Abstract
Polyarteritis nodosa is a primary systemic necrotizing vasculitis whose evolution follows, in many cases, a chronic remitting-recurrent course with refractoriness to conventional immunosuppressants. We report here the clinical case of a 75-year-old patient with serologies suggestive of past hepatitis B virus infection who presented a flare of polyarteritis nodosa with great secondary functional impairment. She had not responded to several previous immunosuppressants and required high doses of glucocorticoids to control the flare. After the initiation of biological therapy with tocilizumab, the patient experienced a rapid and marked clinical and analytical improvement, going into clinical remission and being able to remarkably lower the corticosteroid dose and stop the rest of the immunosuppressants. There was no evidence of hepatitis B virus reactivation or changes in the titers of any of the parameters related to the aforementioned infection. This clinical case represents the first case reported in the literature about the successful and safe treatment of polyarteritis nodosa with tocilizumab in a patient with serologies suggestive of past hepatitis B virus infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
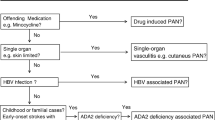
Polyarteritis nodosa (PAN) is defined as a necrotizing arteritis of medium or small arteries that is not associated with glomerulonephritis or with positivity of anti-neutrophil cytoplasmic antibodies (ANCA) [1]. It usually conditions a multi-organ disease in which the most frequent manifestations involve the skin, joints, muscles, and the peripheral nervous and digestive systems, while the lung is not usually affected. Subtypes characterized by involvement of a single organ, or exclusively cutaneous, are also distinguished [2].
Currently, there are no defined clinical guidelines for the treatment of PAN, and the therapeutic regimens used in it are frequently extrapolated from the treatment of ANCA-associated vasculitis (AAV) [3]. Few studies have been carried out with the aim of evaluating the best therapeutic options in PAN, and the vast majority of them focus on the role of systemic glucocorticoids (GC) and cyclophosphamide (CYC) [4, 5]. Cases of cutaneous PAN are usually treated with non-steroidal anti-inflammatory drugs or colchicine and, when refractory, with GC, dapsone, hydroxychloroquine, or other immunosuppressants [6]. In systemic PAN, the choice of treatment depends on the presence of severity criteria, usually defined by a Five Factor Score (FFS) ≥ 1 [4]. Cases lacking severity criteria (FFS = 0) are treated with GC, adding immunosuppressants in refractory cases or as GC sparing agents [7]. In cases with severity criteria (FFS ≥ 1), the combination of GC and CYC is the cornerstone in the induction treatment [4, 5]. In these cases, maintenance of remission is usually achieved with the combination of GC and methotrexate (MTX) or azathioprine (AZA), or in cases of intolerance or contraindications to the latter two, with mycophenolate [8, 9].
More than 50% of patients with PAN not associated with hepatitis B virus (HBV) infection have a relapse despite immunosuppressive treatment [10]. On other occasions, treatment is not well tolerated or needs to be withdrawn due to adverse effects. It is on these cases that bringing in new therapeutic strategies and “off-label” treatments becomes highly relevant in this disease. To date, the use of biological therapies in PAN has not been evaluated through clinical trials and the scientific evidence is based on what has been observed in some reported cases.
There are only a few case reports in the literature about the treatment of PAN with tocilizumab (TCZ) [11,12,13,14,15,16], most of which show favorable results, suggesting the possible role of this molecule in its treatment. The apparent successful use of other biological therapies in PAN, mainly anti-TNFα and rituximab, has also been reported [17, 18].
There are no cases reported to date regarding the safety of treatment with TCZ in patients with PAN and serologies suggestive of past HBV infection, defined as those with a negative surface antigen (HBsAg) and positive antibodies against the core antigen (anti-HBc), accompanied or not, by hepatitis B virus surface antibodies (anti-HBs). In this work, we present the first described case of successful and safe treatment with TCZ of refractory PAN, in a patient with serologies suggestive of past HBV infection. We conducted a review of the literature on the current evidence of PAN treatment with TCZ.
Literature review
We conducted a comprehensive review of the English literature to find data on treatment of PAN with TCZ. The MEDLINE/Pubmed, EMBASE, Scopus, and Web of Science databases were searched combining the following keywords: “polyarteritis nodosa” AND “tocilizumab.” We did not put time limitations regarding the publication dates. Search was conducted in February 2020. We reviewed the abstracts of the relevant studies and retrieved the appropriate articles. Articles cited as references in the identified papers were also reviewed. Pediatric cases were excluded. We identified 6 papers which reported 15 cases of adult patients with PAN treated with TCZ.
