Abstract
Mood and anxiety disorders are comorbid with migraine. The coexistence of a psychiatric disorder alters the quality of life, the total disability, the course of migraine and the final prognosis; it increases the probability of central sensitization, other chronic pain conditions and the evolution to chronic migraine. All patients presenting with frequent episodic and chronic migraine should be screened for depression and anxiety. When these conditions are present, drugs for migraine prevention that may worsen the psychiatric comorbid disorder have to be avoided. When it is possible, both conditions should be treated with a single agent. Amitriptiline can be used both in mood disorders and migraine prevention. Flunarizine and beta-blockers may help if anxiety is present. Pregabalin has demonstrated efficacy in anxiety disorders and fibromyalgia. Divalproex sodium, topiramate and lamotrigine that have demonstrated efficacy in mood stabilization are also indicated in migraine without aura (divalproex sodium and topiramate) and with aura (lamotrigine). When a specific treatment for the comorbid psychiatric disorder is needed, the selective serotonin reuptake inhibitors or the serotonin norepinephrine reuptake inhibitors are the drugs of choice both in depression and anxiety, and the cognitive behavioural therapy has good evidence of efficacy in anxiety disorders. Vagal nerve stimulation may be an option in patients with refractory chronic migraine and depression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The association between migraine and several psychiatric disorders has been well demonstrated [1, 2]; the most important comorbidity appears to be with mood, anxiety and panic disorders.
The migraineurs have a fivefold higher risk of depression, and longitudinal studies have shown that the relationship is bidirectional, in patients with depression having a threefold higher risk of migraine. This bidirectionality suggests that migraine and depression share a common neurobiology. Moreover, compared to individuals without migraine, migraineurs are at 4–5 times greater risk for generalized anxiety disorder (GAD) [3–5], at five times greater risk for obsessive–compulsive disorder (OCD) [3], and run 3–5 times higher risk of suffering from panic disorder [1–5]. An increased risk is demonstrated for suicide ideation too, especially in migraine with aura [4].
The onset of anxiety often precedes migraine, while the risk of depression usually increases later [4].
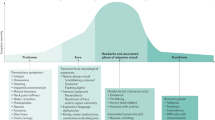
From a clinical point of view, the coexistence of a psychiatric disorder has many practical implications: it alters the quality of life, the total disability, the course of migraine and the final prognosis. We know that a subgroup of migraine sufferers evolves from a stage of episodic migraine into a stage in which the pain is present almost daily (chronic migraine). Several factors have been associated with migraine clinical progression: depression and stressful life events are independent risk factors for progression and may affect other negative variables such as obesity and medications overuse [6]. The relationship between obesity and migraine frequency is modified by depression and anxiety, and the strongest effect on migraine frequency is observed in migraineurs with both depression and anxiety. A complex relationship exists with sleep disorders that may result from or may cause headache [7]. Depression and anxiety cause disturbed sleep, and sleep deprivation or excessive sleep may increase the frequency of migraine attacks.
There are many clinical evidences that depression plays a role in the processing and perception of pain, and that depressed patients are more vulnerable to painful physical symptoms. Cutaneous allodynia is the perception of pain or discomfort in response to non-noxious thermal and mechanical stimuli applied to normal skin; it is a clinical marker of central sensitization, and is more common in frequent and chronic migraine. Some studies [8, 9] report the association between cutaneous allodynia and both anxiety and depression, which probably support the central sensitization. Furthermore, migraine and depression are associated to other comorbid pain conditions (irritable bowel syndrome, chronic fatigue syndrome and fibromyalgia) that share the common mechanism of central sensitization and have common clinical correlates such as allodynia and hyperalgesia.
The first clinical implication of the previous considerations is that all patients presenting with frequent episodic and chronic migraine should be screened for depression and anxiety. We have seen that psychiatric comorbidity contributes to poor prognosis and poor quality of life, but we do not examine the effect of treatments both for migraine prevention and for mood and anxiety disorders on final outcomes.
Heckman et al. [10] prospectively examine how psychiatric disorders relate to treatment outcome in a group of patients with primary headaches. They confirm that psychiatric comorbidity is very frequent (two-thirds of their patients were diagnosed with one or more psychiatric disorders), and that the presence of a comorbid depressive disorder is associated with more frequent and disabling headaches, and also find that patients with psychiatric disorder improve equally as well as patients with no psychiatric disorder. In this study, patients received the “best” state-of-the-science treatment and, of course, those with a mood disorder were more likely to be prescribed antidepressant therapies. The conclusion may be that a migraine patient with psychiatric comorbidity is a difficult one; often he begins treatment with more headache days, more disability, and poorer quality of life, but has good expectations of improvement, if psychiatric comorbidity is treated. Moreover, treating anxiety and depression means to prevent central sensitization and the evolution to chronic migraine.
