table 1. Table S1 shows a descriptive analysis of MT patients divided according to treatment with IVT.
Outcome analysis in all patients undergoing reperfusion therapies
A higher 3-month mRs was associated with no metformin use (4 [2–6] vs 3 [1–5]; p-value = 0.020), MT (4 [2–6] vs 3 [1–5]; p-value = 0.034), older age (correlation coefficient, r = 0.211; p-value = 0.009), higher admission blood glucose (r = 0.202; p-value = 0.013), and elevated admission NIHSS (r = 0.407; p-value = 0.000) (see Table 2). Only admission blood glucose and admission NIHSS maintained statistical significance on MA.
Lower NIHSS on discharge was associated with IVT (5.11 ± 5.50 vs 8.63 ± 6.11; p-value = 0.001), no MT (5.19 ± 5.62 vs 7.71 ± 6.10; p-value = 0.013), lower neutrophil levels (r = 0.200; p-value = 0.018), higher lymphocyte levels (r = − 0.199; p-value = 0.018), and lower admission NIHSS (r = 0.521; p-value = 0.000) (see Table 3). On MA, lower NIHSS on discharge was related only with IVT, no MT, and admission NIHSS.
The 3-month mortality was associated with older age (78.98 ± 8.31 vs 75.41 ± 8.87; p-value = 0.021), no smoke (32.0% vs 12.5%; p-value = 0.053), elevated admission blood glucose (210.00 ± 81.84 vs 175.67 ± 60.98; p-value = 0.005), and a higher admission NIHSS (17.5 [11–20] vs 13 [8–17]; p-value = 0.003) (see Table S2). Age, blood glucose, and admission NIHSS were related with mortality on MA.
Patients with ICH were older (78.97 ± 7.90 vs 75.61 ± 8.93; p-value = 0.017) and more frequently non-smoker (38.3% vs 16%; p-value < 0.031) and they had lower platelet levels (210,574.55 ± 203,000.00 vs 251,046.73 ± 102,239.28; p-value = 0.008) and a higher admission NIHSS (16 [13–19.5] vs 12 [8–17]; p-value = 0.001) (see Table 4). MA confirmed age, platelets, and admission NIHSS.
The predictors of SICH were leucocyte levels (7807.86 ± 2981.04 vs 9405.96 ± 2828.66; p-value = 0.046), stroke etiology (2.6% of large artery atherosclerosis, 15.5% of cardio embolism, 33.3% of small vessel occlusion, 6.0% of undetermined subtype; p-value < 0.051), and duration of MT treatment (151.25 ± 105.11 vs 75.55 ± 38.87; p-value = 0.001) (see Table 5). Only MT duration was confirmed on MA.
Outcome analysis in patients undergoing IVT
Analyzing patients undergoing IVT, a lower 3-month mRs was associated metformin (2 [0–4] vs 4 [3–6]; p-value = 0.004), younger age (r = 0.562; p-value = 0.000), short diabetes duration (r = 0.328; p-value = 0.013), and lower admission NIHSS (r = 0.538; p-value = 0.000) (see Table 2). Age and admission NIHSS were also confirmed on MA.
A lower NIHSS on discharge was related with younger age (r = 0.332; p-value = 0.012); metformin use (2 [1–4.75] vs 5.5 [1–12]; p-value = 0.031); lower neutrophil levels (r = 0.330; p-value = 0.013); higher lymphocyte levels (r = − 0.319; p-value = 0.016); lower admission NIHSS (r = 0.502; − value = 0,000) (see Table 3). MA confirmed only admission NIHSS.
The 3-month mortality was associated with older age (84.71 ± 3.93 vs 74.49 ± 9.82; p-value = 0.001), female sex (37.5% vs 15.2%; p-value < 0.053), longer diabetes duration (21.14 ± 10.13 vs 14.27 ± 9.53; p-value = 0.025), no metformin use (40.0% vs 10.7%; p-value < 0.013), higher admission NIHSS (16.5 [8.25–20] vs 8 [5.5–15]; p-value = 0.004) (see Table S2). MA identified older age and higher admission NIHSS as the mortality main predictors.
