Abstract
Objectives
To determine the prevalence of depression and its determinants among Nigerian patients with knee osteoarthritis (OA).
Methods
Two hundred and fifty patients satisfying the American College of Rheumatology classification criteria for knee OA were recruited from five centers. Pain was assessed using Western Ontario and McMaster Universities Index (WOMAC) pain subscale, functional status was determined by Steinbrokers criteria, radiographic knee OA was graded using Kellgren–Lawrence criteria, depression was determined using the Patient Health Questionnaire (PHQ-9), sleep quality by the Pittsburgh Sleep Quality Index (PSQI), and family functioning by Family APGAR (Adaptation, Partnership, Growth, Affection, and Resolve). Factors associated with depression in KOA following bivariate analyses were adopted as independent variables in logistic regression analysis to determine the predictors of depression in KOA. The study was approved by the Ethical Review Committee of each of the study centers.
Results
The mean age of patients was 59.90 ± 10.62 years and 209 (83.6%) were females. Their mean PHQ-9 score was 4.68 ± 4.19 with 105 (42%) having depression (PHQ-9 ≥ 5). Eighty-four (80%) of patients with depression had poor sleep quality (PSQI≥ 5.0). Depression was significantly associated with poor sleep, WOMAC pain scores, medial compartment KOA, lateral compartment KOA, and patellofemoral OA. Poor sleep quality was the best predictor of depression (OR 4.555, CI (2.241–9.257), p < 0.001) followed by moderate to severe pain (OR 2.490, CI (1.119–5.542), p < 0.025).
Conclusion
Depression is common among patients with knee OA, and depression can be predicted by poor sleep quality and moderate to severe pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Musculoskeletal disorders are a major contributor to the burden of disease across the world accounting for up to 6.8% of the worldwide disability-adjusted life years (DALY); Osteoarthritis (OA) represents the single most important musculoskeletal disorder [1]. Clinically, OA is characterized by mechanical joint pains, stiffness, crepitus, progressive limitation of movement, and variable amounts of joint effusion [2]. Constant, poorly remitting pain is often seen in the late stages of the disease [3]. In addition, worsening destruction of the joint architecture and loss of articular cartilage lead to joint deformities and instability with an increased risk of falls, decline in levels of physical functioning, and compounding psychosocial problems such as depression [4]. Consequently, an emerging insight into the role of both biological and psychosocial factors in the assessment and management of OA has been birthed [3].
Depression affects one-fifth of individuals with knee OA and is twice as common as in the general population [4]. The prevalence of depression among knee OA patient is variable and ranges between 19.16 and 39% [5, 6]. Odole et al [7] reported a frequency of 28.8% among 80 patients with knee OA seen at Ibadan, Nigeria.
Patients with OA and depression are less likely to cope well and may report higher levels of pain and overall OA-associated symptoms [3, 7]. The relationships between depression and pain are reciprocal and complex, with each predicting and worsening the outcome of the other [8]. The effect of depressive symptoms in the reduction of physical activity, which in turn, leads to worsening of pain and disability is increasingly being recognized [9]. Similarly, complex interactions have been suggested in the pervasiveness and severity of depressive symptoms among OA patients living with poor daily sleep quality or in a dysfunctional family setting. Wang et al reported a higher rate of poor family functioning among patients with depression, and they observed that there is good agreement between the self-report of the family members and the documentation of a trained evaluator about the family impairments in these subjects [10]. High-impact recommendations drafted by the European League Against Rheumatism (EULAR) and the American College of Rheumatology (ACR) on the treatment guidelines for OA recognizes that depression contributes to the weight of morbidity, and central pain perception is adversely affected in the patient with depression [11].
There are no multicenter studies on depression among knee OA patients in Nigeria and Africa. The objective of this study is to determine the prevalence of depression, the levels of family functioning, and the predictors of depression among patients with knee OA in a multicentral setting.
Methodology
Study design
This is a multicentral, hospital-based cross-sectional study conducted in the Rheumatology and General Out-Patient Department (GOPD) clinics of five tertiary institutions in Nigeria (University of Maiduguri Teaching Hospital, University of Jos Teaching Hospital, University of Ilorin Teaching Hospital, Lagos State University Teaching Hospital, and University of Uyo Teaching Hospital) spread across the northern, middle, and southern part of the country.