Case presentation
We present the case of a 76-year-old patient diagnosed at 70 years, in December 2013, with cutaneous PAN due to livedoid lesions and panniculitis in the lower extremities. A skin biopsy was performed that reported signs of septal fibrosis in the subcutis and inflammatory changes compatible with PAN. In December 2015, the patient presented with myalgia and paresthesia in the lower extremities with a neurophysiological study compatible with sensory axonal polyneuropathy, meeting the 1990 classification criteria for classic PAN of the American College of Rheumatology [19] and the definitions of the International Chapel Hill Consensus Conference of 2012 [1]. Serum detection of anti-proteinase 3 and anti-myeloperoxidase antibodies was negative. The patient also showed positivity for the antibodies of the anti-phospholipid syndrome anti-β2-glycoprotein IgM, confirmed on more than two occasions 12 weeks apart, with the rest of the antibodies of the anti-phospholipid syndrome negative and without meeting Sapporo’s 1999 classificatory criteria given the absence of clinical criteria. A serological study of HBV was performed in which positive total anti-HBc and anti-HBs were observed, the latter at high titers (> 100 IU/L), with negative HBsAg, normal liver function, and undetectable viral load, suggestive of past HBV infection with natural immunity. Given the poor control of the symptoms and the prediction of an intensification in treatment with high doses of GC, the risk of reactivation of HBV was assessed as intermediate, and anti-viral treatment with tenofovir was started.
The patient’s disease was characterized by a chronic relapsing-remitting course, which required maintenance treatment with prednisone combined with various immunosuppressants, the latter detailed in Fig. 1. Since the moment of her diagnosis, the patient had always been treated with GC, requiring high doses in many occasions.
Starting date of the immunosuppressive treatments received by the patient and cause for withdrawal. Glucocorticoid treatment was maintained at varying doses throughout all follow-up. During all the period represented, the patient only presented cutaneous manifestations of the disease in the form of livedoid lesions and panniculitis in the lower extremities. Systemic symptoms started in December 2015
In April 2018, the patient presented a clinical worsening with peripheral neurological progression and increased muscle and neuropathic pain in the lower extremities with great secondary limitation. Likewise, a worsening of livedo reticularis and nodular skin lesions suggestive of panniculitis (Fig. 2) was observed. At that time, the patient was under immunosuppressant treatment with mycophenolic acid 1080 mg/24 h and prednisone 10 mg/day and had abandoned anti-viral prophylactic treatment in January 2017, as the dose of prednisone could have been reduced below 10 mg/24 h. Analytically, she had elevated acute phase reactants—C-reactive protein 8.98 mg/dL (< 0.5 mg/dL)—and anemia, with a hemoglobin of 10 g/dL (> 12 g/dL). In order to study the extension of the disease activity and rule out involvement of other target organs, a brain magnetic resonance imaging was performed. In order to study the extension of the disease activity and rule out involvement of other target organs, a brain magnetic resonance imaging was performed where non-specific nodular T2 hyperintensities were observed, isolated and at the onset of the supratentorial and protuberance white matter confluence. These alterations were considered to be related to either PAN or anti-phospholipid syndrome antibodies. With the intention of controlling the new symptoms, the prednisone dose was increased to 30 mg/24 h. At that time, the Birmingham Vasculitis Activity Score (BVAS) version 3 was 5.
Despite the absence of severity criteria indicated by a 1996 FFS of 0 since the three predominant clinical manifestations of our patient are not included in this index, inflammatory and vasculitic skin involvement, limiting progressive polyneuropathy, and myalgia can lead to serious, chronic disease with high interference from a functional point of view, as occurred in our patient.
Given the lack of clinical response, the severe functional deterioration presented by the patient, and the inability to decrease the high doses of GC in an elderly patient with multiple comorbidities and an important Cushingoid phenotype, it was decided to start biological treatment with intravenous TCZ in September 2018, at a dose of 8 mg/kg/month (600 mg/month). The infusions were well tolerated by the patient. As side effects, the patient presented neutropenia below 1500 total neutrophils and, despite the fact that stopping treatment with TCZ is not indicated until < 1000 neutrophils, it was decided to adopt a more conservative approach and temporarily stop it for 3 months until the neutrophil count recovered.
