Abstract
The objective of this study was to evaluate the PTZ-induced seizures effects on GABAB receptor (R) expression and to observe its neurodegenerative effect in hippocampal part of developing rat brain. In the present study, high dose of pentylenetetrazol (PTZ 40 mg/kg) was injected in developing rats of age 5 weeks having average weight of 60–65 g for 4 days. Further, baclofen (B 3 mg/kg i.p) agonist and phaclofen (P 30 μg/rat) antagonist of GABABR were injected along with PTZ. Western blot analysis was used to elucidate expression of GABABR protein upon PTZ, baclofen and phaclofen exposure in the developing rat brain. Furthermore, PTZ-induced apoptotic neurodegeneration was also observed through the release of caspase-3 antibody and propidium iodide (PI) staining using confocal microscopy. Seizure was confirmed using electroencephalography (EEG) data obtained from the Laxtha EEG-monitoring device in the EEG recording room and EEG was monitored 5–15 min after PTZ injection. The results of the present study showed that PTZ-induced seizure significantly decreased GABABR expression and induced neuronal apoptosis in cortical and hippocampal part of brain. While, baclofen reverse the effect of PTZ by increasing the expression of GABABR as compared to the PTZ- , PTZ plus B- and PTZ plus P-treated groups. Our findings indicated that PTZ-induced seizure showed not only decrease in GABABR expression but also cause neuronal apoptosis in the developing rat brain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epilepsy is one of the most common neurological diseases worldwide that is estimated to affect 1–2 % of the world population [1]. This disorder is characterized by the occurrence of spontaneous and recurrent seizures that occur due to abnormal excessive and synchronous electrical activity of neuronal networks [2, 3].
It is well known that PTZ cause epileptic seizures and brain damage, acting on defined receptors groups and the consequences of status epilepticus in the developing brain differ from those of the mature brain [4, 5]. PTZ is a blocker of the chloride ionophore complex to the GABAAR [6] that has convulsant effects after repeated or single dose administration and also affects several neurotransmitter systems, such as the GABAergic and glutamatergic systems [7, 8].
The GABABRs are the members of the G-protein coupled receptors family that modulate multiple signal transduction pathways [9, 10]. Experimental evidences suggest that GABABR mechanisms might play a role in learning and memory processes [11], and its mechanisms may be altered in kindling [12]. Molecular expression studies and gene deletion experiments provide unequivocal evidence for modifications of GABABR in the development of seizures, hyperalgesia, hypothermia, memory impairment, anxiety and retarded growth all of which provide important clues about the role of GABABR in controlling brain function [13–15].
Baclofen, a g-aminobutyric acid (GABA) agonist, is widely used to treat spasticity of cerebral and spinal origin (including cerebral palsy, spinal cord injury, traumatic brain injury, multiple sclerosis) and dystonic disorders in both adults and children. Baclofen showed anticonvulsant [16, 17] and proconvulsant effects in animal models [18]. Phaclofen GABABR antagonist reduces ethanol intoxication, including impaired motor activity, coordination and thermoregulation, as well as anticonvulsant actions in mice [19, 20]. Further, GABABR antagonists have proconvulsant effects and produce focal seizures in cortical and limbic structures [21].
Previously, it is reported that cell death in the hippocampus is a well-established consequence of human epilepsy [22] and experimental animal seizure models [23, 24]. There are many potential mechanisms by which neurons may die after seizures, including excitotoxicity from excessive glutamate, release of nitric oxide, increased oxidative stress, as well as induction of apoptosis [25]. Recently, we have studied that PTZ-induced seizure cause apoptotic neurodegeneration and decreased GABAB1R expression in prenatal rat brain during pregnancy [26].
The aim of the present study was to examine the PTZ-induced seizures effect on GABABR expression and apoptotic neuronal death in hippocampal part of developing rat brain. Our results revealed that PTZ-induced seizure not only cause apoptotic neurodegeneration but also decreased GABABR expression in rat brain. These results provide evidence of apoptotic neurodegeneration and decreased GABABR expression in developing rat brain due to seizure induced by PTZ.