Study population
Individuals aged 18 years and above, satisfying the American College of Rheumatology (ACR) clinical classification criteria for knee OA [12] were recruited over a period of 3 months. Consenting patients aged 18 and older who satisfied the ACR clinical classification criteria for knee OA served as inclusion criteria. Patients with a history of previous knee surgery, known mental illness, inflammatory arthritis, systemic infection, or malignancy and other symptomatic chronic diseases e.g., diabetes mellitus, chronic liver disease, and chronic obstructive lung disease were excluded from the study.
Sample size determination
Sample size was obtained using Fisher’s statistical formula for estimating the minimum sample size in descriptive health studies when population size is greater than 10,000 [13]. Based on the reported knee OA prevalence of 11.5% determined by Adebusoye et al in Ibadan, Nigeri [14], the calculated sample size for the study was estimated to be 156. However, to increase the power of the study, we recruited a total of 250 patients at a rate of 50 patients per center.
Sampling method
Patients were recruited using a systematic random sampling method in which every other patient with knee OA were recruited. A prior communication with the coinvestigators representing each of the participating hospitals revealed that a median of 100 patients with knee OA was seen over a period of 3 months. With a recruitment plan of 50 participants per center, a sampling interval of two was chosen. The first patient seen each day meeting the inclusion criteria for the study was chosen followed by the third patient and so on. If an individual does not satisfy the inclusion criteria, or the person refused to participate, the next individual was recruited. Patients’ folders were labeled, and a research register was kept to avoid double sampling. The procedure was repeated each day until the sample size was attained.
Data collection
An informed verbal and written consent was obtained from all participants while a semi-structured interviewer questionnaire was administered to collect demographic and relevant clinical information. Pain severity was assessed using a 0–10 numerical rating scale (NRS), with 0 being no pain, while 10 is the maximum pain experienced. A score of 4 or less was considered mild pain, 5–7 as moderate, and 8 and above as severe pain. The Western Ontario and McMaster Universities index (WOMAC) (Likert) pain subscale was also used to grade pain intensity. We considered cutoff points of less than 5, 6–10, and 11–20 as mild, moderate, and severe pain respectively. Individuals were grouped into four functional classes using the Steinbrocker functional classification [15]. Each knee was examined separately for the presence or absence of deformities, effusion, joint line tenderness, and crepitus. The range of motion (ROM) and alignment of the knee joint were measured using an International Standard Goniometer. Quadriceps strength was graded using the Medical Research Council grading scale.
The weight to the nearest 0.01 kg and height to the nearest 0. 01 m were measured using a Seca electronic weighing/height scale (Seca Deutschland, Hamburg, Germany) using standard techniques. Body mass index (BMI) was calculated using the formula, weight (kg)/height2 (m2). For the purpose of our analysis, we dichotomized patients as not obese (BMI < 30 kg/m2) or obese (BMI ≥ 30.0 kg/m2).
Blood pressure (BP) was measured with a mercury sphygmomanometer (Accosson, England) using standard techniques [16].
Standard anteroposterior (AP) and lateral semi-flexed radiographs of knees in weight bearing position were taken by qualified radiographers of the radiology department of the hospitals. The radiographs were interpreted and graded by both the radiologists and the principal investigators using the Kellgren and Lawrence criteria [17]. The radiographs are graded after the two have agreed on a particular KL grade. The higher KL grade of the two knees was used in the final analysis.
Depression was assessed using the Patient Health Questionnaire (PHQ-9) [18]. It has a minimum score of 0 and maximum score of 27. Component scores are rated 0 to 3. The interpretation of the total scores is as follows: 0–4 = no depression; 5–9 = mild depression; 10–14 = moderate depression; 15–19 = moderately severe depression; 20–27 = severe depression. It has been validated for use in Nigeria, having a good concurrent validity with Beck’s depression inventory (BDI) (r = 0.84, p < 0.001) and good 1 month test-retest reliability (r = 0.84, p < 0.001) [19]. The sensitivity and specificity with 5 as cutoff score for minor depressive disorder is 0.989 and 0.973 respectively, and 0.846 and 0.994 respectively with 10 as cutoff for major depression [19]. PHQ-9 has also been shown to be a valid and reliable tool for assessing depressive disorders and depression severity among patients with knee OA [20]. We dichotomized patients into two groups, PHQ-9 < 5 (no depression) and PHQ-9 ≥ 5 (has depression).
