Abstract
Multilevel studies have gained importance for highlighting social inequalities in health. These associations have been reported previously in diseases such as arthritis and chronic pain. We conducted a cross-sectional study using multilevel analysis to identify individual and contextual factors associated with the variation of prevalence of osteoarthritis (OA) in the Mexican population. The sample included 17,566 individuals of which 10,666 (60.7 %) were women. The relationship between individual and contextual factors and OA were analyzed with a multilevel strategy. From the total population, 1,681 individuals had OA. Multilevel analysis showed that individual variables such as female gender (odds ratio (OR) = 1.3, 95 % confidence interval (CI) 1.1, 1.4), age range 55–65 years (OR = 1.6, 95 % CI 1.3, 2.0), musculoskeletal pain in the last 7 days (OR = 2.6, 95 % CI 2.3, 3.0), and use of pain treatments (OR = 1.4, 95 % CI 1.2, 1.7) were associated with OA. At the regional level, the Social Gap Index (SGIx) was associated with the diagnosis of OA (coefficient 0.5, 95 % CI 0.2–1.1). The SGIx contextual variable was positively associated with the regional prevalence of OA and the variation in prevalence of OA in different regions. The larger the social gap, the greater the variation in OA prevalence. These factors were independently associated with the prevalence of OA: female gender, pain intensity, physical limitation, and the use of pain treatments were individual variables associated with OA. The association between OA prevalence and regional variations with SGIx reflects inequities in health provisions that should be considered in health programs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Educational, economic, and health care inequities characterize human society. In a wide sense, social inequity has been recognized as an important factor in health and disease. Health inequity refers to the moral or ethical dimensions of health inequality. Health inequality refers to variations in health status across individuals in a population [1]. Social inequity plays an important role in the prevalence of chronic diseases [1, 2], but information related to rheumatic diseases is still scarce [3, 4]. Few studies have identified the existence of inequities among patients with rheumatoid arthritis (RA) [4], osteoarthritis (OA) [5], and systemic lupus erythematosus [6] in any country.
Despite the fact that social inequities and consequentially health care inequities may be recognized in developed and underdeveloped nations, the problem is greater in those lacking a health care system that covers the whole population. That is the case in many Latin American, Asian, and African countries, and in the United States of “North” America to some extent. In particular, the Mexican health care system is a mixed or fragmented model, in which around half of the population is not covered by the state and the expenses generate great economic and social inequities. The burden of disease affects the household through out-of-pocket expenses and restrains economic growth and family activities. In contrast, the impact of the disease in the population covered by the national health budget is much less important. The proportion of households having catastrophic expenses resulting from RA as a consequence of impoverishment is much greater that in those covered by the state [7, 8].
We recently reported the results of a large epidemiological study to determine the prevalence of the most important rheumatic diseases in 17,566 individuals distributed in several states. The results showed OA as the most common of the rheumatic diseases with a prevalence of 9.5 % (95 % CI 9.1, 10.0). A more detailed analysis of the data showed wide geographic variations, ranging from 2.5 to 16.3 %, which were not easily explained by methodological and individual characteristics. Nonetheless, because we carried out our study in geographical regions with uneven socioeconomic indicators [9], we hypothesized that social inequity could play a role in the prevalence of OA in each of the geographic areas studied. The approach of these geographic variations was based on a multilevel contextual design, which is able to detect social inequalities in health. Therefore, we aimed to identify individual and contextual factors associated with the prevalence of OA and integrate the level of social and cultural elements influencing health and disease.
Materials and methods
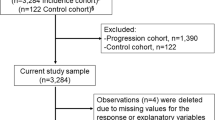
This is a secondary analysis of the database of a previously published study on the prevalence of musculoskeletal (MSK) symptoms and rheumatic conditions, including OA, carried out in the Mexican population [9]. Briefly, the study was cross-sectional and included communities from the states of Nuevo Leon, Sinaloa, Yucatan, and Mexico City. The Community Oriented Program for the Control of Rheumatic Diseases (COPCORD) questionnaire was used to identify patients with nontraumatic MSK pain and collect a number of demographic, clinical, therapeutic, economic, and educational information. Additional questionnaires were administered to obtain clinical, therapeutic, economical, educational, and functional capacity data. A positive MSK case definition was an individual with nontraumatic MSK pain >1 on a visual analog scale (0 to 10) in the last 7 days or in the past. Positive cases were referred to board certified rheumatologists for diagnosis. The diagnosis of OA was established according to American College of Rheumatology criteria [10–12]. We consider “cases” those individuals who had symptomatic OA, which we define as those patients who reported the presence of pain or discomfort and stiffness accompanied by articular crepitus. Only borderline cases were asked to undergo a radiographic study. The sample that underwent analysis included 17,566 individuals (60.7 % women) with a mean age of 43.1 years (17.4 standard deviation [SD]; range 18–99 years). The group of controls in this study included all individuals without OA. The study protocol was previously approved by the Institutional and Ethics Committees of each participating institution. All study participants were informed of the study procedures prior to their participation and voluntarily signed informed consent forms.