The ICH was associated with older age (80.73 ± 7.23 vs 74.78 ± 10.11; p-value = 0.018), no metformin use (52.0% vs 20.0%; p-value < 0.013), higher admission systolic pressure (169.10 ± 32.57 vs 154.03 ± 21.00; p-value = 0.032), lower platelet levels (210,714.29 ± 44,976.82 vs 277,375.00 ± 127,498.96; p-value = 0.024), stroke etiology (7.1% of large artery atherosclerosis, 60% of cardio embolism, 33.3% of small vessel occlusion, and 36.7% of undetermined subtype; p-value < 0.031), unknown onset time (18.2% vs 2.5%; p-value = 0.033) (see Table 4). Only age and platelets remained significant on MA.
The only predictor of SICH was metformin use (0.0% vs 20.8%; p-value < 0.009) (see Table 5).
Outcome analysis in patients undergoing MT
Analyzing patients undergoing MT, the 3-month mRs score was associated with admission blood glucose (r = 0.297; p-value = 0.004) and admission NIHSS (r = 0.267; p-value = 0.008) (see Table 2). This significance persisted on MA.
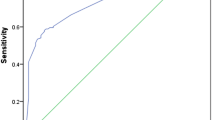
The discharge NIHSS was associated with IVT (3.5 [1.25–5] vs 7 [4–13]; p-value = 0.004; see Fig. 1) and admission NIHSS (r = 0.437; p-value = 0.000) (see Table 3). MA confirmed these associations.
The 3-month mortality was also linked with admission systolic pressure (160.34 ± 24.91 vs 148.20 ± 25.05; p-value = 0.027) and admission glucose levels (215.94 ± 92.34 vs 171.86 ± 63.83; p-value = 0.008) (see Table S2). MA confirmed these associations.
The ICH was related only with higher NIHSS (17 [14–20] vs 13 [9–18]; p-value = 0.001) (see Table 4).
The predictors of SICH were elevated weight (89.25 ± 11.06 vs 74.06 ± 10.73; p-value = 0.008), rtPA dosage (73.33 ± 14.74 vs 56.54 ± 11.18; p-value = 0.024), and prolonged MT duration (151.25 ± 105.11 vs 75.55 ± 38.87; p-value = 0.001) (see Table 5). MA identified only weight as SICH-independent predictor.
Discussion
Although T2DM is present in one-third of IS, only few studies had evaluated factors determining prognosis among diabetic patients with IS and undergoing RT.
Regarding functional outcome and mortality, we observed an association with admission glycemia in all patients and MT patients but not in the IVT-alone group. Patients undergoing MT, therefore, are probably more influenced by hyperglycemia than IVT patients and this should be considered. In our patients treated only with IVT, mRs score increased according to the glycemia levels but this trend was not significant: hyperglycemia had an influence on functional outcome but it was not a main outcome predictor. Literature data are conflicting about glycemia and functional outcome in diabetics. In IVT patients, two studies did not find an association [12, 13] whereas other three observed it [14,15,16]. In MT patients, two studies correlated hyperglycemia with a worst functional outcome [17, 18] whereas other two failed to find it [7, 19]. These discrepant responses to hyperglycemia could be due to the difference in chronic glycemic control, diabetic drugs taken, diabetes duration, and other metabolic conditions: further studies should investigate these elements. Another important element of our analysis is that mortality in MT patients was linked to high levels of systolic pressure on the admission. No other studies in literature evaluated pressure influence in diabetic patients treated with MT. A high systolic pressure was associated with a worse functional outcome in general patients undergoing MT in several studies which explained it through reperfusion injury, cerebral edema, and hemorrhagic transformation [20]. Another hypothesis is that hypertension may be a sign of stroke severity rather than a determinant: the organisms increase blood pressure in order to maintain cerebral perfusion [20]. It is interesting to observe that blood pressure was not related with discharge neurological severity, hemorrhagic transformation, and functional outcome in our patients: we could also hypothesize that the higher mortality was due to a more severe T2DM rather than stroke damage in itself. T2DM was associated with artery stiffness, autonomic dysfunction, endothelium dysfunction, and impaired nitric oxide (NO) synthesis [21] that can favor an alteration of blood pressure control. IS could be considered a stress test that could induce higher pressure peaks in patients with a more severe neurovascular dysfunction due to T2DM. Conditions such as autonomic dysfunction were indeed associated with an increased mortality in T2DM [22, 23].
