Abstract
Isolated cerebrospinal fluid hypertension (ICH) is a condition of increased cerebrospinal fluid (CSF) pressure in the cranial-spinal compartment without an identifiable cause. Isolated headache is the most common symptom of ICH, while missing may be signs such as papilledema or sixth nerve palsy. This fact makes difficult the clinical diagnosis of headache attributable to ICH in headache sufferers. Another source of confusion stems from the CSF pressure measurement. It has been observed that a single-spot CSF opening pressure measurement may be insufficient to identify elevated CSF pressure in headache sufferers. A new method of CSF pressure measurement has been able to identify pressure-related features of isolated CSF hypertension (ICH). In fact, nocturnal or postural headache and abnormal pressure pulsations are the more common pressure-related features of ICH in patients with chronic headache. The compressive action of these abnormal pressure pulsations causes the periventricular white matter microstructure alterations leading to the focal diffusion tensor imaging findings in patients with ICH. Abnormal pressure pulsations are a marker of ICH in chronic headache. The identification of the CSF pressure-related features may be useful for differentiating headache sufferers with ICH from those with primary headache disorder in clinical practice. The therapeutic strategy in these headache sufferers with ICH includes the CSF removal and a medical treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The term isolated cerebrospinal fluid (CSF) hypertension indicates the occurrence of CSF pressure elevation in the cranial-spinal compartment without an identifiable cause [1]. For the reason that altered CSF pressure is investigated by using a novel method of lumbar CSF pressure monitoring, and the pressure parameters evaluated for diagnosing increased CSF pressure are not included in the ICHD-3 diagnostic criteria of idiopathic intracranial hypertension [2], we used to name isolated CSF hypertension (ICH) a condition of increased CSF pressure in the cranial-spinal compartment in the place of idiopathic intracranial hypertension.
The clinical manifestations of ICH are headache, visual disturbances, tinnitus, vertigo, and intracranial noises, while signs such as papilledema and sixth nerve palsy may be also lacking in patients with elevated CSF pressure [3, 4]. Isolated headache is the more common clinical manifestation of ICH [5, 6]. In such cases, recognition of headache due to ICH is difficult and subject to much debate in everyday practice. Indeed, the recognized headache profile of patients with ICH does not differ from that of patients with primary headache disorder [7]. This fact indicates the need to identify the clinical characteristics and the CSF pressure-related features of ICH in headache sufferers.
The recent introduction of the new method of lumbar CSF pressure measurement enabled us to detect the characteristics and the pressure-related features of ICH, in order to differentiate headache sufferers with headache attributable to ICH from those with primary headache disorder [8].
Diagnostic innovations
CSF pressure measurement
In clinical practice, the diagnosis of high CSF pressure relies on the single-spot measurement of CSF opening pressure. Latterly, a growing body of evidence [1, 8,9,10] highlighted that CSF pressure measurement by using the height of the fluid column in the manometer line connected to a spinal puncture needle may be misleading in headache sufferers. Hence, in everyday practice, it may be an error in excluding the recognition of ICH in headache sufferers on the basis of a single-spot opening pressure measurement.
Recently, some studies demonstrated the accuracy of 1-h lumbar CSF pressure monitoring through a spinal puncture needle in estimating CSF pressure. Some authors reported that a single-spot of opening pressure measurement was less accurate than 1-h CSF pressure monitoring in detecting high CSF pressure in headache sufferers suspected of having ICH [8]. Others demonstrated that 1-h lumbar CSF pressure monitoring through a spinal puncture needle is a safe method of pressure measurement, and also found that 60 min of pressure recording is sufficient to detect altered CSF pressure in headache sufferers suspected of having ICH in the absence of papilledema or sixth nerve palsy [1].
One-hour lumbar CSF pressure monitoring through a spinal puncture needle has also been described elsewhere [8]. To improve the compliance of the patients during the lumbar CSF pressure monitoring, a local anesthesia and a mild sedation is necessary before LP. This avoided confounding factors such as pain and anxiety of the patients, and pressure artifacts during continuous pressure recording. In short, in a puncture room with the subject in the left lateral decubitus position, a standard 20-gauge (occasionally 22-gauge) Quincke pointed spinal needle with a three-way stopcock was inserted. The pressure transducer (Transducer kit, Edwards Lifesciences, Irvine, CA, USA) was attached to the hub of needle via a 10-cm-long flexible tube without loss of CSF and placed at the level of the same horizontal plane as the estimated level of the spinal puncture needle in the subarachnoid space; it was then zeroed. A pressure cable linked the transducer to the monitor (Passport V, Datascope Corporation, Mahwah, NJ, USA). At the beginning, opening pressure was recorded for 4 min to be certain that the pressure values had stabilized. Immediately after, CSF pressure was also monitored for a 60-min period to analyze the mean pressure, highest peak pressure, mean pulse amplitude, and abnormal fluctuations in pressure. Physician observation was continuous in order to analyze CSF pressure only during artifact-free epochs.
