Abstract
The objectives of this study are to assess the levels of serum Interleukin-35 (IL-35) in patients with idiopathic inflammatory myopathies (IIMs) and to evaluate the association between IL-35 levels and IIM-related features. Serum IL-35 was detected in 76 patients with dermatomyositis (DM), 28 patients with polymyositis (PM), 98 disease controls (40 rheumatoid arthritis (RA), 34 systemic lupus erythematosus (SLE), 12 systemic sclerosis (SSc), and 12 sjogren syndrome (SS)), and 43 healthy controls by ELISA. Follow-up was conducted on 34 patients. Serum IL-35 was higher in myositis (PM/DM) patients than in healthy controls (median 76.6 pg/ml [interquartile range (IQR) 57.9–136.2] vs. 29.9 pg/ml (IQR 21.9–65.5), P < 0.001) and disease controls. Serum IL-35 in IIM patients negatively correlated with disease duration moderately (r = −0.35, P < 0.01). Patients with dysphagia had higher IL-35 than those without (median149.35 pg/ml (IQR 87.97–267.32) vs. 70.72 pg/ml (IQR 54.49–123.42), P = 0.001). Cross-sectional correlation analysis showed a weak positive correlation between serum IL-35 and CK (r = 0.293, P = 0.003), moderate positive correlation with erythrocyte sedimentation rate (ESR) (r = 0.304, P = 0.002), serum ferritin (SF) (r = 0.467, P = 0.001) and LDH levels (r = 0.401, P < 0.001). Additionally, serum IL-35 was higher in patients who were positive for anti-HMGCR (median 292.04 pg/ml (IQR 67.9–442.86) vs. 74.66 pg/ml (IQR 57.24–131.32), P = 0.038) and anti-SRP antibody (median 130.33 pg/ml (IQR 88.04–481.28) vs. 73.06 pg/ml (IQR 56.78–134.28), P = 0.009) than in negative patients, respectively. Follow-up study showed that changes in IL-35 levels after treatment correlated with changes in MYOACT scores moderately (r = 0.375, P = 0.029). These data indicate that increased serum IL-35 could act as a disease activity marker and as a risk factor for esophageal involvement in IIM. IL-35 may participate in the pathophysiological processes of IIM, but it still needs further study to confirm.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic inflammatory myopathies (IIMs) are a group of heterogeneous, systemic disorders that can be divided into the following subtypes based on clinicopathological features: dermatomyositis (DM), polymyositis (PM), necrotizing autoimmune myositis (NAM), sporadic inclusion-body myositis (sIBM), and overlap myositis (OM) [1–3]. DM and PM are two major clinical subtypes of IIMs that occur in Chinese populations. The pathogenesis underlying IIMs is complicated and unclear. Cytokines were recognized to play both pro-inflammatory and anti-inflammatory roles [4, 5] in IIM processes. Interleukin-35 (IL-35) is a novel member of the IL-12 family, and it was thought to play a critical role in immunoregulatory and autoimmune disease processes. IL-35 is a heterodimeric cytokine composed of two subunits: p35 (IL-12a) and Epstein-Barr-virus-induced gene 3 (EBI3, IL-27b) [6]. Bioactive IL-35 is constitutively produced by regulatory T (Treg) cells and is required for their maximal suppressive capacity in mouse [6]. Human Treg cells do not express detectable amounts of IL-35 [7, 8], but IL-35 can convert human conventional CD4+Foxp3− T cells (Tconv) into induced regulatory T cells (iTR) that exhibit immunosuppressive functions [9]. To date, IL-35 has been studied in several autoimmune diseases, but its role remains controversial. Several studies report its pro-inflammatory roles [10–12] while others describe it as anti-inflammatory [13, 14]. To date, there has been no study conducted on IL-35 in IIMs. Therefore, we aimed to study IL-35 expression in sera of IIM patients and to evaluate its association with myositis-related features.