Currently, the patient has received 11 doses of intravenous TCZ over 14 months with significant clinical and biological improvement, remaining in remission with a BVAS of 0. At this time, the patient is asymptomatic, without myalgia or neuropathic pain in lower extremities and without new skin lesions. Analytically, she presents a normalization of acute phase reactants and an improvement on hemoglobin (Fig. 3). Regarding concomitant medication, it has been possible to stop mycophenolic acid and decrease the prednisone dose to 2.5 mg/day (84% reduction in prednisone dose compared with the dose prior TCZ treatment), with the corresponding improvement in her secondary Cushing’s syndrome (Fig. 4). No reactivation of HBV has been observed, defined as the new detection of serum HBV-DNA (more than 2.0 log copies/ml to more than 3.0 log copies/ml) in a patient with a previously undetectable viral load, positivization of HBsAg, or the increase in alanine aminotransferase (ALT) values> 2 times the upper value of normality in two consecutive determinations.
Changes in ESR (erythrocyte sedimentation rate), CRP (C-reactive protein), and ANC (absolute neutrophil count) values before and after starting tocilizumab. The dark solid vertical line indicates the starting time of the first dose of tocilizumab; the dark dashed vertical line, the time when stopped by neutropenia; and the third dark solid vertical line, when it was resumed 3 months after the recovery of the neutrophil count
Discussion
The use and efficacy of biological therapies in PAN has not been evaluated through clinical trials and the current scientific evidence is based on what has been reported as off-label therapy in some case reports.
According to Nakahama et al., serum IL-6 levels are correlated with the activity of PAN and can be used in its diagnosis and monitoring. So, the inhibition of IL-6 seems to have a potential relevant role in the control of this disease [20]. TCZ, a humanized recombinant monoclonal IgG1 antibody anti-human interleukin-6 (IL-6) receptor, has shown encouraging preliminary results regarding its efficacy in multiple immunomediated diseases in whose physiology the dysregulation of IL-6 is clearly involved [21, 22].
Regarding the use of TCZ for the treatment of PAN specifically, Krusche et al. conducted an exhaustive review of the literature in 2018 [15], detailing the demographics, clinical characteristics, and response to TCZ of the case reports in the matter published to date [12,13,14,15,16]. We have reviewed the literature in order to detect cases of PAN adult patients treated with TCZ, published after Krusche’s review, while at the same time, we report a new case. Our clinical case represents the first case of PAN treated with TCZ in a patient with serologies suggestive of past HBV infection, since in all previously reported cases the patients had intentionally negative serologies.
Recently, Bodoki et al. reported the successful use of TCZ in combination with MTX and GC in an adult male who did not respond to initial treatment with CYC and GC. He presented with multisystemic symptoms consisting of constitutional symptoms, myalgia, polyneuropathy, and digestive and neurological symptoms, and showed angiographic brain and abdominal abnormalities, After the administration of TCZ, the patient went into clinical remission, with normalization of the analytical parameters and improvement of the cerebral angiographic lesions [11].
Regarding the use of TCZ in patients with serologies suggestive of past HBV infection, we found some controversy in the literature about the risk of HBV reactivation in these patients. In a systematic review carried out in 2015 on patients predominantly affected by rheumatoid arthritis with past HBV infection, it was found that 8.6% of patients treated with TCZ experienced HBV reactivation [23]. However later, Ahn et al. did not observe any case of HBV reactivation 3 months after starting treatment with TCZ in 15 anti-HBc positive patients, who had not received anti-viral prophylaxis. Moreover, they did not find any changes in the titers of HBsAg, anti-HBc, or anti-HBs after treatment with said drug [24]. Along the same line, Papalopoulos et al. evaluated the risk of HBV reactivation in 30 patients with rheumatoid arthritis treated with TCZ who had antibodies suggestive of HBV past infection (anti-HBc+, anti-HBc±), of whom only 2 had received prophylactic anti-viral treatment. No case of HBV reactivation was observed, although anti-HBs titers fell below the level of immune protection (< 10 mIU/ml) in one patient [25]. Nevertheless, it seems that the safety of TCZ treatment in patients with past HBV infection has been evaluated, in its entirety, in patients affected by rheumatoid arthritis, and there are no cases reported to date regarding the safety of TCZ treatment in anti-HBc positive patients with PAN.