Therapeutic strategies
Specific therapeutic guidelines for depression and anxiety in migraine are lacking. First of all, choosing a drug for migraine prevention that may worse the psychiatric comorbid disorder has to be avoided: this is true for flunarizine and beta-blockers in depression. When it is possible, treatment of both conditions would be accomplished with a single agent. Between the drugs with known effect on migraine prevention: beta-blockers and flunarizine may help if anxiety is present; amitriptiline is indicated in mood disorders, but the dose required for treating migraine may be insufficient to treat the affective disorder, and larger dose may cause collateral effects.
In specific cases, some drugs may play a role in both migraine and psychiatric comorbidity.
Pregabalin is indicated in anxiety disorders (see later), and has recently been approved in the United States for the treatment of fibromyalgia that, as we have seen, is one of the chronic pain conditions associated with migraine and depression. Furthermore, it might be a useful alternative prophylaxis for chronic migraine [11, 12].
Divalproex sodium (VPA), topiramate [13] and lamotrigine [14, 15] have demonstrated efficacy in bipolar depression. The efficacy of VPA and topiramate in migraine prevention has been shown in several double blind, randomised, placebo-controlled trials [16, 17], and some studies suggest that lamotrigine constitutes a specific prophylactic treatment of migraine with aura [18–20].
The migraineurs can sometimes derive benefit from some less traditional approaches, such as riboflavin or coenzyme Q10 [21], which have marginal evidence in depression in specific cases [22, 23].
When a single agent has insufficient effect or is not tolerated, two different drugs must be used: one for migraine prevention and one for the psychiatric disorder.
The American College of Physicians [24] recommends the second-generation antidepressants as the treatment of choice for acute episodes of major depression without striking differences between selective serotonin reuptake inhibitors (SSRIs), serotonin norepinephrine reuptake inhibitors (SNRIs) and selective serotonin norepinephrine reuptake inhibitors (SSNRIs). Treatment must be modified if the patient does not have an adequate response to pharmacotherapy within 6–8 weeks and must be continued for 4–9 months after a satisfactory response.
For GAD, OCB and panic disorder [25, 26], the interventions that have evidence for the longest duration of effects are pharmacological therapy and psychological therapy (cognitive behavioural therapy). First-line pharmacological treatments are SSRIs, SNRIs and the calcium channel modulator pregabalin. Tricyclic antidepressants (TCAs) are equally effective for some disorders, but many are less well tolerated than the SSRIs/SNRIs. In treatment-resistant cases, benzodiazepines may be used when the patient does not have a history of substance abuse disorders.
The increase of synaptic serotonin, a common effect both of SSRIs/SNRIs and amitriptiline, seems to be critical for efficacy on depression but not for migraine prevention activity. In fact SSRIs/SNRIs have poor evidence of efficacy in preventive treatment of migraine [27], and in most cases a second drug must be added. However, some studies indicate a possible clinical benefit in migraine prevention of sertraline, fluoxetine and venlafaxine. Interestingly, the efficacy becomes evident only from the third month of treatment or later [27]. The FDA recommends that patients treated concomitantly with a triptan and a SSRI/SNRI be informed of the rare possibility of serotonin syndrome [28]. Chronic migraine can in some cases evolve in drug refractory chronic daily headache, a highly disabling condition characterized by high prevalence of psychiatric disorders and by a resistance to all known treatments. Vagal nerve stimulation (VNS) is an established treatment option for selected patients with medically refractory epilepsy and depression. Small case series support a beneficial effect of chronic VNS in patients with both drug refractory chronic migraine and depression [29], offering a chance in an otherwise intractable condition.