Materials and methods
Study population
From the patients admitted to China-Japan Friendship Hospital between April 2010 and September 2015, 104 adults who would be classified by the Bohan and Peter criteria as IIM patients [15, 16] were enrolled in our study. Patients with infections, tumors, and other non-IIM autoimmune diseases were excluded. Our initial evaluation divided the patients into two groups: those who showed a poor response to previous therapy (n = 63) and those who were treatment-naive (n = 41). Clinical and laboratory data were obtained from electronic medical records. The control group included 98 disease controls (40 patients with rheumatoid arthritis (RA), 34 with SLE, 12 with systemic sclerosis (SSc), and 12 with sjogren syndrome (SS)) and 43 healthy volunteers (27 females and 16 males, ages 23–70 with mean age of 47.7 years). There were no statistically significant differences between the age and sex compositions of the IIM patients and the healthy control group (P = 0.911, P = 0.381, respectively). Ethical approval for the research was obtained from the Research Review Committee (RRC) and the Ethical Review Committee (ERC) of the China-Japan Friendship Hospital. All serum samples were collected and stored at −80 °C until use.
Measurement of serum levels of IL-35
Serum samples were collected from the 104 IIM patients (76 DM patients and 28 PM patients), 98 disease controls (40 patients with RA, 34 with SLE, 12 with SSc, and 12 with SS), and the 43 healthy controls. Of the IIM patients, 34 were followed up (30 DM patients and 4 PM patients). The length of observation time between the first and last follow-up visits varied from 15 days to 53 months. The mean length of observation time was 11.1 months. Serum IL-35 levels were measured using an ELISA kit (USCN Life Sciences Inc., Hubei, China) according to the manufacturer’s protocol. A standard curve was generated for each plate, and the absolute concentrations of IL-35 were calculated. The limit of detection is 5.6 pg/ml.
Assessment of disease activity
Myositis disease activity was evaluated by using the Myositis Disease Activity Assessment Visual Analog Scales (MYOACT), established by the International Myositis Assessment and Clinical Studies (IMACS) group [17].
Statistical analysis
Data were analyzed by using SPSS V .17.0 (SPSS), and figures were plotted by using GraphPad Prism 5 (version 5.01; GraphPad Software). Measurement data are presented as mean ± SD unless stated otherwise. The normality of measured variables was assessed using the one-sample Kolmogorov Smirnov test. The unpaired t test or Mann-Whitney test was used for comparisons between groups. The Wilcoxon signed-rank test was used to compare paired data when appropriate. Some non-normal data were transformed to be normally distributed through log transformation. Pearson correlations and Spearman’s rank correlations were used to analyze normal and non-normal distribution data, respectively. Correlation (r) strength was defined as follows: 0.2 < r ≤ 0.3, weak correlation; 0.3 < r ≤ 0.5, moderate correlation; and 0.5 < r ≤ 1, strong correlation. P values less than 0.05 were considered to be statistically significant.
Results
Demographic characteristics of IIM patients and healthy controls
The 104 IIM patients who were enrolled in this study included 76 DM and 28 PM patients. Among them, 73 were female (70.2 %) and 31 were male (29.8 %), with ages ranging from 21 to 77 years (mean age 48.0 years). Median disease duration as measured at initial evaluation was 10.5 months (range 0.25–204 months). Table 1 summarizes the patients’ baseline characteristics around the time of blood sampling. There were no statistically significant differences between the age and sex compositions of the IIM patients and the healthy control group.
IL-35 is increased in the sera of IIM patients
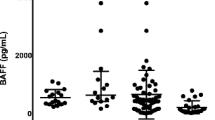
Serum levels of IL-35 in IIM patients were higher than those in healthy controls (median 76.6 pg/ml (IQR 57.9–136.2) vs. 29.9 pg/ml (IQR 21.9–65.5), P < 0.001), RA (35.1 pg/ml (IQR 18.18–65.9), P < 0.001), SLE (14.01 pg/ml (IQR 8.61–32.09), P < 0.001), SSc (53.39 pg/ml (IQR 24.33–78.98), P = 0.023), and SS (under the minimum detectable dose) patients (Fig. 1)). Although serum IL-35 levels in DM patients tended to be a little higher than those in PM patients, the difference was not statistically significant (Fig. 1). In order to know whether the serum levels of IL-35 could be influenced by drugs, we compared the serum IL-35 levels of 41 treatment-naive IIM patients with those of the patients who responded inadequately to previous therapy and found there was no statistically significant difference between the two subgroups (median 90.69 pg/ml (IQR 57.16–149.29) vs. 73.06 pg/ml (IQR 57.9–134.28), P = 0.28). The MYOACT scores of the two groups were 0.272 ± 0.096 and 0.193 ± 0.077, respectively (P < 0.01).