Construction of the multilevel model
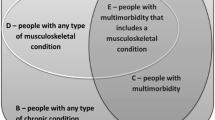
We included variables related to the individual in the level 1 model whereas the level 2 model comprised all variables related to collective or contextual data (for a complete definition of variables, please see Table 1 and Fig. 1). The level 1 model included the following variables: (1) socioeconomic variables: age and gender, economic and educational level, work status, household income, housing facilities, and support for health care access; (2) individual’s lifestyle (tobacco and alcohol consumption), clinical (MSK pain, self-reported comorbidities, previous treatments, and medical and alternative therapy), and physical disability variables (Health Assessment Questionnaire-Disability Index [HAQ-DI])[13]. Level 1 variables were all obtained from the COPCORD questionnaire that each individual had already completed.
Level 2 model variables included group information, i.e., state information [14]. The selection of these variables was probabilistic and according to risk factors described in the literature for its association with OA [15–20]. The model included the following instruments and topics: (a) Human Development Index (HDIx) [21], (b) Gini coefficient for inequality [22], (c) urbanization [23], (d) gross national product (GNP) [24], (e) health care access [25], (f) the Migration Index (MiIx) [26], (g) unemployment [27], (h) the Marginalization Index (MaIx) [28], and (i) the Social Gap Index (SGIx) [29]. Information was extracted from the National Institute of Statistics and Geography (INEGI), the National Population Council (CONAPO), the National Health Survey (ENUSALUD), and the National Council for the Evaluation of Social Development Policy (CONEVAL), all Mexican electronic databases. Of special interest is the SGIx, which is an aggregate of variables extracted from the database of the CONEVAL, which incorporates indicators of education, access to health services, basic services, of housing quality and space, and household assets. This index is scored as very low, medium, and very high social underdevelopment, which is interpreted as those locations that range from lower to higher limitations in the indicators (a higher score means more limitations) [30].
Statistical analysis
In the descriptive analysis, we reported measures of central tendency and dispersion as continuous variables and absolute and relative frequencies in ordinal as well as nominal or categorical variables. For each variable, we performed a bivariate analysis with analysis of variance (ANOVA), one and two-tailed for continuous variables, and the chi-square test for ordinal, nominal, or categorical variables. The presence of each individual variable was evaluated in the model by a stepwise selection methodology; the initial model was a full descriptive model, but additional parameters were deleted in each step. The significance of parameters was evaluated using the Wald test. For the multivariate analysis, we used a two-level logistic model, level 1 for individual variables and level 2 for contextual variables. A multilevel analysis was performed with simultaneous analysis of the influence of individual and community characteristics in relation to variations of OA prevalence [31]. Given the constraints of sample size, we did not add the states as a first-level unit to the model [32], but rather the municipalities (counties) within it. The initial phase of analysis corresponded to raw comparisons using the chi-square test.
To verify the suitability of the multilevel approach, we calculated the intra-class correlation coefficient (ICC). The association between such variables and the prevalence of OA (and its uncertainty) were assessed at the individual level by odds ratio (OR) and 95 % confidence intervals (95 % CI; fixed model effect). To incorporate state variations in the relation between variables and the prevalence of OA, we considered regional variables as random effects. The structure of the covariance matrix used in this study did not allow for a correlation analysis of the levels of information. The final model was achieved after a backward selection process, stage by stage, eliminating one variable by one to obtain first, the individual model, and then the regional and individual variables at the same time. Changes in each model were examined using likelihood criteria [30]. The OR was calculated from the median as a measure of heterogeneity among the different geographic areas. This measure can be defined as the median of the ORs obtained by choosing two random individuals with the same covariates, but from different geographic areas [32]. Unobserved heterogeneity was quantified by considering the median OR for pairs of randomly sampled persons having the same covariate value, i.e., living in the same area. The aim of the median odds ratio (MOR) is to translate the area level variance in the widely used OR scale, which has a consistent and intuitive interpretation. The MOR is defined as the median value of the OR between the area at highest risk and the area at lowest risk when randomly choosing two areas. MOR can be conceptualized as the increased indirect risk that (in a median value) would occur if moving to another area with a higher risk [32]. All analyses were performed using the statistical package STATA v 11 (College Station, Texas, USA [33].