This technique of continuous recording of lumbar CSF pressure found that headache sufferers without papilledema or sixth nerve palsy but with a normal or slightly elevated CSF opening pressure during a single-spot CSF pressure measurement may manifest high-mean CSF pressure and abnormal pressure pulsations in form of B waves [1, 8,9,10], identified as repetitive pulsations in CSF pressure occurring one to six times per minute in periods of more than 10 min with pressure elevations from 65 mm H2O to 680 mm H2O [11]. Small pulsations in CSF pressure synchronous with respiration (ranging 10–30 mm CSF) and with systole (ranging 20–30 mm CSF) were observed in normal subjects [10]. The pathogenesis of these abnormal CSF pressure pulsations may be explained taking into consideration the theory that CSF pressure is derived from the circulation of cerebral blood and cerebrospinal fluid [12]. In fact, the disruption of the autoregulation of cerebral blood flow and poor compliance of cerebrospinal system may be both pathophysiological mechanisms causing the abnormal CSF homeostasis which in turn lead to abnormal pressure pulsations and high CSF pressure [13].It is worth noting, the majority of headache sufferers with ICH have bilateral transverse sinus stenosis that causes cerebral venous flow abnormalities. While a reduced compliance of the spinal canal compartment causing a delayed CSF absorption [14] can contribute to the development of high CSF pressure with abnormal pressure pulsations in headache who have no transverse sinus stenosis. Abnormal pressure waves (B waves) are associated with rhythmic alterations of cerebral blood flow [15]. On this basis, the presence of the abnormal CSF pressure pulsations, indicating a failure of the compensatory mechanisms for maintaining a normal CSF pressure, signifies that CSF pressure elevation is symptomatic. Abnormal CSF pressure pulsations, hence, may be considered a marker of high CSF pressure.
Neuroimaging study
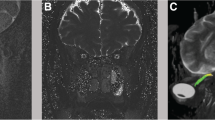
It has recently been recognized that brain MRI and cerebral MR venography are useful tools for detecting periorbital and intracranial findings and cerebral venous outflow abnormalities associated with elevated CSF pressure. Typical periorbital and intracranial MRI findings in patients with ICH include distension of the perioptic subarachnoid space, flattening of the posterior aspect of the globe, optic nerve protrusion, and empty sella turcica [16, 17]. 3D phase contrast cerebral MR venography with a velocity of encoding set to 15 cm/s is the most valuable non-invasive way for detecting venous flow disturbances associated with ICH [18]. Moreover, sinovenous stenosis is more common in patients with ICH than in subjects with normal CSF pressure [19, 20]. By contrast, few of headache patients with abnormal CSF pressure pulsations and high CSF pressure have normal appearance of TS or unilateral TSS [1].
Transverse sinus (TS) stenosis (TSS) is considered present when the signal flow was poor or lacking (flow gap) in the mid-lateral portion of the transverse sinus (unilateral TSS) or in both transverse sinuses (BTSS). It has been observed that BTSS, identified through cerebral MR venography, is associated with ICH in headache sufferers who had migraine or chronic tension-type headache as an isolated neurological symptom [5, 6].
Diffusion tensor imaging (DTI) is a non-invasive method based on the diffusion characteristics of water which recognizes the random motion of water molecules and where it is restricted by biological barriers, and is one of the most sensitive and promising MRI-based diagnostic tools for detecting subtle microstructural cerebral WM changes. A more recent study [21] found a significant DTI alteration in periventricular WM microstructure of patients with ICH suggesting tissue compaction correlated with the compressive action of the abnormal CSF pressure pulsations. This periventricular WM change may be partially reversible after medical treatment. These findings for the first time provide evidence that ICH, as well as high blood pressure, causes target organ damage.