The sleep quality of respondents was assessed using the Pittsburgh Sleep Quality Index (PSQI) [21]. The 19-item questionnaire generates seven components: sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medications and daytime dysfunction. The global score ranges from 0 to 21, and a higher score is indicative of a poorer subjective sleep quality. PSQI has been validated in Nigeria by Aloba et al. with the best cutoff score set at 5 [22]. We dichotomized patients into two groups scores less than 5 (no sleep abnormality) and score ≥ 5 (poor sleep quality).
Family functioning was assessed by the Family APGAR (Adaptation, Partnership, Growth, Affection, and Resolve) questionnaire. The measure consists of five parameters of family function: Adaptability, Partnership, Growth, Affection, and Resolve. The instrument has a minimum score of 0 and a maximum score of 10. Family APGAR’s scores are interpreted as follows: 7–10 = highly functional family; 4–6 = moderately dysfunctional family; 0–3 = severely dysfunctional family. The correlation of the instrument with the previously validated instrument (Pless–Satherwhite index) is 0.80, and the correlation with clinical report is 0.64 [23]. The Family APGAR has been validated and used for previous studies in Nigeria [24].
Data analysis
All data obtained were analyzed using statistical package for social science, IBM SPSS statistics® 2012 version 21.0 for windows by IBM USA, Armonk, NY, 10504. Demographic and clinical data were summarized using frequencies, percentages, and proportions. Test of normality was performed using Shapiro–Wilk statistics. Means of normally distributed continuous variables of participant with depression and those without depression were compared using T test, while the median of skewed variables was compared using Mann–Whitney U test. Test of association between depression and each of the determinants under consideration (KL grades, functional status, sleep quality, family functioning) were done using chi square test. Fisher’s exact was used where frequencies are less than 5. Predictors of depression in patients with knee OA were determined using multiple logistic regression analysis with PHQ-9 score < 5 and ≥ 5 as a binary outcome, after controlling for age and sex. A P value < 0.05 was considered statistically significant for all tests.
Ethical considerations
The study was approved by the Ethical Review Committee of each of the study centers.
Results
Demographics
The 250 participants had a mean age of 59.90 ± 10.62 years. One hundred and sixty-four (65.6%) were 65 years or older. They comprised of 209 (83.6%) females and 41(16.4%) males. There was no significant difference in their mean ages (p = 0.937). Majority (74.4%) had one form of education, 185 (74%) were married, 66 (26.4%) were unemployed, and 179 (71.6%) of the females were postmenopausal. Table 1 shows the socio-demographic distribution of the patients.
Clinical features
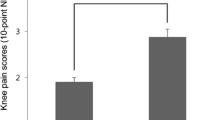
One hundred and sixty-five (66%) participants had bilateral knee involvement; 44 (17.4%) and 41(16.4%) had unilateral right and left knee involvement respectively. The median duration of knee pain reported by all participants was 48 months (range 1–600). The total mean pain score was 8.83 ± 3.836 using WOMAC, indicating, on average that participants had moderate pain intensity at presentation. Crackling noise in the knee was the commonest symptom (73.2%) and 130 (52%) were in functional class II. Family history of knee OA was reported by 132 (52.8%) of the participants. Tables 2 and 3 show the clinical and radiographic features of the participants respectively.
Frequency of depression, sleep quality and family function
The mean PHQ-9 score of all participants was 4.68 ± 4.195, indicating, on average that most patients were not depressed when a cutoff point of ≥ 5 was used. One hundred and five (42%) had a PHQ-9 score of ≥ 5, while 26 (10.4%) had PHQ-9 score ≥ 10 (moderate to severe depression). Table 3 shows the distribution of participants across various grades of depression. There was no association between depression and gender (p = 0.302), BMI (p = 0.189), and functional class (p = 0.748). Participants with depression (PHQ-9 score ≥ 5) did not differ significantly in terms of age, proportion of males to females, BMI, duration of knee pain, and APGAR score; however, they have higher median PSQI score (p < 0.0001) and higher NRS and WOMAC pain scores (p = 0.005 and p < 0.0001 respectively) when compared with the participants without depression (Table 4).
The mean PSQI score for all participants was 6.46 ± 4.596. One hundred and five (56.4%) of them had score of ≥ 5, indicating poor sleep quality. Eighty-four (80%) of the participants with depression had poor sleep quality (PSQI median score = 9.0) and differed significantly from those without depression (p < 0.0001).