Serum levels of IL-35 in patients with DM/PM and in controls. a Serum levels of IL-35 are significantly higher in IIM patients than in other controls. b Serum IL-35 levels are higher in both IIM subsets than in healthy controls. c Serum IL-35 levels are higher in both group 1 and group 2 than in healthy controls. Horizontal bars represent the median. ***P < 0.001. NS not significant. Group 1: treatment-naive patients; group 2: patients who responded inadequately to previous therapy
Correlation between serum IL-35 levels and clinical manifestations
Furthermore, we conducted a correlation analysis between serum IL-35 levels and clinical manifestations. One interesting result was that the serum IL-35 levels of IIM patients correlated negatively with disease duration moderately (r = −0.35, P < 0.01) (Fig. 2). If we define disease duration less than or equal to 6 months as “early stage”, and disease duration longer than 6 months as “advanced stage”, then serum IL-35 levels were higher in “early stage” IIM patients than in “advanced stage” patients (P = 0.014). Another noteworthy finding was that serum IL-35 levels were significantly higher in patients with dysphagia than in patients without dysphagia (P = 0.001) (Fig. 2), but no significant differences were observed between patient subgroups with regard to Raynaud’s phenomenon, Mechanic’s hands, muscle weakness, different types of myositis-specific skin eruptions (Gottron sign, Heliotrope sign, V sign, Shawl sign, Holster syndrome), calcinosis, arthritis, and interstitial lung disease (ILD) (Table 2).
Correlation between serum IL-35 levels and clinical manifestations. a Serum IL-35 levels in IIM patients correlate negatively with disease duration moderately. Disease duration and concentration of serum IL-35 were log transformed in the statistical analyses. b Higher IL-35 serum levels were found in early stage IIM patients than in those with advanced disease (P = 0.035). *Disease duration ≤6 months; # disease duration >6 months. (Early stage vs. advanced stage). c Serum levels of IL-35 in IIM with or without dysphagia. d Serum levels of IL-35 in IIM with or without ILD. Horizontal bars represent the median
Correlation between serum IL-35 levels and laboratory parameters
Associations between serum IL-35 concentrations and laboratory data were also evaluated. Correlation analysis showed a weak correlation between serum IL-35 levels and CK (r = 0.293, P = 0.003), moderate positive correlation with erythrocyte sedimentation rate (ESR) (r = 0.304, P = 0.002), serum ferritin (SF) (r = 0.467, P = 0.001), and LDH (r = 0.401, P < 0.001) levels. Correlational analysis between serum IL-35 levels and peripheral blood lymphocyte subset counts showed no significant correlations. However, serum IL-35 levels were significantly higher in patients who were positive for antinuclear antibodies (ANA) (P = 0.026), anti-HMGCR antibody (P = 0.038), and anti-SRP antibody (P = 0.009) than in those who were negative, respectively (Fig. 3).
Correlation between serum IL-35 levels and laboratory data in IIM patients Correlations between the IL-35 levels and a serum creatine kinase (CK) levels (n = 102), b erythrocyte sedimentation rate (ESR) (n = 98), c serum ferritin (SF) levels (n = 48), and d lactate dehydrogenase (LDH) levels (n = 101) in IIM patients. Comparisons between serum IL-35 levels of e ANA-positive and ANA-negative patients (n = 88), f anti-HMGCR antibody-positive and anti-HMGCR antibody-negative patients (n = 104), g anti-SRP antibody-positive and anti-SRP antibody-negative patients (n = 104); all patients have IIM. Horizontal bars represent the median. Each point represents an individual sample. Serum IL-35, CK, ESR, and SF values in Fig. 3a–c were log transformed in the statistical analyses
Serum IL-35 is associated with clinical disease activity in IIM patients
We further investigated whether serum IL-35 levels could be associated with myositis activity. Disease activity was evaluated according to MYOACT scores at the time of blood sampling. We found a weak positive correlation between serum IL-35 levels and MYOACT scores (r = 0.274, P = 0.005) in a cross-sectional study of the 104 IIM patients. The correlation existed especially for PM patients (r = 0.459, P = 0.014) (Fig. 4a–c).