Regarding neurological severity on discharge, in all RT group, we observed that MT was associated with higher NIHSS, whereas IVT with lower score probably because most of IVT patients had no large vessel occlusion. It is important to highlight that IVT in patients undergoing MT led to a reduced (almost halved) neurological severity, supporting (with the limits of our small population size) the efficacy of combined treatment in these patients.
Evaluating ICH, platelet levels and age appeared as the main predictors in all RT group and IVT patients which did not influence bleedings in MT. Our study also showed that duration of MT was associated with SICH in all RT but not in MT. We could explain this result as an increased SICH risk in patients undergoing longer MT compared with patients treated only with IVT. In patients undergoing MT, the high weight was the only predictor of SICH. This association was not evaluated in other MT study on T2DM. Regarding hemorrhagic transformation and obesity in general population treated with MT, some studies described no association [24,25,26], whereas Chen et al. reported a reduction in symptomatic hemorrhage [27]. Another study found no relationship between SICH and metabolic syndrome [28]. In our patients, the combination between T2DM and high weight probably favored an increased vessel fragility that could not be present in obesity alone and in metabolic syndrome, condition in which patients are not always diabetics.
We furthermore found that metformin had a protective role for SICH in IVT patients. Several preclinical study [29,30,31,32,33] and three clinical study showed the positive impact of metformin in ischemic stroke [34,35,36]. Indeed, metformin plays an anti-oxidant and anti-inflammatory action, favoring the blood–brain barrier integrity and a correct endothelial function [37]. The metformin beneficial effect was not observed in our MT patients, a larger population study is probably necessary in order to find it.
There are several limitations in our study. The small number of patients may have underpowered our analysis. The study in a single institution may have affected the selection of patients but it allowed us to obtain data homogeneity. The retrospective design represents another limit. The glycated hemoglobin would have been a useful data but it was missing in a significant part of patients.
Conclusion
The present study evaluated RT in patients affected by T2DM that constitutes one-third of IS victims and deserve attention in regard to their complexity and fragility. We observed a prognostic role of admission glycemia in MT but not in IVT. The study showed that neurological severity on discharge was reduced in patients undergoing both treatments compared with MT alone. A protective role of metformin for SICH was found in patients treated with IVT, whereas the high weight was a predictor of symptomatic hemorrhage in MT. Our results give several insights in regard to T2DM and stroke RT that need to be confirmed in larger studies, but they represent a starting point in order to ameliorate medical management of these patients.
Data availability
Derived data supporting the findings of this study are available from the corresponding author on request.
References
Khan MAB, Hashim MJ, King JK et al (2020) Epidemiology of type 2 diabetes - global burden of disease and forecasted trends. J Epidemiol Glob Health 10:107–111. https://doi.org/10.2991/JEGH.K.191028.001
Zheng Y, Ley SH, Hu FB (2018) Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol 14:88–98. https://doi.org/10.1038/nrendo.2017.151
Chen R, Ovbiagele B, Feng W (2016) Diabetes and stroke: epidemiology, pathophysiology, pharmaceuticals and outcomes. Am J Med Sci 351:380–386. https://doi.org/10.1016/j.amjms.2016.01.011
Lau L, Lew J, Borschmann K et al (2019) Prevalence of diabetes and its effects on stroke outcomes: a meta-analysis and literature review. J Diabetes Investig 10:780–792. https://doi.org/10.1111/jdi.12932
Desilles JP, Meseguer E, Labreuche J et al (2013) Diabetes mellitus, admission glucose, and outcomes after stroke thrombolysis: a registry and systematic review. Stroke 44:1915–1923. https://doi.org/10.1161/STROKEAHA.111.000813