Methodology
Animals and drug treatment
Sparague-Dawley developing rats of 5 week average weight of 60–65 g (King Abdulaziz University, Neurobiology Laboratory, Jeddah, Saudi Arabia) were housed in a temperature-controlled environment with lights from 06:00 to 20:00 h with food ad libitum. Rats were injected i.p. with a dose of 40 mg/kg of PTZ in saline solution and co-treatment of baclofen (B 3 mg/kg i.p) agonist and phaclofen (P 30 μg/rat) antagonist of GABABR was done along with PTZ for 4 days.
EEG recording and seizure observation
Animals were injected intraperitoneally with sub convulsive doses of PTZ (40 mg/kg) in saline every day and control groups were given only saline injection. Convulsive behavior was observed for 30 min after each injection, and resultant seizures were scored as follows: stage 0, no response; stage 1, ear and facial twitching; stage 2, convulsive waves axially through the body; stage 3, myoclonic jerks and rearing; stage 4, clonic convulsions with the animal falling on its side; and stage 5, repeated severe tonic–clonic convulsions or lethal convulsions. EEG data were recorded for 5–10 min using amplifiers (LAXTHA, LXEJ 108) and were digitized at 250 Hz in EEG recording room. Whole EEG samples were analyzed by visual inspection for the presence of epileptic form activity as previously defined [27].
Western blotting
Animal were killed after 4 days of PTZ, PTZ plus baclofen, PTZ plus phaclofen and PTZ plus baclofen and phaclofen treatments. Brains were dissected out and hippocampal part was removed carefully and tissue was frozen in dry ice. For each treatment group, three to four rats were analyzed. The brain tissues were homogenized in 0.2 M PBS with protease inhibitor cocktail. The protein concentration was measured using Bio-Rad protein assay solution. Equivalent amounts of protein (30 μg per sample) were electrophoresed on 10 % SDS-PAGE gels under reducing conditions and transferred to a polyvinylidene difluoride (PVDF) membrane (Santa Cruz Biotechnology, Santa Cruz, CA, USA). Prestained protein markers, broad range (6–175 kDa, New England Biolabs Inc., Ipswich, MA, USA), were run in parallel for the detection of the molecular weights of the protein. GABABR analysis was done as previously described with some modification [23]. Western blots were analyzed by densitometry using the computer-based Sigma Gel (SPSS Inc. Chicago, USA) system. In every case, the acceptance level for statistical significance was *P < 0.05.
Tissue collection and sample preparation
Animals were killed after 4 days of drug treatment. Brain sections from control rats and rats subjected to PTZ followed by baclofen were analyzed. For tissue analysis (n = 4–5 per group), developing rats were perfused transcardially with 4 % ice-cold paraformaldehyde followed by 1 × PBS; brains were post-fixed in 4 % paraformaldehyde overnight and then transferred to 20 % sucrose until they sank to the bottom of the tubes. Brains were frozen in O.C.T compound (A.O. USA) and 16 μm sections were made in the coronal planes using a Leica cryostat (CM 3050C, Germany). Sections were thaw-mounted on probe-on plus charged slides (Fisher).
Visualization of caspase-3 expression and PI staining by using confocal microscopy
The analysis of caspase-3 expression and PI staining was carried out by immunofluorescence technique. Tissue sections of cortex and hippocampus were prepared as mentioned above. Caspase-3 expression was detected using rabbit anti-caspase-3 antibody (Cell signaling) over night at 4 °C and goat anti-rabbit FITC-labeled secondary antibody (Santa Cruz Biotechnology, CA, USA) for 90 min at room temperature (1:250 and 1:100, respectively; Santa Cruz Biotechnology, CA, USA). Propidium iodide (PI) staining was performed as previously described [28]. For PI, slides were dipped in 1 mg/mL of PI solution in PBS for 20 min at room temperature with gentle mixing and washed twice with PBS for 10 min. Glass cover slip was mounted on glass slides with mounting medium. PI filter was used to detect the PI staining (red color). Images were taken by use of a confocal laser scanning microscope (Fluoview FV 1000, Olympus, Japan).