The mean APGAR score was 8.09 ± 2.23. One hundred and ninety-nine (79.6%) participants had APGAR scores of 7–10 indicative of a highly functional family with only 11(4.4%) having a severely dysfunctional family. There was no association between gender of the participants and categories of APGAR score (p = 0.093).
Radiographic findings of participants with depression and those without depression
Depression was not associated with the severity of KL grades of the participants (p = 0.698); however, there was significant association between depression and the compartments affected (Table 5). The proportion of patients with medial, lateral, and patellofemoral involvement was higher in those with depression than those without depression (p = 0.012, p = 0.005, and p = 0.007 respectively).
Predictors of depression
Multiple logistic regression analysis revealed poor sleep quality with cutoff of PSQI ≥ 5 as the best predictor of depression (OR 4.555, CI (2.241–9.257), p < 0.001). Individuals with PSQI score ≥ 5 were 4.6 times more likely to be depressed than those with good sleep quality. Moderate to severe pain as categorized using WOMAC pain subscale also predicted depression among the participants (OR 2.490, CI (1.119–5.542), p < 0.025). However, no individual knee compartment OA predicted depression (Tables 6 and 7).
Discussion
Depression is common among our participants, and it is associated with pain, poor sleep quality, and patellofemoral radiographic OA. There was no association between depression and age, gender, BMI, duration of symptoms, family function and functional status of our patients, in spite of previous reports. [25] The best predictors of depression in our participants were poor sleep quality and pain.
Our results revealed the frequency of depression to be 42.0% among patients with knee OA when a PHQ-9 cutoff of ≥ 5 was used to defined depression with only 10.4% having moderate to severe depression. Though, higher than the 19.9–23% reported from a systematic review by Stubbs et al [5], some studies have reported higher frequencies of up 52% among patients with knee OA [26]. Axford et al [27] reported a frequency of 40.7% after evaluating 54 patients with lower limb OA. This variation in frequency may be explained by differences in methodology, depression assessment tools used, patient heterogeneity, and type of OA in question.
The age and gender distributions of our participants were similar to that seen in earlier reports [5, 25, 26]. We found no association between depression and age, however, Gignac et al, [28] reported that individuals with mean age of 50.8 years with OA reported more depression compared to elderly subjects having similar OA severity. They attributed the difference to role limitation and dissatisfaction among middle-aged OA individuals. Regarding gender, Rosemann et al. [25] reported a similar frequency of depression between males and females (19.76% of males and 19.16% of females, PHQ-9 ≥ 15). We found a frequency of 34.1% in males and 43.5% in females (with PHQ ≥ 5) and 7.3% of males and 11.4% of females (with PHQ ≥ 10). There was no statistical difference in proportion of males and females with depression using both cutoffs (p = 0.055 and p = 0.308 respectively). Body mass index (BMI), being one of the major risk factors for incidence and progression of knee OA, is commonly associated with OA severity, pain, and limitation of activity [25, 29]; however, an intuitive association with depression was not established in this study.
Our participants had good family relationships reflected by the high number of participants (81.9%) with the APGAR score between 7 and 10. In contrast, Wang et al. reported a higher rate of poor family functioning among patients with depression, and they observed that there is good agreement between the self-report of the family members and the documentation of a trained evaluator about the family impairments in their subjects [11]. This difference may be explained by the fact that the African cultural setting provides care for ill elderly patients by children and other extended family members compared to what is obtained in western countries where they are often catered for in nursing homes.
Osteoarthritis has long been documented to be associated with sleep abnormalities, with OA patients having intermitted sleep, restlessness, and insomnia [30]. A recent study from Korea showed that the prevalence of OA was lowest in the participants who had 6–7 h of sleep and progressively increased with shorter sleep time [31]. It has also been suggested that the amount of improvement in sleep disturbance may serve as an indicator of assessing response to treatment of OA [30]. Taylor et al [32] in a report of 300 patients with knee OA found that 53% had insomnia similar to what we found. Strikingly, 80% of those with sleep abnormality in our study were depressed, further elucidating that.