Girot J-B, Richard S, Gariel F et al (2020) Predictors of unexplained early neurological deterioration after endovascular treatment for acute ischemic stroke. Stroke 51:2943–2950. https://doi.org/10.1161/STROKEAHA.120.029494
Šaňák D, Černík D, Divišová P et al (2020) Low levels of glycemia within the first 48 hours after mechanical thrombectomy for acute ischemic stroke may be associated with better clinical outcome. J Stroke Cerebrovasc Dis 29:1–8. https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.104621
Zhang YH, Shi MC, Wang ZX et al (2021) Factors associated with poor outcomes in patients undergoing endovascular therapy for acute ischemic stroke due to large-vessel occlusion in acute anterior circulation: a retrospective study. World Neurosurg 149:e128–e134. https://doi.org/10.1016/j.wneu.2021.02.064
Adams HP, Bendixen BH, Kappelle LJ et al (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24:35–41. https://doi.org/10.1161/01.STR.24.1.35
Hacke W, Kaste M, Fieschi C et al (1998) Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Lancet 352:1245–1251. https://doi.org/10.1016/S0140-6736(98)08020-9
Hosmer DW, Hosmer T, Cessie SLE, Lemeshow S (1997) A comparison of goodness-of-fit tests for the logistic regression model. Stat Med 16:965–980. https://doi.org/10.1002/(SICI)1097-0258(19970515)16:9%3c965::AID-SIM509%3e3.0.CO;2-O
Choi KH, Park MS, Kim JT et al (2016) Lipoic acid use and functional outcomes after thrombolysis in patients with acute ischemic stroke and diabetes. PLoS ONE 11:1–12. https://doi.org/10.1371/journal.pone.0163484
Fang HJ, Pan YS, Wang YJ et al (2020) Prognostic value of admission hyperglycemia on outcomes of thrombolysis in ischemic stroke patients with or without diabetes. Chin Med J (Engl) 133:2244–2246. https://doi.org/10.1097/CM9.0000000000001005
Masrur S, Cox M, Bhatt DL et al (2015) Association of acute and chronic hyperglycemia with acute ischemic stroke outcomes post-thrombolysis: findings from get with the guidelines-stroke. J Am Heart Assoc 4:1–13. https://doi.org/10.1161/JAHA.115.002193
Poppe AY, Majumdar SR, Jeerakathil T et al (2009) Admission hyperglycemia predicts a worse outcome in stroke patients treated with intravenous thrombolysis. Diabetes Care 32:617–622. https://doi.org/10.2337/dc08-1754
Tsivgoulis G, Katsanos AH, Mavridis D et al (2019) Association of baseline hyperglycemia with outcomes of patients with and without diabetes with acute ischemic stroke treated with intravenous thrombolysis: a propensity score-matched analysis from the SITS-ISTR registry. Diabetes 68:1861–1869. https://doi.org/10.2337/db19-0440
Natarajan SK, Dandona P, Karmon Y et al (2011) Prediction of adverse outcomes by blood glucose level after endovascular therapy for acute ischemic stroke. J Neurosurg 114:1785–1799. https://doi.org/10.3171/2011.1.JNS10884
Borggrefe J, Glück B, Maus V et al (2018) Clinical outcome after mechanical thrombectomy in patients with diabetes with major ischemic stroke of the anterior circulation. World Neurosurg 120:e212–e220. https://doi.org/10.1016/j.wneu.2018.08.032
Wnuk M, Popiela T, Drabik L et al (2020) Fasting hyperglycemia and long-term outcome in patients with acute ischemic stroke treated with mechanical thrombectomy. J Stroke Cerebrovasc Dis 29:104774. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.104774
Vitt JR, Trillanes M, Hemphill JC (2019) Management of blood pressure during and after recanalization therapy for acute ischemic stroke. Front Neurol 10:1–13. https://doi.org/10.3389/fneur.2019.00138
Goligorsky MS (2017) Vascular endothelium in diabetes. Am J Physiol - Ren Physiol 312:F266–F275. https://doi.org/10.1152/ajprenal.00473.2016
Freeman R (2014) Diabetic autonomic neuropathy. In: Handbook of clinical neurology, 1st ed. Elsevier B.V., pp 63–79
Vinik AI, Maser RE, Mitchell BD, Freeman R (2003) Diabetic autonomic neuropathy. Diabetes Care 26:1553–1579. https://doi.org/10.2337/diacare.26.5.1553
Hallan DR (2021) Obesity and mechanical thrombectomy. Cureus 13:1–9. https://doi.org/10.7759/cureus.12671
Pirson FAV, Hinsenveld WH, Staals J et al (2019) The effect of body mass index on outcome after endovascular treatment in acute ischemic stroke patients: a post hoc analysis of the MR CLEAN Trial. Cerebrovasc Dis 48:200–206. https://doi.org/10.1159/000504744