Clinical implications
Characteristics and CSF pressure-related features of ICH
Diagnostic innovations such as 1-h lumbar CSF pressure monitoring via a spinal puncture needle enable us to detect the characteristics and the CSF pressure-related features of ICH.
Nocturnal and postural headache, and abnormal CSF pressure pulsations are the most common pressure-related features of ICH in patients with chronic headache. Abnormal pressure pulsations may be considered a marker of ICH in patients with chronic headache who have no evidence of papilledema or sixth nerve palsy. Their presence, hence, differentiates headache sufferers with ICH from those with primary headache disorder [1].
There is indeed an important difference in clinical manifestations of patients with ICH. The more severe symptoms such as nocturnal attacks of pulsating pain and postural headache, vertigo, headache aggravated with coughing, or pulsatile tinnitus were more common in patients with ICH who have the most abnormal CSF pressure pulsations. Nocturnal attacks of pulsating pain and postural headache are more common in patients with ICH. The abnormal pulsations in CSF pressure occurring during sleep may be the cause of nocturnal headache, while rapid pulsations in CSF pressure precipitated by posture changes may trigger the positional headache [22]. These observations indicate that clinical manifestations are related to the presence and severity of abnormal pressure pulsations in headache sufferers with ICH.
One possible basis for headache in these patients with ICH, thus, could be a sensitization of the intracranial meninges due to mechanical stimuli of recurrent abnormal CSF pressure pulsations. This sensitization of meningeal afferents to mechanical stimuli is recognized to be the mechanism causing pulsating head pain aggravated by sudden head movements and coughing in patients with intracranial pathologies [23]. The latter mechanism produces the peripheral sensitization leading to central sensitization, which in turn may contribute to the chronification of headache in these patients. It is worth noting that most patients with ICH had a chronic headache mimicking the pre-existing primary headache. A possible explanation of the presence of a primary headache mimic in these patients is that abnormal pulsations in CSF pressure may trigger the same mechanism that causes the pain in primary headache attack. Hence, the primary headache mimic can also be a variation of pre-existing primary headache; thus, it could be considered neither secondary nor primary but triggered headache [1].
Diagnostic criteria of ICH
ICH was diagnosed if the patient met the following diagnostic criteria: (i) at least two or more of the following symptoms of raised CSF pressure: postural or nocturnal headaches, headache aggravated with coughing or worse on awakening, transient visual obscurations, photopsias, vertigo, pulsatile tinnitus, and intracranial noises; (ii) at least two or more of the following neuroimaging signs: bilateral transverse sinus stenosis, empty sella, posterior sclera flattening, perioptic subaracnoid space distension, vertical tortuosity of the orbital optic nerve, and tonsillar ectopia; (iii) altered pressure parameters for stage 1 or stage 2 of CSF hypertension (Table 1); (iv) normal CSF contents; (v) symptoms were relieved by reducing CSF hypertension.
Therapeutic strategy
The therapeutic strategy in these headache sufferers with ICH includes the CSF removal which induces an improvement of headache intensity and frequency in all of the patients with ICH, an informal weight reduction diet program in all obese patients, and the administration of acetazolamide and topiramate simultaneously.
Conclusions
The new findings, demonstrating that the presence and the severity of abnormal pressure pulsations are related to clinical manifestations of ICH in patients with chronic headache, highlight that CSF pressure is a continuous, not discrete, variable. Thus, lumbar CSF pressure monitoring via a spinal puncture needle for 1 h may be needed for detecting high CSF pressure in patients with chronic headache who have no papilledema and sixth nerve palsy. In clinical practice, the diagnostic innovations may be useful for avoiding that patients with ICH experienced a considerable delay in their diagnosis and treatment.