Correlation between serum IL-35 levels and myositis disease activity. a Serum IL-35 levels vs. MYOACT scores in IIM patients (n = 104). b Serum IL-35 levels vs. MYOACT scores in DM patients (n = 76). c Serum IL-35 levels vs. MYOACT scores in PM patients (n = 28). d Serum IL-35 levels, e serum CK levels, and f MYOACT scores were significantly decreased after treatment. g Changes in IL-35 levels after treatment correlated positively with changes in MYOACT scores moderately. Serum IL-35 values in Fig. 4a, b were log transformed in the statistical analyses. Changes in MYOACT scores refer to decrease rates of MYOACT scores which mean MYOACT scores before treatment minus MYOACT scores after treatment and then divided by MYOACT scores before treatment. So do the changes in serum IL-35 levels
Follow-up study
In order to further investigate whether the changes in serum IL-35 levels could reflect the changes in disease activity, a follow-up study was conducted on 34 patients. The median follow-up time was 11.1 months with a range of 0.5–53 months. Serum and clinical data were collected at each follow-up visit. Serum levels of IL-35 (P = 0.014) and CK (P < 0.001) were decreased significantly after treatment with glucocorticoids and immunosuppressive agents (Fig. 4d, e). Myositis disease activity also decreased (P < 0.001) (Fig. 4f). A moderate positive correlation was found between changes in serum IL-35 levels and changes in MYOACT scores (r = 0.375, P = 0.029) (Fig. 4g).
Discussion
In this study, we found that serum IL-35 levels in patients with PM/DM were higher than in healthy controls. The role of IL-35 in IIM is unknown. IL-35 may play dual roles in the regulation of autoimmune diseases and depend heavily on T cell activation, in a similar manner as TGF-β and IL-10 [18–21]. In our study, serum IL-35 levels in SLE patients and SS patients were lower than in healthy controls while there was no statistically significant difference of serum IL-35 in RA and SSc patients when compared to healthy controls. So, IL-35 activity can be complex and context-dependent, and in a given system, we may only see the net outcome of its multiple effects. In DM/PM, it may act as an anti-inflammatory cytokine but not exert its suppressive role if the corresponding receptor expression is lacking, or there may be other defects in the suppressive signaling pathway of IL-35 in PM/DM patients [22], or elevated levels of IL-35 may be a protective anti-inflammatory response to diseases that protect against pathogenic factors to avoid the impairment of tissues and organs, but this upregulation may be antagonized by pro-inflammatory factors like in SLE [23]. However, we cannot exclude the possibility of a pro-inflammatory role that elevated serum IL-35 could play in PM/DM patients.
Concerning the sources of elevated serum IL-35 in IIM patients, our study shows there was no correlation between serum IL-35 levels and peripheral blood lymphocyte subset counts. Other studies showed a lower percentage of peripheral blood Treg cells in PM/DM patients than in healthy controls. Also, CD3 (+) cells, CD3 (+) CD4 (+) cells, and CD3 (+) CD8 (+) cells in patients with active DM patients were lower than in patients with inactive DM and in healthy controls [24–26]. Based on these data, we speculate that the sources of IL-35 may be stimulated, not by peripheral blood T cells, but by human skeletal muscle cells, which can secrete many kinds of cytokines under pro-inflammatory stimuli in PM/DM patients [27]. Other non-T cell sources, such as immature dendritic cells, microvascular endothelial cells, epithelial cells, CD138+ plasma cells, and smooth muscle cells, may also contribute to the elevated serum IL-35 [28–32]. But the exact origin of the serum IL-35 in IIM still needs to be explored.
One interesting finding in our study is that the serum levels of IL-35 correlated negatively with IIM disease duration. We do not know the reason for these results. Perhaps it is because the different pathways involved have varying levels of influence during the different stages of the disease, and the results may suggest that IL-35-related immune pathways may play a more important role in the early stages than in the advanced stages of IIMs. However, the exact mechanism of the difference needs to be investigated.