Bouslama M, Perez HJ, Barreira CM et al (2020) Body mass index and clinical outcomes in large vessel occlusion acute ischemic stroke after endovascular therapy. Interv Neurol 8:144–151. https://doi.org/10.1159/000496703
Chen SH, McCarthy D, Saini V et al (2020) Effect of body mass index on outcomes of mechanical thrombectomy in acute ischemic stroke. World Neurosurg 143:e503–e515. https://doi.org/10.1016/j.wneu.2020.07.220
Chen Z, Su M, Li Z et al (2020) Metabolic syndrome predicts poor outcome in acute ischemic stroke patients after endovascular thrombectomy. Neuropsychiatr Dis Treat 16:2045–2052. https://doi.org/10.2147/NDT.S264300
Li J, Benashski SE, Venna VR, McCullough LD (2010) Effects of metformin in experimental stroke. Stroke 41:2645–2652. https://doi.org/10.1161/STROKEAHA.110.589697
Venna VR, Li J, Hammond MD et al (2014) Chronic metformin treatment improves post-stroke angiogenesis and recovery after experimental stroke. Eur J Neurosci 39:2129–2138. https://doi.org/10.1111/ejn.12556
Jiang T, Yu JT, Zhu XC et al (2014) Acute metformin preconditioning confers neuroprotection against focal cerebral ischaemia by pre-activation of AMPK-dependent autophagy. Br J Pharmacol 171:3146–3157. https://doi.org/10.1111/bph.12655
Deng T, Zheng YR, Hou WW et al (2016) Pre-stroke metformin treatment is neuroprotective involving AMPK reduction. Neurochem Res 41:2719–2727. https://doi.org/10.1007/s11064-016-1988-8
Harada S, Fujita-Hamabe W, Tokuyama S (2010) The importance of regulation of blood glucose levels through activation of peripheral 5′-AMP-activated protein kinase on ischemic neuronal damage. Brain Res 1351:254–263. https://doi.org/10.1016/j.brainres.2010.06.052
Mima Y, Kuwashiro T, Yasaka M et al (2016) Impact of metformin on the severity and outcomes of acute ischemic stroke in patients with type 2 diabetes mellitus. J Stroke Cerebrovasc Dis 25:436–446. https://doi.org/10.1016/j.jstrokecerebrovasdis.2015.10.016
Westphal LP, Widmer R, Held U et al (2020) Association of pre-stroke metformin use, stroke severity, and thrombolysis outcome. Neurol. https://doi.org/10.1212/WNL.0000000000009951
Favilla CG, Mullen MT, Ali M et al (2011) Sulfonylurea use before stroke does not influence outcome. Stroke 42:710–715. https://doi.org/10.1161/STROKEAHA.110.599274
Sharma S, Nozohouri S, Vaidya B, Abbruscato T (2021) Repurposing metformin to treat age-related neurodegenerative disorders and ischemic stroke. Life Sci 274:119343. https://doi.org/10.1016/j.lfs.2021.119343
Acknowledgements
We would like to thank L.R., C.A., and C.M.L. for the strong support in these years; F.F. for the opportunity; A.G., M.A., and R.S. for the long and strong partnership; N.G., Z.V., and C.A. for the partnership and the support in these unforgettable years; C.A. also for the method, the advices, the spark, and the research interest in common; F.I., V.C., and G.F. for the partnership, the advices, and for being an example; C.D., D.J., G.A., and F.G. for the partnership and their limitless kindness; C.M. for believing in us from the beginning; D.C. for being a wonderful person; M.R. for the motivation; and all members of our neurology department in particular the physicians in training.
Author information
Authors and Affiliations
Contributions
C.C.T. contributed to the study design; C.C.T., C.M., P.A., L.M., V.S.L., F.M.C., G.F., and D.C. performed the data collection; T.G. performed the statistical analysis; C.M., G.R., L.P., C.C., T.A., L.M., G.F., and M.R.F. supervised the research; C.C.T., F.G., M.R.F., and R.G. wrote the article.
Corresponding author
Ethics declarations
Ethical approval
The research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. The study protocol has been approved by the research institute’s committee on human research.
Consent to participate and for publication
All the patients have given their written informed consent.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Currò, C.T., Fiume, G., Cotroneo, M. et al. Ischemic stroke and reperfusion therapies in diabetic patients. Neurol Sci 43, 4335–4348 (2022). https://doi.org/10.1007/s10072-022-05935-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-022-05935-x