Nissl staining
Cresyl violet was used to stain tissue sections for histological examination and measurement of neuronal loss. Nissl histology of developing rat brain and the presence and absence of dead and injured neurons were analyzed on microscope using slides mounted with 16 μm thick brain sections. Sections derived from all investigated rat pups were defatted in ascending alcohols (70–100 %), hydrated in descending alcohols (95–70 %), washed in acetate buffer pH 5.0 and subsequently stained with a 0.25 % cresyl violet for approximately 15 min. Sections were then washed with distilled water and dehydrated in graded ethanol. Images were viewed with a fluorescence light microscope.
Data analysis and statistics
Western blots were scanned and analyzed by densitometry using a computer based on the Sigma Gel System (SPSS Inc., Chicago, IL, USA). Density values were expressed as mean ± SEM. Comparisons between treated groups and controls were done by Student‘s t test to determine the significance of differences between relevant treatment groups. In every case, the acceptance level for statistical significance was P < 0.05.
Results
PTZ-induced seizures
A convulsant dose of pentylenetetrazol (PTZ) (40 mg/kg, i.p.) was administered for 4 days in developing rats. After injection of PTZ, occurrence of central nervous system (CNS) excitation was noted for 5–30 min by observing the animal’s behavior in a plexiglass chamber. Convulsive dose of PTZ 40 mg/kg for 4 days induced minimal seizures. In addition, barrel rotations and tonic seizures were noticed in some of the animals: 65 % of the animals after the 4th injection. A seizure induced by PTZ in developing rat started with hindlimb kicks, followed by generalized tonic and clonic convulsion of four limbs while laying down. The results of seizure observations after PTZ injections are summarized in Table 1. To confirm the seizure induced by PTZ, EEG recording was monitored for 30 min and started 3 min after the PTZ injection. Five rats from the control group and five from the PTZ-treated group were monitored for EEG recording. The results for the evaluation of EEG monitoring are summarized in Fig. 1.
Representative EEG traces in adult rat after 4th injections of PTZ, PTZ plus B, PTZ plus P. Representative 30 s EEG samples recorded 15 min after 5th injection of PTZ (40 mg/kg). a Showed normal EEG in saline group as a base line, b EEG 15 min after 4th PTZ injection and c EEG after PTZ + B injection, d EEG after PTZ + P injection
GABABR expression upon PTZ-induced seizure in rat brain
To explore the in vivo changes of GABABR expression and its relation with PTZ-induced seizure in hippocampal neuronal cells, samples of protein from rat brain were studied using Western blot analysis. The results showed that PTZ-induced seizure significantly decreased GABABR expression in hippocampal neurons (Fig. 2), whereas baclofen (GABABR agonist) treatment along with PTZ injection reverse this process. Further, phaclofen (GABABR antagonist) treatment along with PTZ also decreased the GABABR expression as compared to the control groups. Moreover, the co-treatment of baclofen and phaclofen along with PTZ showed significant increased expression as compared to PTZ-treated group. Thus, the decreased protein level of GABABR upon PTZ exposure suggests that PTZ-induced seizure modulates the GABABR protein expression in the developing rat brain.