We found no association between depression and radiographic grades of the knee. However, patellofemoral OA showed an association but failed to independently predict depression among our patients. Studies have shown that patellofemoral knee OA is common, predicts progression to structural damage, and is associated with pain and disability when compared with tibiofemoral knee OA (OR 2.25, p = 0.005) [33]. Poor sleep quality turned out to be the best predictor of depression seen in our study even after excluding factors like pain and age, similar to previous reports [25]. The relationship between sleep and pain might explain why pain, too, is an independent predictor of depression. Both are associated with poor quality of life, anxiety, and general feeling of lack of well-being.
The cross-sectional nature of the study allowed us to only assess information within the period of the study, and depression being a chronic illness that fluctuates might be missed in some patients. Participants were also not followed up to see if time-dependent changes in KL grades will be accompanied by concomitant changes in the psychosocial statuses.
In conclusion, depression is common among our patients with knee OA, and it can be predicted by poor sleep quality and moderate to severe pain.
Considering the complex association of pain, sleep abnormality, and radiographic findings, there is a need to carry out more studies to further understand the relationship and to improve the management of patients with knee OA and depression.
References
Lourenço S, Lucas R, Araújo F, Bogas M, Santos RA, Barros H (2014) Osteoarthritis medical labelling and health-related quality of life in the general population. Health Qual Life Outcomes 12
Pereira D, Ramos E, Branco J (2015) Osteoarthritis. Acta Medica Port 28:99–106
Rathbun AM, Yau MS, Shardell M, Stuart EA, Hochberg MC (2017) Depressive symptoms and structural disease progression in knee osteoarthritis: data from the osteoarthritis initiative. Clin Rheumatol 36:155–163
Sharma L (2016) Osteoarthritis year in review 2015: clinical. Osteoarthr Cartil 24:36–48
Stubbs B, Aluko Y, Myint PK, Smith TO (2016) Prevalence of depressive symptoms and anxiety in osteoarthritis: a systematic review and meta-analysis. Age Ageing 45:228–235. https://doi.org/10.1093/ageing/afw001
Wong LY, Yiu RL, Chiu CK, Lee WK, Lee YL et al (2015) Prevalence of psychiatric morbidity in Chinese subjects with knee osteoarthritis in a Hong Kong orthopaedic clinic. East Asian Arch Psychiatry 25(4):150–158
Odole AC, Ogunlana MO, Adegoke BOA, Ojonima F, Useh U (2015) Depression, pain and physical function in patients with osteoarthritis of the knee: implications for interprofessional care. Nigerian J Med Rehabil 18(1):1–16 Available at http://www.njmr.org.ng. Accessed 18 Jan 2019
Tan V, Jinks C, Chew-Graham C, Healey EL, Mallen C (2015) The triple whammy anxiety depression and osteoarthritis in long-term conditions. BMC Fam Pract 16:163
Stubbs B, Hurley M, Smith T (2015) What are the factors that influence physical activity participation in adults with knee and hip osteoarthritis? A systematic review of physical activity correlates. Clin Rehabil 29:80–94
Wang J, Mansfield AK, Zhao X, Keitner G (2013) Family functioning in depressed and non-clinical control families. Int J Soc Psychiatry 59:561–569
Conaghan PG, Kloppenburg M, Schett G, Bijlsma JW (2014) Osteoarthritis research priorities: a report from a eular ad hoc expert committee. Ann Rheum Dis 73:1442–1445
Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, Christy W, Cooke TD, Greenwald R, Hochberg M, Howell D, Kaplan D, Koopman W, Longley S, Mankin H, McShane DJ, Medsger T, Meenan R, Mikkelsen W, Moskowitz R, Murphy W, Rothschild B, Segal M, Sokoloff L, Wolfe F (1986) Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and therapeutic criteria Committee of the American Rheumatism Association. Arthritis Rheum 29:1039–1049
Wang D, Bakhai A, Del Buono A, Maffulli N (2013) Sample size determination for clinical research. MLTJ Muscles, Ligaments Tendons J 3:116–117
Adebusoye LA, Ogunbode AM, Alonge TO (2013) Magnitude of knee osteoarthritis and associated risk factors among adult patients presenting in a family practice clinic in Nigeria. J Med Tropics 15:144
