Abstract
Previous reports have suggested an increased risk of psoriasis in MS patients. Worsening of dermatologic lesions during interferon therapy has been rarely reported, but activation of psoriatic arthritis has not been described until now. The following is a case report. A 37-year-old woman affected by relapsing–remitting multiple sclerosis had severe worsening of cutaneous psoriasis and activation of psoriatic arthritis during interferon beta treatment. The symptoms resolved after therapy discontinuation. This case further supports that activation of psoriasis might be a rare side effect of IFNB therapy and suggests careful evaluation of concomitant morbidity to allow a patient-oriented treatment strategy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Interferon beta (IFNB) is the first-line therapy for relapsing–remitting (RR) multiple sclerosis (MS). It reduces clinical exacerbations, and new brain lesions detected by magnetic resonance imaging (MRI). Flu-like syndrome and dermal injection site reactions are the most common side effects [1, 2]. The occurrence or recurrence of autoimmune diseases is well documented during IFNB therapy [1]; this may be related to the drug itself or to an increased susceptibility to autoimmune disorders in MS patients [3].
Psoriasis occurs in MS patients, although the evidence of the association is uncertain [3–6]. Exacerbation of cutaneous psoriasis has been rarely reported in MS patients treated with IFNB [2, 7–9], while psoriatic arthritis (PsA) has not till now described.
We report a patient affected by RR MS who had worsening of cutaneous psoriasis and activation of arthritis during IFNB therapy. Psoriasis resolved after IFNB’s withdrawal and during azathioprine therapy. This case further supports that activation of psoriasis and development of PsA might be rare side effects of IFNB therapy and suggests to carefully evaluate concomitant morbidity in order to allow a patient-oriented treatment strategy.
Case report
A 37-year-old woman was affected by RR MS from 22 years of age and by mild hair psoriasis from her teens.
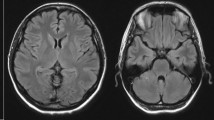
MS diagnosis was made 1 year after an attack of optic neuritis, when the patient had a new relapse (ataxia and vertigo). MRI showed multiple demyelinating brain and spinal lesions and oligoclonal bands were detected at the cerebrospinal fluid examination. She was treated with glatiramer acetate, but switched to IFNB-1b at 29 years of age, because of suboptimal response (persistence of relapses, with mild residual deficit on piramidal system, EDSS 2.0). During this treatment she remained relapse free, without significant side effects, although she noticed a slight increase of hair psoriasis. IFNB-1b was stopped after 2 years for pregnancy wish. She had a child at 31 years of age. In the following years, she refused therapy and had a second child. At 37 years of age, after a new MS relapse, she was treated again with IFNB-1b. After a few months, the patient referred the increase of hair psoriasis and developed pain and swelling of the left third metatarsophalangeal joint with echographic evidence of tenosynovitis. A concomitant neurological worsening (hypoesthesia and hyposthenia of the left leg) was treated with steroids (dexamethasone) with benefit and remission of the arthralgia as well. After 2 months, she developed a further increase in hair psoriasis (Fig. 1a) and pain and swelling of the left fourth metacarpophalangeal and proximal interphalangeal joints (Fig. 2a). Hematological examinations including serum rheumatologic tests were within normal limits. A diagnosis of oligoarticular PsA was made and low-dose prednisone therapy (10 mg/day) given and tapered over 1 year, with slight improvement in arthropathy but not in dermatological lesions. After 1 year, psoriatic lesions occurred also in the leg skin and in the IFNB injection sites. The patient refused to continue IFNB. Few months later, amelioration of psoriasis and PsA occurred (Figs. 1b, 2b). MRI showed an asymptomatic increase of disease burden and azathioprine was begun. After 6 months, the patient was free of arthralgia and hair lesions; neurological examination revealed a slight paraparesis and hypoesthesia of the left leg (EDSS 2.5).
Discussion
This patient was affected by RR MS, responsive to IFNB treatment, which, however, was associated with the exacerbation of pre-existing psoriasis and the development of oligoarticular PsA. The remission of both cutaneous and articular diseases following the cessation of therapy strongly supports a direct role of IFNB therapy.
Exacerbation of cutaneous psoriasis has been already reported in a few MS patients during IFNB treatment. Pustular flare of quiescent psoriasis caused by IFNB-1b has been described by Webster [2] in one case. Munschauer [8] described a similar worsening in a small number of psoriasis patients receiving IFN beta-1a. Navne [7] described two other cases, in one of them psoriasiform injection site lesions persisted 6 years after termination of the IFN treatment. Recently, a new-onset psoriasis has been described in a patient treated with IFNB-1a [9].
The development of polyarthritis may be a rare side effect of IFNB therapy: in two out of three MS patients, a diagnosis of rheumatoid arthritis was made [10, 11]. Bilateral complaints of the main joints resolved after cessation of therapy in two patients [10]. Best at our knowledge, no cases of oligoarticular PsA have been reported.
Psoriasis is a chronic inflammatory skin disorder that affects 2–3% of the Caucasian population. The disease is characterized by thickened scaly skin patches or psoriatic plaques caused by abnormal keratinocyte proliferation and infiltration of inflammatory cells into the dermis and epidermis, in genetically susceptible individuals. Approximately 10–30% of psoriatic patients also develop PsA. Psoriasis may occur in MS patients, although the evidence of the association between the two diseases is uncertain. The frequency of psoriasis is higher in MS patients compared with the general population [3, 4], but similar in comparison with spousal controls (5.8 vs. 5.4%) [5]. No correlation with exacerbation or functional loss have been showed [4], although recently, Ganesvaran [12] has reported a significant association with brainstem and cerebellar involvement and disease severity in susceptible MS patients. Furthermore, psoriasis seems to be the most common autoimmune disorders occurring in MS family members, significantly associated with early onset of MS [6].