Western blot analyses of the GABABR in the hippocampal brain. Developing rat of 5-week old was treated with PTZ 40 mg/kg while baclofen and phaclofen was treated along with PTZ injection. Saline was injected as control (c), rat treated with PTZ, rat treated with PTZ + B, rat treated with PTZ + P and rat treated with PTZ + B + P. β-actin is taken as loading control. a Immunoblots of GABABR of hippocampal area under different treatment conditions. The immunoblots were labeled with GABABR antibody. b Density values were expressed as mean ± SEM (n = 4) of the corresponding protein of GABABR are presented. The density values on the Y-axis are expressed as arbitrary units (AU). *P < 0.05 versus control group
Release of caspase-3 and PI expression upon PTZ-induced seizure in developing rat brain
To study the effect of PTZ-induced apoptotic neurodegeneration in cortical and hippocampal part of rat brain, animals were treated with PTZ, baclofen and PTZ plus baclofen for 4 days. The ability of PTZ-induced seizure to induce neuronal cell death such as the activation of caspase-3 was studied. The translocation of caspase-3 along with PI stains using confocal microscopy was observed, which revealed a diffuse staining pattern of caspase-3 and PI, suggesting increase in neuronal apoptosis (caspase-3, green FITC-labeled) along with (PI, red) upon PTZ treatment in the developing rat cortex and hippocampus. Figure 3 illustrated that exposure of PTZ caused significant increase around 50 % expression of caspase-3 and PI level in cortex and hippocampus of rat brain as compared to control group, while the co-treatment of PTZ with baclofen showed 20–25 % decrease in expression of caspase-3 and PI stains as compared to the PTZ-treated group, suggesting that baclofen protects the PTZ-induced apoptotic neurodegeneration (Fig. 3).
a Developing rats were injected with saline (Control) PTZ and PTZ plus baclofen. Animals were killed at 12 h after PTZ injection for analysis. Shown are tissue sections from anterior cingulate cortex and CA1 region of the hippocampus that were double stained for caspase-3 (FITC-label, green) and PI (TRITC-label, red). a–f Magnification with 40× objective field, Scale bar 20 μm. b Number of shrunken and damaged neurons were counted and represented in graph. Graphic representation of saline, PTZ and PTZ plus baclofen effect groups in developing rat brain after PTZ-induced apoptotic neurodegeneration in cortical and hippocampal part of brain. Significance *P < 0.05 versus control group. Magnification 40×; Scale bar 20 μm (color figure online)
PTZ-induced seizure cause neuronal cell death in developing rat brain
Further, Nissl staining was used to measure the extent of neuronal cell death upon PTZ-induced seizure in the cortex and hippocampus of the developing rats. Dying neurons in the section allow identification of cells demonstrating clear light microscopic morphological hallmarks of apoptosis (with large, round, chromatin clumps). An increased vacuolization and neuronal loss in the cortex and hippocampus was observed in PTZ-treated group as compared to the control (Fig. 4). Moreover, the co-treatment of PTZ with baclofen was associated with less vacuolization and neuronal loss, in these vulnerable brain regions (Fig. 4), and showed a significant neuroprotection against PTZ-induced apoptotic cell death as compared to the PTZ groups.
Histopathological changes in cortical and hippocampal part of the brain-treated saline as controls, PTZ and PTZ plus baclofen groups a–c cortex and d–f hippocampus. The arrows indicate shrunken and damaged neurons. Nissl-stained brain tissue at higher magnification with 40× objective field, Scale bar 50 μm
Discussion
In the present study, we have observed the PTZ-induced seizure’s effect on expression of GABABR and neuronal cell death in developing rat brain. Our results showed that PTZ-induced epileptic seizure elicited decreased in GABABR expression and increased in neuronal cell death in the cortex and hippocampus of the developing rat brain. Epileptic rats were examined using Western blot analysis for GABABR expression analysis while, release of caspase-3, PI and Nissl staining was used for the detection of neurodegeneration in the developing brain.
PTZ produces proconflict and convulsant effects in rodents [29], but cognitive deficits have also been noted [30]. PTZ-induced seizure is associated with an imbalance between excitatory and inhibitory neurotransmissions where long-term reduction of GABA-mediated inhibition in the cortex increases the seizure susceptibility [31, 32]. GABAAR mediate most fast inhibitory synaptic transmission in the central nervous system (CNS). The evidence that altered function of GABAAR subtypes is closely related to epileptogenesis has been elucidated in animal models and human epilepsy [33, 34]. Furthermore, pharmacological effects of PTZ appear to be mediated through a specific interaction with the GABA-gated chloride ionophore. GABAAR are involved in the control of neuronal excitability and epileptogenesis in the generalized convulsive seizures [35].