References
Bono F, Curcio M, Rapisarda L et al (2018) Cerebrospinal fluid pressure-related features in chronic headache: a prospective study and potential diagnostic implications. Front Neurol 18(9):1090. https://doi.org/10.3389/fneur.2018.01090 eCollection 2018
(2018) The International Classification of Headache Disorders, 3rd edition. Cephalalgia 38(1):1–211
Lipton HL, Michelson PE (1972) Pseudotumor cerebri without optic papilledema. JAMA 220:1591–1592
Marcelis J, Silberstein SD (1991) Idiopathic intracranial hypertension without papilledema. Arch Neurol 48:392–399
Bono F, Messina D, Giliberto C, Cristiano D, Broussard G, Fera F, Condino F, Lavano A, Quattrone A (2006) Bilateral transverse sinus stenosis predicts IIH without papilledema in patients with migraine. Neurology 67:419–423
Bono F, Messina D, Giliberto C, Cristiano D, Broussard G, D’Asero S, Condino F, Mangone L, Mastrandrea C, Fera F, Quattrone A (2008) Bilateral transverse sinus stenosis and idiopathic intracranial hypertension without papilledema in chronic tension-type headache. J Neurol 255:807–812
Bono F, Quattrone A (2009) Idiopathic intracranial hypertension without papilledema in headache sufferers. Cephalalgia 29:593–594
Bono F, Salvino D, Tallarico T, Cristiano D, Condino F, Fera F, Lanza PL, Lavano A, Quattrone A (2010) Abnormal pressure waves in headache sufferers with bilateral transverse sinus stenosis. Cephalalgia 30(12):1419–1425
Spence JD, Amacher LA, Willis NR (1980) Benign intracranial hypertension without papilledema: role of 24-hour cerebrospinal fluid pressure monitoring in diagnosis and management. Neurosurgery 7:326–336
Torbey MT, Geocadin RG, Razumovsky AY, Rigamonti D, Williams MA (2004) Utility of CSF pressure monitoring to identify idiopathic intracranial hypertension without papilledema in patients with chronic daily headache. Cephalalgia 24(6):495–502
Lundberg N (1960) Continuous recording and control of ventricular fluid pressure in neurosurgical practice. Acta Psychiatr Neurol Scand 149(suppl):1–193
Fishman RA (1992) Cerebrospinal fluid in diseases of the nervous system, 2nd edn. W.B. Saunders Company, Philadelphia, pp 71–101
Czosnyka M, Pickard JD (2004) Monitoring and interpretation of intracranial pressure. J Neurol Neurosurg Psychiatry 75(6):813–821
Alperin N, Sang HL, Sivaramakrishnan S, Hushek SG (2005) Quantifying the effect of posture on intracranial physiology in humans by MRI flow studies. J Magn Reson Imaging 22:591596
Newell DW, Aaslid R, Stoos R, Reulen HJ (1992) The relationship of blood flow velocity fluctuations to intracranial pressure B-waves. J Neurosurg 76:415–421
Agid R, Farb RI, Willinsky RA, Mikulis DJ, Tomlinson G (2006) Idiopathic intracranial hypertension: the validity of cross-sectional neuroimaging signs. Neuroradiology 48:521–527
Messina D, Bono F, Fera F, Lanza P, Giliberto C, Lavano A, Quattrone A (2006) Empty sella and bilateral transverse sinus stenosis predict raised intracranial pressure in the absence of papilloedema. A preliminary study. J Neurol 253:674–676
Fera F, Bono F, Messina D, Gallo O, Lanza PL, Auteri W et al (2005) Comparison of different MR venography techniques for detecting transverse sinus stenosis in idiopathic intracranial hypertension. J Neurol 252:1021–1025
Farb RI, Vanek I, Scott JN, Mikulis DJ, Willinsky RA, Tomlinson G, terBrugge KG (2003) Idiopathic intracranial hypertension: the prevalence and morphology of sinovenous stenosis. Neurology 60:1418–1424
Bono F, Lupo MR, Lavano A, Mangone L, Fera F, Pardatscher K, Quattrone A (2003) Cerebral MR venography of transverse sinuses in subjects with normal CSF pressure. Neurology 61:1267–1270
Sarica A, Curcio M, Rapisarda L, Cerasa A, Quattrone A, Bono F (2019) Periventricular white matter changes in idiopathic intracranial hypertension. Ann Clin Transl Neurol. https://doi.org/10.1002/acn3.685
Bono F, Giliberto C, Lavano A, Quattrone A (2005) Posture-related cough headache and orthostatic drop in lumbar CSF pressure. J Neurol 252:237–238
Strassman AM, Raymond SA, Burstein R (1996) Sensitization of meningeal sensory neurons and the origin of headaches. Nature 384:560–564
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that he has no conflict of interest.
Ethical standards
This article does not contain any original study with human subjects performed by the author.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bono, F. Isolated cerebrospinal fluid hypertension in chronic headache: diagnostic innovations and clinical implications. Neurol Sci 40 (Suppl 1), 71–74 (2019). https://doi.org/10.1007/s10072-019-03836-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-019-03836-0