Dysphagia is a refractory complication that lacks a definitive serum biomarker in IIM. Our study reveals that IIM patients with dysphagia have significantly higher IL-35 levels than those without. Meanwhile, serum IL-35 levels were higher in patients carrying anti-HMGCR and anti-SRP antibodies than in patients who did not carry those autoantibodies. The anti-HMGCR and anti-SRP antibodies have been shown to be significantly associated with severe necrotizing myopathy, and their presence increases the risk for dysphagia [33, 34]. Our results indicate that elevated serum IL-35 could be used as a marker for dysphagia, in addition to the anti-SRP and anti-HMGCR autoantibodies. It was reported that IL-35 does not affect human primary aortic smooth muscle cell apoptosis, necrosis, or viability [35]. But there is no report on the effect of IL-35 on esophageal smooth muscle. Our data invites consideration of this interesting question. The mechanism of the association between IL-35 and dysphagia still needs to be studied.
It is worth noting that serum levels of IL-35 seem to be unaffected by the use of corticosteroids or immunosuppressive agents. However, IL-35 was significantly associated with myositis disease activity as represented by MYOACT scores, especially in PM patients. Follow-up studies also show decreased serum IL-35 levels after disease remission, and the change in IL-35 levels after treatment correlated with the change in MYOACT scores. These data suggest that increased serum IL-35 could act as a disease activity marker in clinical practice.
The limitation of our study is that we did not detect IL-35 expression in IIM muscle tissue and did not find the source of IL-35, so further studies are required to elucidate these potential mechanisms. Our study is a single center study and it still needs confirmation in additional centers.
In conclusion, this study is the first to show that serum IL-35 levels are elevated in both PM and DM patients, and increased serum IL-35 could be an IIM disease activity marker and risk factor for esophageal involvement in IIM. Our findings suggest that IL-35 may participate in the pathogenesis of IIM but it still needs to be confirmed. Further study is necessary to clarify the source of serum IL-35 production and its immunoregulatory role in IIMs.
References
Dalakas MC (2015) Inflammatory muscle diseases. N Engl J Med 372:1734–1747
Dalakas MC, Hohlfeld R (2003) Polymyositis and dermatomyositis. Lancet 362:971–982
Dalakas MC (1991) Polymyositis, dermatomyositis and inclusion-body myositis. N Engl J Med 325:1487–1498
Mei Z, Lundberg IE (2011) Pathogenesis, classification and treatment of inflammatory myopathies. Nat Rev Rheumatol 7:297–306
Lundberg IE (2000) The role of cytokines, chemokines, and adhesion molecules in the pathogenesis of idiopathic inflammatory myopathies. Curr Rheumatol Rep 2:216–224
Collison LW, Workman CJ, Kuo TT, et al. (2007) The inhibitory cytokine IL-35 contributes to regulatory T-cell function. Nature 450:566–569
Bardel E, Larousserie F, Charlot-Rabiega P, et al. (2008) Human CD4+CD25+Foxp3+ regulatory T cells do not constitutively express IL-35. J Immunol 181:6898–6905
Allan SE, Song-Zhao GX, Abraham T, et al. (2008) Inducible reprogramming of human T cells into Treg cells by a conditionally active form of FOXP3. Eur J Immunol 38:3282–3289
Collison LW, Chaturvedi V, Henderson AL, et al. (2010) IL-35-mediated induction of a potent regulatory T cell population. Nat Immunol 11:1093–1101
Filkova M, Vernerova Z, Hulejova H, et al. (2015) Pro-inflammatory effects of interleukin-35 in rheumatoid arthritis. Cytokine 73:36–43
Kuo J, Nardelli DT, Warner TF, et al. (2011) Interleukin-35 enhances Lyme arthritis in Borrelia-vaccinated and -infected mice. Clin Vaccine Immunol: CVI 18:1125–1132
Thiolat A, Denys A, Petit M, et al. (2014) Interleukin-35 gene therapy exacerbates experimental rheumatoid arthritis in mice. Cytokine 69:87–93
Niedbala W, Wei XQ, Cai B, et al. (2007) IL-35 is a novel cytokine with therapeutic effects against collagen-induced arthritis through the expansion of regulatory T cells and suppression of Th17 cells. Eur J Immunol 37:3021–3029
Wang RX, Yu CR, Dambuza IM, et al. (2014) Interleukin-35 induces regulatory B cells that suppress autoimmune disease. Nat Med 20:633–641