Psoriasis and PsA are currently thought as T cell-mediated type 1 diseases [13]. Both psoriatic skin lesions and synovial tissue in PsA are characterized by an infiltrate of adaptive immune cells (CD4+ and CD8+ lymphocytes), innate immune cells (neutrophils, macrophages) and proinflammatory cytokines such as IFN-γ, and TNF-α [14]. Of interest, skin biopsies at the IFNB injection sites have showed strong expression of chemokines such as CXCL10 and CCL2 characterized by chemotactic activity for T cells and macrophages [9]. To be noticed that a large number of IFN-related genes are upregulated in psoriasis, accounting for >5% of total genes with elevated expression in lesions [15]. These observations suggest that IFNB might induce or exacerbate psoriasis and probably PsA in susceptible patients, by stimulating the influx in the skin and modulation of both adaptive and innate immune cells.
On the other hand, it is known that psoriasis patients treated with TNF alpha inhibitors (etanercept, infliximab, adalimumab) have an increased risk of demyelinating disease and these drugs might cause an increased disease activity in MS patients [16–18]. These findings suggest that MS and psoriasis, both T cell-immune-mediated diseases, seem to partially share pathways of immune dysregulation, causing a paradoxical reciprocal activation with disease modifying agents.
In conclusion, this report shows that activation of psoriasis and PsA might be a rare side effect of IFNB therapy, which may be an additional trigger of psoriasis, similar to other exogenous factors, such as rapid withdrawal of immunosuppressive drugs like steroids and systemic infections [13]. The clinicians should carefully evaluate concomitant morbidity in order to allow a patient-oriented treatment strategy and inform patients about possible adverse events of disease modifying agents.
References
Walther EU, Hohlfeld R (1999) Multiple sclerosis side effects of interferon beta therapy and their management. Neurology 53:1622–1627
Webster GF, Knobler RL, Lublin FD, Kramer EM, Hochman LR (1996) Cutaneous ulcerations and pustular psoriasis flare caused by recombinant interferon beta injections in patients with multiple sclerosis. J Am Acad Dermatol 34:365–367
Nielsen NM, Frisch M, Rostgaard K, Wohlfahrt J, Hjalgrim H, Koch-Henriksen N, Melbye M, Westergaard T (2008) Autoimmune diseases in patients with multiple sclerosis and their first-degree relatives: a nationwide cohort study in Denmark. Mult Scler 14:823–829
Cendrowski W (1989) Multiple sclerosis and psoriasis. Wiad Lek 42:575–578
Ramagopalan SV, Dyment DA, Valdar W, Herrera BM, Criscuoli M, Yee IML, Sadovnick AD, Ebers GC (2007) Autoimmune disease in families with multiple sclerosis: a population-based study. Lancet Neurol 6:604–610
Annunziata P, Morana P, Giorgio A, Galeazzi M, Campanella V, Lore’ F, Guarino E (2003) High frequency of psoriasis in relatives is associated with early onset in an Italian multiple sclerosis cohort. Acta Neurol Scand 108:327–331
Navne JE, Hedegaard U, Bygum A (2005) Activation of psoriasis in patients undergoing treatment with interferon-beta. Ugeskr Laeger 167:2903–2904
Munschauer FE, Kinkel RP (1997) Managing side effects of interferon-beta in patients with relapsing–remitting multiple sclerosis. Clin Ther 19:883–893
Lo-Pez-Lerma I, Pranzo P, Herreo C (2009) New-onset psoriasis in a patient treated with interferon beta-1a. Br J Dermatol 160:716–717
Altintas A, Alici Y, Melikoglu M, Siva A (2002) Arthritis during interferon beta-1b treatment in multiple sclerosis. Mult Scler 8:534–536
Alsalameh S, Manger B, Kern P, Kalden J (1998) New onset of rheumatoid arthritis during interferon beta-1b treatment in a patient with multiple sclerosis: comment on the case report by Jabaily and Thompson. Arthritis Rheum 41:754
Ganesvaran G, Greer JM, Pender MP (2009) Prominent brainstem and cerebellar involvement in multiple sclerosis with psoriasis. Mul Scler 15:763–766
Liu Y, Krueger JG, Bowcock AM (2007) Psoriasis: genetic associations and immune system changes. Genes Immun 8:1–12
Krueger JG, Bowcock A (2005) Psoriasis pathophysiology: current concepts of pathogenesis. Ann Rheum Dis 64:30–36
Lew W, Bowcock AM, Krueger JM (2004) Psoriasis vulgaris: cutaneous lymphoid tissue supports T cell activation and type-1 inflammatory gene expression. Trends Immunol 25:295–305
Sukal SA, Nadiminti L, Granstein RD (2006) Etanercept and demyelinating disease in patients with psoriasis. J Am Acad Dermatol 54:160–164
Mohan N, Edwards ET, Cupps TR (2001) Demyelination occurring during anti-tumor necrosis factor alpha therapy for inflammatory arthritides. Arthritis Rheum 44:2862–2869
Bensouda-Grimaldi L, Mulleman D, Valat JP, Autret-Leca E (2007) Adalimumab-associated multiple sclerosis. J Rheumatol 34:239–240
Acknowledgments
We gratefully acknowledge the patient for her valuable collaboration and Mr Mauro to support the study taking photographs of the lesions during the follow-up.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
La Mantia, L., Capsoni, F. Psoriasis during interferon beta treatment for multiple sclerosis. Neurol Sci 31, 337–339 (2010). https://doi.org/10.1007/s10072-009-0184-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-009-0184-x