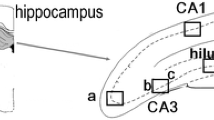
Previously, it has been reported that transient decreases in GABAB1R mRNA expression occurs in all subfields of the hippocampus after KA-induced seizures [36]. Since the early decreases in GABAB-R mRNAs in CA1 and CA3 pyramidal cells essentially preceded the prominent seizure-induced cell losses seen in animal model [36, 37]. It is also reported that the GABABR showed altered expression in the hippocampus of epileptic patients [38, 39], kindling rat [40], electroshock-induced seizure rat [38] and kainate-induced mouse epilepsy models [41].
Our results also showed that co-treatment of baclofen along with PTZ significantly reversed the effect of PTZ-induced seizure decreased in GABABR expression and apoptotic neurodegeneration in developing rat brain. Previously, it is also reported that baclofen treatment might result in block of asynchronous GABA-mediated potentials and activity-dependent changes in hippocampal network excitability [42]. These baclofen effects may be mediated by disinhibition through both presynaptic and postsynaptic GABABR in inhibitory interneuron. Further, activation of pre and postsynaptic GABABR on GABAergic neurons evokes transient interruption of GABAAR due to decreased GABA release [18]. Moreover, baclofen treatment results in activation of GABABR on principal neurons, which inhibits principal neurons. GABABR agonists have antiepileptic activity in convulsive seizures [43, 44]. However, opposite GABABR functions have also been reported [12, 45]. Moreover, the opposite effects of the GABABR agonist and antagonist were observed in both seizure models only in 25-day-old rats. Surprisingly, baclofen exhibited an anticonvulsant action against an absence model in 18-day-old animals [46]. This developmental irregularity cannot yet be explained, only some possibilities might be outlined. Developmental changes of coupling of GABABR with G proteins cannot be excluded but no systematic study is at disposal.
In the present study, we have observed that PTZ-induced seizure decreased GABABR expression and induced apoptotic neuronal death in developing rat brain. The present study also demonstrated that co-treatment of baclofen along with PTZ significantly improved neuronal survival, prevents PTZ-induced seizure and apoptotic neurodegeneration in the cortical and hippocampal part of rat brain. Therefore, our results suggested that epileptic activity in hippocampal part of brain may be related with alteration in GABABR expression. Moreover, seizure induced by PTZ decreased GABABR expression and cause neuronal degeneration in the developing rat brain.
References
Browne TR, Holmes GL (2001) Epilepsy. N Engl J Med 344:1145–1151
Elger CE, Schmidt D (2008) Modern management of epilepsy: a practical approach. Epilepsy Behav 12:501–539
Fisher RS, van Emde Boas W, Blume W, Elger C, Genton P, Lee P, Engel J Jr (2005) Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia 46:470–472
Rauca C, Zerbe R, Jantze H (1999) Formation of free hydroxyl radicals after pentylenetetrazol-induced seizure and kindling. Brain Res 847:347–351
Sperk G (1994) Kainic acid seizures in the rat. Prog Neurobiol 42:1–32
Huang RQ, Bell-Horner CL, Dibas MI, Covey DF, Drewe JA, Dillon GH (2001) Pentylenetetrazol-induced inhibition of recombinant gamma-aminobutyric acid type A (GABA(A)) receptors: mechanism and site of action. J Pharmacol Exp Ther 298:986–995
Jensen FE, Applegate C, Burchfiel J, Lombroso CT (1991) Differential effects of perinatal hypoxia and anoxia on long term seizure susceptibility in the rat. Life Sci 49:399–407