Bohan APJ (1975) Polymyositis and dermatomyositis (second of two parts). N Engl J Med 292:403–407
Bohan APJ (1975) Polymyositis and dermatomyositis (first of two parts). N Engl J Med 292:344–347
Isenberg DA, Allen E, Farewell V, et al. (2004) International consensus outcome measures for patients with idiopathic inflammatory myopathies development and initial validation of myositis activity and damage indices in patients with adult onset disease. Rheumatology (Oxford) 43:49–54
Bettelli E, Korn T, Oukka M, et al. (2008) Induction and effector functions of T(H)17 cells. Nature 453:1051–1057
Llorente L, Zou W, Levy Y, et al. (1995) Role of interleukin 10 in the B lymphocyte hyperactivity and autoantibody production of human systemic lupus erythematosus. J Exp Med 181:839–844
Macneil IA, Suda T, Moore KW, et al. (1990) IL-10, a novel growth cofactor for mature and immature T cells. J Immunol 145:4167–4173
Shachar I, Karin N (2013) The dual roles of inflammatory cytokines and chemokines in the regulation of autoimmune diseases and their clinical implications. J Leukoc Biol 93:51–61
Cai Z, Wong CK, Kam NW, et al. (2015) Aberrant expression of regulatory cytokine IL-35 in patients with systemic lupus erythematosus. Lupus 24
Qiu F, Song L, Yang N, et al. (2013) Glucocorticoid downregulates expression of IL-12 family cytokines in systemic lupus erythematosus patients. Lupus 22:1011–1016
Banica L, Besliu A, Pistol G, et al. (2009) Quantification and molecular characterization of regulatory T cells in connective tissue diseases. Autoimmunity 42:41–49
Antiga E, Kretz CC, Klembt R, et al. (2010) Characterization of regulatory T cells in patients with dermatomyositis. J Autoimmun 35:342–350
Wang DX, Lu X, Zu N, et al. (2012) Clinical significance of peripheral blood lymphocyte subsets in patients with polymyositis and dermatomyositis. Clin Rheumatol 31:1691–1697
Nagaraju, Raben, Merritt, et al. (1998) A variety of cytokines and immunologically relevant surface molecules are expresssed by normal skeletal muscle cells under proinflammatory stimuli. Clin Exp Immunol 113:407–414
Kempe S, Heinz P, Kokai E, et al. (2009) Epstein-barr virus-induced gene-3 is expressed in human atheroma plaques. Am J Pathol 175:440–447
Seventer JMV, Nagai T, Seventer GAV (2002) Interferon-beta differentially regulates expression of the IL-12 family members p35, p40, p19 and EBI3 in activated human dendritic cells. J Neuroimmunol 133:60–71
Heidemann J, Rüther C, Kebschull M, et al. (2008) Expression of IL-12-related molecules in human intestinal microvascular endothelial cells is regulated by TLR3. Am J Physiol Gastrointest Liver Physiol 293:G1315–G1324
Maaser C, Egan LJ, Birkenbach MP, et al. (2004) Expression of Epstein-Barr virus-induced gene 3 and other interleukin-12-related molecules by human intestinal epithelium. Immunology 112:437–445
Xinyuan L, Jietang M, Anthony V, et al. (2012) IL-35 is a novel responsive anti-inflammatory cytokine—a new system of categorizing anti-inflammatory cytokines. PLoS One 7:65–65
Targoff IN, Johnson AE, Miller FW (1990) Antibody to signal recognition particle in polymyositis. Arthritis Rheum 33:1361–1370
Kao AH, David L, Mary L, et al. (2004) Anti-signal recognition particle autoantibody in patients with and patients without idiopathic inflammatory myopathy. Arthritis Rheum 50:209–215
Skowron W, Zemanek K, Wojdan K, et al. (2015) The effect of interleukin-35 on the integrity, ICAM-1 expression and apoptosis of human aortic smooth muscle cells. Pharmacol Rep: PR 67:376–381
Acknowledgments
This work was supported by the National Natural Science Foundation of China (9154212181571603) and the Science and Technology Commission Foundation of Beijing (No:Z151100004015143).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval for the research was obtained from the Research Review Committee (RRC) and the Ethical Review Committee (ERC) of the China-Japan Friendship Hospital.
Disclosures
None.
Rights and permissions
About this article
Cite this article
Yin, L., Ge, Y., Yang, H. et al. The clinical utility of serum IL-35 in patients with polymyositis and dermatomyositis. Clin Rheumatol 35, 2715–2721 (2016). https://doi.org/10.1007/s10067-016-3347-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-016-3347-1