In conclusion, the results of our clinical case are in the same line as that published to date on the efficacy of TCZ in PAN, as well as with what has been reported about the safety of TCZ in patients with past HBV infection in other rheumatologic diseases [24, 25]. Our observations seem to indicate that TCZ could be highly effective in treating PAN, controlling disease activity and acting as a GC sparing agent, allowing a marked reduction in the dose of GC and other immunosuppressants. Likewise, it seems that PAN treatment with TCZ is safe in patients with anti-HBc positive, HBsAg-negative, and anti-HBs positive at high titers, and that it would not cause a reactivation of the HBV, nor a decrease in anti-HBs titers, contrarily to what has been debated with other biologics [25].
Therefore, despite the need for future prospective studies to confirm our observations, TCZ could be an effective alternative in the treatment of active PAN refractory to other immunosuppressants in patients with past HBV infection and should be considered within the therapeutic options when evaluating this group of patients.
References
Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, Flores-Suarez LF, Gross WL, Guillevin L, Hagen EC, Hoffman GS, Jayne DR, Kallenberg CGM, Lamprecht P, Langford CA, Luqmani RA, Mahr AD, Matteson EL, Merkel PA, Ozen S, Pusey CD, Rasmussen N, Rees AJ, Scott DGI, Specks U, Stone JH, Takahashi K, Watts RA (2013) 2012 Revised International Chapel Hill consensus conference nomenclature of vasculitides. Arthritis Rheum 65:1–11
De Virgilio A, Greco A, Magliulo G et al (2016) Polyarteritis nodosa: a contemporary overview. Autoimmun Rev 15:564–570
Yates M, Watts RA, Bajema IM, Cid MC, Crestani B, Hauser T, Hellmich B, Holle JU, Laudien M, Little MA, Luqmani RA, Mahr A, Merkel PA, Mills J, Mooney J, Segelmark M, Tesar V, Westman K, Vaglio A, Yalçındağ N, Jayne DR, Mukhtyar C (2016) EULAR/ERA-EDTA recommendations for the management of ANCA-associated vasculitis. Ann Rheum Dis 75:1583–1594
Guillevin L, Lhote F, Gayraud M, Cohen P, Jarrousse B, Lortholary O, Thibult N, Casassus P (1996) Prognostic factors in polyarteritis nodosa and Churg-Strauss syndrome: a prospective study in 342 patients. Medicine (Baltimore) 75:17–28
Gayraud M, Guillevin L, Cohen P et al (1997) Treatment of good-prognosis polyarteritis nodosa and Churg-Strauss syndrome: comparison of steroids and oral or pulse cyclophosphamide in 25 patients. Br J Rheumatol 36:1290–1297
De Menthon M, Mahr A (2011) Treating polyarteritis nodosa: current state of the art. Clin Exp Rheumatol 29:S100–S116
Ribi C, Cohen P, Pagnoux C, Mahr A, Arène JP, Puéchal X, Carli P, Kyndt X, le Hello C, Letellier P, Cordier JF, Guillevin L, French Vasculitis Study Group (2010) Treatment of polyarteritis nodosa and microscopic polyangiitis without poor-prognosis factors a prospective randomized study of one hundred twenty-four patients. Arthritis Rheum 62:1186–1197
Pagnoux C, Mahr A, Hamidou MA, Boffa JJ, Ruivard M, Ducroix JP, Kyndt X, Lifermann F, Papo T, Lambert M, le Noach J, Khellaf M, Merrien D, Puéchal X, Vinzio S, Cohen P, Mouthon L, Cordier JF, Guillevin L, French Vasculitis Study Group (2008) Azathioprine or methotrexate maintenance for ANCA-associated vasculitis. N Engl J Med 359:2790–2803
Hiemstra TF, Walsh M, Mahr A, Savage CO, de Groot K, Harper L, Hauser T, Neumann I, Tesar V, Wissing KM, Pagnoux C, Schmitt W, Jayne DRW, European Vasculitis Study Group (EUVAS) (2010) Mycophenolate mofetil vs azathioprine for remission maintenance in antineutrophil cytoplasmic antibody-associated vasculitis: a randomized controlled trial. JAMA - J Am Med Assoc 304:2381–2388