References
Radat F, Swendsen J (2004) Psychiatric comorbidity in migraine: a review. Cephalalgia 25:165–178
Lake AE, Rains JC, Penzien DB, Lipchik GL (2005) Headache and psychiatric comorbidity: historical context, clinical implications, and research relevance. Headache 45:493–506
Hamelsky SW, Lipton RB (2006) Psychiatric comorbidity of migraine. Headache 46:1327–1333
Breslau N, Davis GC, Andreski P (1991) Migraine, psychiatric disorders, and suicide attempts: an epidemiologic study of young adults. Psychiatry Res 137:11–23
Baskin SM, Todd Æ, Smitherman A (2009) Migraine and psychiatric disorders: comorbidities, mechanisms, and clinical applications. Neurol Sci 30(Suppl 1):S61–S65
Bigal M, Lipton RB (2009) What predicts the change from episodic to chronic migraine? Curr Opin Neurol 22:269–276
Tietjen GE, Brandes JL, Peterlin BL, Eloff A, Dafer RM, Stein MR, Drexler E, Martin VT, Hutchinson S, Aurora SK, Recober A, Herial NA, Hutley C, White L, Khunder SA (2009) Allodynia in migraine: association with comorbid pain conditions. Headache 49:1333–1344
Scher AI, Lipton RB, Stewart WF (2003) Habitual snoring as a risk factor for chronic daily headache. Neurology 60:1366–1368
Bigal ME, Ashina S, Burstein R (2008) Prevalence and characteristics of allodynia in headache sufferers: a population study. Neurology 70:1525–1533
Heckman BD, Holroyd KA, Himawan L, O’Donnell FJ, Tietjen G, Utley C, Stillman M (2009) Do psychiatric comorbidities influence headache treatment outcomes? Results of a naturalistic longitudinal treatment study. Pain 146:56–64
Krymchantowski AV, Bryson J, Lipton RB, Bigal ME (2008) Neuromodulators for the treatment of headache disorders and fibromyalgia. Curr Pain Headache Rep 12(5):333–337
Calandre EP, Garcia-Leiva JM, Rico-Villademoros F, Vilchez JS, Rodriguez-Lopez CM (2010) Pregabalin in the treatment of chronic migraine: an open-label study. Clin Neuropharmacol 33(1):35–39
Maidment ID (2002) The use of topiramate in mood stabilization. Ann Pharmacother 36(7–8):1277–1281
Frye M, Ketter T, Kimbrell T et al (2000) A placebo-controlled study of lamotrigine and gabapentin monotherapy in refractory mood disorders. J Clin Psychopharmacol 20:607–614
Calabrese J, Bowden C, Sachs G et al (2003) A placebo-controlled 18-month trial of lamotrigine and lithium maintenance treatment in recently depressed patients with bipolar I disorder. J Clin Psychiatry 64:1013–1102
Klapper J (1997) Divalproex sodium in migraine prophylaxis: a dose-controlled study. Cephalalgia 17:103–108
Vikelis M, Rapoport AM (2010) Role of antiepileptic drugs as preventive agents for migraine. CNS Drugs 24(1):21–33
Steiner TJ, Findley LJ, Yuen AW (1997) Lamotrigine versus placebo in the prophylaxis of migraine with and without aura. Cephalalgia 17:109–112
D’Andrea G, Granella F, Cadaldini M, Manzoni GC (1997) Effectiveness of lamotrigine in the prophylaxis of migraine with aura: an open pilot study. Cephalalgia 19:64–66
Lampl C, Katsarava Z, Diener HC, Limmroth V (2005) Lamotrigin reduces migraine aura and migraine attacks in patients with migraine with aura. J Neurol Neurosurg Psychiatry 76:1730–1732
Schürks M, Diener HC, Goadsby P (2008) Update on the prophylaxis of migraine. Curr Treat Options Neurol 10(1):20–29
Bell IR, Edman JS, Morrow FD, Marby DW, Perrone G, Kayne HL, Greenwald M, Cole JO (1992) Vitamin B1, B2, and B6 augmentation of tricyclic antidepressant treatment in geriatric depression with cognitive dysfunction. Am Coll Nutr 11(2):159–163
Maes M, Mihaylova I, Kubera M, Uytterhoeven M, Vrydags N, Bosmans E (2009) Lower plasma Coenzyme Q10 in depression: a marker for treatment resistance and chronic fatigue in depression and a risk factor to cardiovascular disorder in that illness. Neuro Endocrinol Lett 30(4):462–469
Qaseem A, Snow V, Denberg TD, Forciea MA, Owens DK, for the Clinical Efficacy Assessment Subcommittee of the American College of Physicians (2008) Using second-generation antidepressants to treat depressive disorders: a clinical practice guideline from the American College of Physicians. Ann Intern Med 149:725–733
NICE guidelines. Anxiety: management of anxiety (panic disorder, with or without agoraphobia, and generalised anxiety disorder) in adults in primary, secondary and community care. http://guidance.nice.org.uk/CG22
WFSBP Task Force on Treatment Guidelines for Anxiety, Obsessive-Compulsive and Post-Traumatic Stress Disorders (2008) World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the pharmacological treatment of anxiety, obsessive-compulsive and post-traumatic stress disorders—first revision. World J Biol Psychiatry 9(4):248–312
Colombo B, Annovazzi POL, Comi G (2004) Therapy of primary headaches: the role of antidepressants. Neurol Sci 25:S171–S175
Evans RW (2007) The FDA alert on serotonin syndrome with combined use of SSRIs or SNRIs and triptans: an analysis of the 29 case reports. MedGenMed 9(3):48
Proietti Cecchini A, Mea E, Tullo V, Curone M, Franzini A, Broggi G, Savino M, Bussone G, Leone M (2009) Vagus nerve stimulation in drug-resistant daily chronic migraine with depression: preliminary data. Neurol Sci 30(Suppl 1):S101–S104
Conflict of interest statement
The authors declare that they have no conflict of interest related to the publication of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Finocchi, C., Villani, V. & Casucci, G. Therapeutic strategies in migraine patients with mood and anxiety disorders: clinical evidence. Neurol Sci 31 (Suppl 1), 95–98 (2010). https://doi.org/10.1007/s10072-010-0297-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-010-0297-2