Psarropoulou C, Matsokis N, Angelatou F, Kostopoulos G (1994) Pentylenetetrazol-induced seizures decrease gamma-aminobutyric acid-mediated recurrent inhibition and enhance adenosine-mediated depression. Epilepsia 35:12–19
Bormann J (2000) The ‘‘ABC’’ of GABA receptors. Trends Pharmacol Sci 21:16–19
Bowery NG (1993) GABAB receptor pharmacology. Annu Rev Pharmacol Toxicol 33:109–147
Mondadori C, Jaekel J, Preiswerk G (1993) The first orally active GABA blocker improves the cognitive performance in mice, rats and rhesus monkeys. Behav Neurol Biol 60:62–68
Getova D, Froestl W, Bowery NG (1998) Effects of GABAB receptor antagonism on the development of pentylenetetrazol-induced kindling in mice. Brain Res 809:182–188
Mombereau C, Kaupmann K, Froestl W, Sansig G, Putter H van der, Cryan JF (2004) Genetic and pharmacological evidence of a role for GABAB receptors in the modulation of anxiety- and antidepressant-like behavior. Neuropsychopharmacology 29:1505–1062
Prosser HM, Gill CH, Hirst WD, Grau E, Robbins M, Calver A, Soffin EM, Farmer CE, Lanneau C, Gray J, Schenck E, Warmerdam BS, Clapham C, Reavill C, Rogers DC, Stean T, Upton N, Humphreys K, Randall A, Geppert M, Davies CH, Pangalos MN (2001) Epileptogenesis and enhanced prepulse inhibition in GABA(B1)-deficient mice. Mol Cell Neurosci 17:1059–1070
Schuler V, Luscher C, Blanchet C (2001) Epilepsy, hyperalgesia, impaired memory, and loss of pre- and postsynaptic GABAB responses in mice lacking GABAB(1). Neuron 31:47–58
Ault B, Nadler JV (1983) Anticonvulsant-like actions of baclofen in the rat hippocampal slice. Br J Pharmac 78:701–708
Benedito MA, Leite JR (1981) Baclofen as an anticonvulsant in experimental models of convulsions. Exp Neurol 72:346–351
Mott DD, Bragdon AC, Lewis DV, Wilson WA (1989) Baclofen has a proepileptic effect in the rat dentate gyrus. J Pharmacol Exp Ther 249:721–725
Allan AM, Harris RA (1989) A new alcohol antagonist: phaclofen. Life Sci 45:1771–1779
Mehta AK, Ticku MK (1990) Are GABAB receptors involved in the pharmacological effects of ethanol? Eur J Pharmacol 182:473–480
Vergnes M, Boehrer A, Simler S, Bernasconi R, Marescaux C (1997) Opposite effects of GABAB receptor antagonists on absences and convulsive seizures. Eur J Pharmacol 332:245–255
Arzimanoglou A, Hirsch E, Nehlig A, Castelnau P, Gressens P, Pereira de Vasconcelos A (2002) Epilepsy and neuroprotection: an illustrated review. Epileptic Disord 4:173–182
Represa A, Niquet J, Pollard H, Ben-Ari Y (1995) Cell death, gliosis, and synaptic remodeling in the hippocampus of epileptic rats. J Neurobiol 26:413–425
Turski WA, Cavalheiro EA, Schwarz M, Czuczwar SJ, Kleinrok Z, Turski L (1983) Limbic seizures produced by pilocarpine in rats: behavioral, electroencephalographic and neuro-pathological study. Behav Brain Res 9:315–335
Friedman WJ (2010) Proneurotrophins, seizures, and neuronal apoptosis. Neuroscientist 16:244–252
Naseer MI, Li S, Kim MO (2009) Maternal epileptic seizure induced by Pentylenetetrazol: apoptotic neurodegeneration and decreased GABAB1 receptor expression in prenatal rat brain. Mol Brain 2:20
Kondo S, Najm I, Kunieda T, Perryman S, Yacubova K, Luders HO (2001) Electroencephalographic characterization of an adult rat model of radiation-induced cortical dysplasia. Epilepsia 42:1221–1227
Johnson JE (1995) Methods for studying cell death and viability in primary neuronal cultures. Methods Cell Biol 46:243–276
Becker A, Grecksch G, Mathies H (1994) The influence of diazepam on learning processes impaired by pentylenetetrazol kindling. Naunyn-Schmiedeberg’s Arch. Pharmacol 349:429–496