Samson M, Puéchal X, Devilliers H, Ribi C, Cohen P, Bienvenu B, Ruivard M, Terrier B, Pagnoux C, Mouthon L, Guillevin L, French Vasculitis Study Group (FVSG) (2014) Long-term follow-up of a randomized trial on 118 patients with polyarteritis nodosa or microscopic polyangiitis without poor-prognosis factors. Autoimmun Rev 13:197–205
Bodoki L, Végh E, Szekanecz Z, Szűcs G (2019) Tocilizumab treatment in polyarteritis nodosa. Isr Med Assoc J 21:560–562
Ostrovršnik J, Hočevar A, Lestan B, Sodin Šemrl S, Lakota K, Tomšič M (2016) Long-term follow-up on tocilizumab treatment of AA amyloidosis secondary to polyarteritis nodosa. Amyloid 23:260–261
Saunier A, Issa N, Vandenhende MA, Morlat P, Doutre MS, Bonnet F (2017) Treatment of polyarteritis nodosa with tocilizumab: a new therapeutic approach? RMD Open 3:e000446
Watanabe K, Rajderkar DA, Modica RF (2016) A case of polyarteritis nodosa associated with vertebral artery vasculitis treated successfully with tocilizumab and cyclophosphamide. Case Rep Pediatr
Krusche M, Ruffer N, Kötter I (2019) Tocilizumab treatment in refractory polyarteritis nodosa: a case report and review of the literature. Rheumatol Int 39:337–344
Hočevar A, Lestan B, Sodin Šemrl S, Lakota K, Kojc N, Potočnik N, Tomšič M (2013) AA amyloidosis in a polyarteritis nodosa patient treated with tocilizumab. Amyloid 20:275–276
Ginsberg S, Rosner I, Slobodin G, Rozenbaum M, Kaly L, Jiries N, Boulman N, Awisat A, Hussein H, Novofastovski I, Silawy A, Rimar D (2019) Infliximab for the treatment of refractory polyarteritis nodosa. Clin Rheumatol 38:2825–2833
Seri Y, Shoda H, Hanata N, Nagafuchi Y, Sumitomo S, Fujio K, Yamamoto K (2017) A case of refractory polyarteritis nodosa successfully treated with rituximab. Mod Rheumatol 27:696–698
Lightfoot Jr, Robert W et al (1990) The American College of Rheumatology 1990 criteria for the classification of polyarteritis nodosa. Arthritis Rheum 33:1088–1093
Nakahama H, Okada M, Miyazaki M et al (1993) Distinct responses of interleukin-6 and other laboratory parameters to treatment in a patient with polyarteritis nodosa—a case report. Angiology 32:189–192
Rubbert-Roth A, Furst DE, Nebesky JM, Jin A, Berber E (2018) A review of recent advances using tocilizumab in the treatment of rheumatic diseases. Rheumatol Ther 5:21–42
Tanaka T, Kishimoto T (2012) Targeting interleukin-6: all the way to treat autoimmune and inflammatory diseases. Int J Biol Sci 8:1227–1236
Mori S, Fujiyama S (2015) Hepatitis B virus reactivation associated with antirheumatic therapy: risk and prophylaxis recommendations. World J Gastroenterol 21:10274–10289
Ahn SS, Jung SM, Song JJ, Park YB, Park JY, Lee SW (2018) Safety of tocilizumab in rheumatoid arthritis patients with resolved hepatitis B virus infection: data from real-world experience. Yonsei Med J 59:452–456
Papalopoulos I, Fanouriakis A, Kougkas N, Flouri I, Sourvinos G, Bertsias G, Repa A, Avgoustidis N, Sidiropoulos P (2018) Liver safety of non-tumour necrosis factor inhibitors in rheumatic patients with past hepatitis B virus infection: an observational, controlled, long-term study. Clin Exp Rheumatol 36:102–109
Acknowledgments
We gratefully thank Dr. Gustavo Deza Vargas for providing us with pictures of the cutaneous lesions of the patient and collaborating in the patient’s clinical management.
Author information
Authors and Affiliations
Contributions
All authors approved the final manuscript as submitted, and accepted responsibility for all aspects of the work.
Corresponding author
Ethics declarations
Disclosures
None.
Informed consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Carrión-Barberà, I., Pros, A., Salman-Monte, T.C. et al. Safe and successful treatment of refractory polyarteritis nodosa with tocilizumab in a patient with past hepatitis B virus infection: a case-based review. Clin Rheumatol 40, 2065–2070 (2021). https://doi.org/10.1007/s10067-020-05345-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05345-4