Hochberg MC, Chang RW, Dwosh I, Lindsey S, Pincus T, Wolfe F (1992) The American College of Rheumatology 1991 revised criteria for the classification of global functional status in rheumatoid arthritis. Arthritis Rheum 35:498–502
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL et al (2003) The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. JAMA 289:412–419
Yoshida K, Barr RJ, Galea-Soler S, Aspden RM, Reid DM, Gregory JS (2015) Reproducibility and diagnostic accuracy of Kellgren-Lawrence grading for osteoarthritis using radiographs and dual-energy x-ray absorptiometry images. J Clin Densitom 18:239–244
Kroenke K, Spitzer RL, Williams JB (2001) The phq-9. J Gen Intern Med 16:606–613
Adewuya AO, Ola BA, Afolabi OO (2006) Validity of the patient health questionnaire (phq-9) as a screening tool for depression amongst Nigerian university students. J Affect Disord 96:89–93
Rosemann T, Backenstrass M, Joest K, Rosemann A, Szecsenyi J, Laux G (2007) Predictors of depression in a sample of 1,021 primary care patients with osteoarthritis. Arthritis Rheum 57:415–422
Buysee D, Reynolds C, Monk T, Berman S, Kupfer D (1989) The Pittsburgh sleep quality index: a new instrument for psychiatry practice and research. Psychiatry Res 28:198–213
Aloba O, Adewuya A, Ola B, Mapayi B (2007) Validity of the Pittsburgh sleep quality index (psqi) among nigerian university students. Sleep Med 8:266–270
Smilkstein G, Ashworth C, Montano D (1982) Validity and reliability of the family apgar as a test of family function. J Fam Pract
Muyibi AS, Ajayi I-OO, Irabor AE, Ladipo MM (2010) Relationship between adolescents' family function with socio-demographic characteristics and behaviour risk factors in a primary care facility. Afr J Prim Health Care Fam
Rosemann T, Backenstrass M, Joest K, Rosemann A, Szecsenyi J, Laux G (2007) Predictors of depression in a sample of 1,021 primary care patients with osteoarthritis. Arthritis Rheum 57(3):415–422
Marks R (2007) Physical and psychological correlates of disability among a cohort of individuals with knee osteoarthritis. Can J Aging 26(4):367–377
Axford J, Butt A, Heron C, Hammond J, Morgan J, Alavi A, Bolton J, Bland M (2010) Prevalence of anxiety and depression in osteoarthritis: use of the Hospital Anxiety and Depression Scale as a screening tool. Clin Rheumatol 29:1277–1283. https://doi.org/10.1007/s10067-010-1547-7
Gignac MA, Backman CL, Davis AM, Lacaille D, Cao X, Badley EM (2013) Social role participation and the life course in healthy adults and individuals with osteoarthritis: are we overlooking the impact on the middle-aged? Soc Sci Med 81:87–93
Zheng H, Chen C (2015) Body mass index and risk of knee osteoarthritis: systematic review and meta-analysis of prospective studies. BMJ Open 5(12):e007568. https://doi.org/10.1136/bmjopen-2014-007568
Leigh TJ, Bird HA, Hindmarch I, Wright V (1988) Measurement of nocturnal motility: behaviour of osteoarthritic patients and controls. Rheumatol Intl 8:67–70
Jung JH, Seok H, Choi SJ, Bae J, Lee SH, Lee MH, Kim JH, Song GG (2018) The association between osteoarthritis and sleep duration in Koreans: a nationwide cross-sectional observational study. Clin Rheumatol 37(6):1653–1659. https://doi.org/10.1007/s10067-018-4040-3
Taylor SS, Hughes JM, Coffman CJ, Jeffreys AS, Ulmer CS, Oddone EZ, Bosworth HB, Yancy WS Jr, Allen KD (2018) Prevalence of and characteristics associated with insomnia and obstructive sleep apnea among veterans with knee and hip osteoarthritis. BMC Musculoskelet Disord 19(1):79. https://doi.org/10.1186/s12891-018-1993
Hinman RS, Crossley KM (2007) Patellofemoral joint osteoarthritis: an important subgroup of knee osteoarthritis. Rheumatology 46:1057–1062
Acknowledgements
We are grateful to the radiographers and radiologists that took and interpret the radiographs of the participants.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the Ethical Review Committee of each of the study centers.
Disclosures
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Akintayo, R.O., Yerima, A., Olaosebikan, H.B. et al. How much gloom is in groans? Depression and its determinants in Nigerian patients with knee osteoarthritis: a multi-center cross-sectional study. Clin Rheumatol 38, 1971–1978 (2019). https://doi.org/10.1007/s10067-019-04497-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-019-04497-2