Howe JR, Sutor B, Ziegelgansberger W (1987) Baclofen reduces postsynaptic potentials of rat cortical neurones by an action other than its hyperpolarizing action. J Physiol 384:539–569
Rocha L, Briones M, Ackermann RF, Anton B, Maidment NT, Evans CJ, Engel J (1996) Pentylenetetrazol-induced kindling: early involvement of excitatory and inhibitory systems. Epilepsy Res 26:105–113
Corda MG, Biggio G (1986) Proconfict effect of GABA receptor complex antagonists. Reversal by diazepam. Neuropharmacology 25:541–544
Brooks-Kayal AR, Shumate MD, Jin H, Rikhter TY, Coulter DA (1998) Selective changes in single cell GABA(A) receptor subunit expression and function in temporal lobe epilepsy. Nat Med 4:1166–1172
McDonald JW, Garofalo EA, Hood T, Sackellares JC, Gilman S, McKeever PE, Troncoso JC, Johnston MV (1991) Altered excitatory and inhibitory amino acid receptor binding in hippocampus of patients with temporal lobe epilepsy. Ann Neurol 29:529–541
Mohler H, Benke D, Benson J, Lüscher B, Rudolph U, Fritschy JM (1997) Diversity in structure, pharmacology, and regulation of GABAA receptors. In: Enna SJ, Bowery NG (eds) The GABA receptors. Humana Press, Totowa, pp 203–209
Tsunashima K, Schwarzer C, Kirchmair E, Sieghart W, Sperk G (1997) GABAA-receptor subunits in the rat hippocampus III: altered expression of their mRNAs in kainic acid-induced epilepsy. Neuroscience 80:1019–1032
Nicholson DW (1999) Caspase structure, proteolytic substrates, and function during apoptotic cell death. Cell Death Differ 6:1028–1042
Billinton A, Stean TO, Bowery NG, Upton N (2000) GABA(B(1)) splice variant mRNAs are differentially affected by electroshock-induced seizure in rats. Neuroreport 11:3817–3822
Muñoz A, Arellano JI, De Felipe J (2002) GABABR1 receptor protein expression in human mesial temporal cortex: changes in temporal lobe epilepsy. J Comp Neurol 449:166–179
Kokaia Z, Kokaia M (2001) Changes in GABA(B) receptor immunoreactivity after recurrent seizures in rats. Neurosci Lett 315:85–88
Straessle A, Loup F, Arabadzisz D, Ohning GV, Fritschy JM (2003) Rapid and long-term alterations of hippocampal GABAB receptors in a mouse model of temporal lobe epilepsy. Eur J Neurosci 18:2213–2226
Motalli R, Louvel J, Tancredi V, Kurcewicz I, Wan-Chow-Wah D, Pumain R, Avoli M (1999) GABA(B) receptor activation promotes seizure activity in the juvenile rat hippocampus. J Neurophysiol 82:638–647
Karlsson G, Kolb C, Hausdorf A, Portet C, Schmutz M, Olpe HR (1992) GABAB receptors in various in vitro and in vivo models of epilepsy: a study with the GABAB receptor blocker CGP 35348. Neuroscience 47:63–68
Wurpel JN (1994) Baclofen prevents rapid amygdala kindling in adult rats. Experientia 50:475–478
Sarro De, Palma E, Costa N, Marra R, Gratteri S, De Sarro A, Rotiroti D (2000) Effects of compounds acting on GABA(B) receptors in the pentylenetetrazole kindling model of epilepsy in mice. Neuropharmacology 39:2147–2161
Velisek L, Veliskova J, Ptachewich Z, Ortiz J, Shinnar S, Moshe SL (1995) Age-dependent effects of GABA agents on flurothyl seizures. Epilepsia 36:636–643
Acknowledgment
This work was supported by Ministory of Higher Education Saudi Arabia and CEGMR grant No (12-02).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Naseer, M.I., Ullah, I., Al-Qahtani, M.H. et al. Decreased GABABR expression and increased neuronal cell death in developing rat brain after PTZ-induced seizure. Neurol Sci 34, 497–503 (2013). https://doi.org/10.1007/s10072-012-1083-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-012-1083-0