Results
The diagnosis of OA was established in 1,681 individuals. The prevalence of OA was 9.5 %( 95 % CI 9.1, 10.0), higher in women than in men [10.9 % (IC95% 10.3–11.5) vs. 7.3 % (IC95% 6.7–8.0), p < 0.01]. By age group, the prevalence of OA was 4.8 % (95 % CI 4.4, 5.2) in individuals ≤45 years, 14.0 % (95 % CI 1.0, 15.0) in individuals between 46 and 65 years, and 21.4 % (95 % CI 19.7, 23.2) in those over ≥65 years. Interestingly, the prevalence of OA varied from 2.5 % in Sinaloa to 6.7 % in Yucatan, 12.8 % in Mexico City, and 16.3 % in Nuevo Leon. Compared with control individuals, the subjects with OA reported VAS pain in the last 7 days with an intensity ≥4 (6.1 vs. 3.4 %, p < 0.01), physical limitations (9.6 vs. 4.0 %, p < 0.01), and greater use of pain treatments (55.5 vs. 44.4 %). OA prevalence in individuals under 45 years was 4.8 % (95 % CI 4.4, 5.2), in those between 46 and 65 years 14.0 % (95 % CI 1.0, 15.0), and in those over 65 years 21.4 % (95 % CI 19.7, 23.2).
Individual variables
Significant differences contextual variables in individuals with and without OA included income 25.8 (95 % CI 26.1, 27.4) vs. 17.2 (95 % CI 15.5, 18.8); education 8.5 (95 % CI 8.5, 8.6) vs. 7.9 (95 % CI 7.6, 8.3) (Table 2).
The group of individuals with OA had greater pain intensity (OR = 2.6, 95 % CI 2.5, 3.0), physical limitation (OR = 1.6, 95 % CI 1.5, 1.8), paid work (OR = 0.7, 95 % CI 0.7, 0.8), HAQ_DI score greater than 1.0 (OR = 3.3, 95 % CI 2.9, 3.7), and increased use of therapies for pain (OR = 4.3, 95 % CI 3.8, 4.7) compared with controls.
Contextual variables
The GNP and the SGIx were significantly different across states. All other regional differences of contextual variables are shown in Table 3.
Multilevel analysis
-
Multilevel model 1
The inclusion of regional variables in the analysis confirmed the existence of significant variations in the prevalence of OA even after controlling for individual factors (χ 2 = 549.69, P < 0.001). The multilevel model, including all regional and individual effects, showed statistically significant differences regarding the prevalence of OA associated with female gender (OR = 1.3, 95 % CI 1.1, 1.4), higher age (OR = 1.6, 95 % CI 1.3, 2.0), MSK pain in the last 7 days (OR = 2.6, 95 % CI 2.2, 3.0), pain treatments (OR = 1.4, 95 % CI 1.2, 1.7), and SGIx (OR = 0.3, 95 % CI 0.2, 0.6). All other variables were marginal or not significant (see Table 4).
Table 4 Multilevel model 1. Regional effects and significant individual effects -
Multilevel model 2
SGIx was the unique variable showing significant effect at the regional level (see Table 5). The model showed significant variation in the OR by SGIx level. Thus, an increase of 1 SGIx unit in a specific state implied an increase of 1 standard deviation in the OR resulting from comparison of OA and the reference value. However, the estimate of this effect was so variable that the magnitude of the standard error of the coefficient represents 46 % of its value (SE = 0.2). Thus, the states with high SGIx (i.e., Yucatan, mean −1.2, SD 0.4) were characterized by a greater social underdevelopment in comparison with the state with the lowest SGIx (Mexico City, mean −2.0, SD 0), which is one standard deviation below the overall mean (−1.3 SD 0.8)(see Table 3).
Table 5 Multilevel model 2. Association of significant regional and individual variables Interaction between level l data and level 2 was not statistically significant, though we found considerable variation in the presence of pain in the last 7 days, marital status, use of pain treatments, physical limitation, decreased ability to bend over and squat, and age (see Table 5).
The interpretation of the hypothesis is that the effects associated with each of the individual variables are not significant. The chi-square test indicated that the variation in the prevalence of OA, once adjusted for the effect of individual variables, was significantly heterogeneous in terms of the values of the index of the social gap.
Discussion
We found individual and contextual factors associated with the variable prevalence of OA in the Mexican population. The implementation of two multilevel models to determine the influence of social and cultural elements in this study followed today’s global initiatives to identify health disparities as well as to prevent and reduce the impact of MSK diseases in the general population [34]. In this sense, our study is consistent with the research proposal of the CONEVAL [35], which refers to the identification of global factors affecting health equity, defined “as the absence of systematic differences in health, between and within countries that are avoidable by reasonable action” [36].
Regarding individual variables in the level 1 model, we found significant associations between the prevalence of OA and female gender as well as older age and at least three related variables: pain of great intensity, use of pain treatments, and functional limitations for which temporality should be analyzed in detail. A community study of hip OA found a significant association between HAQ_DI score and levels of education and poverty [37]. That association could result in limited access to public transportation as well as exercise facilities and result in individuals being less responsible and less conscious about their own health. The association implies a considerable impact of disease in the health community environment.
In this study, the contextual variable SGIx was significantly associated with the variability of OA prevalence in the community. SGIx is an aggregation of variables extracted from the CONEVAL, a decentralized public database that produces information about social policies, including the measurement of poverty. The association between SGIx and the prevalence of OA in the community was not homogeneous. There was a significant variation in the prevalence of OA after adjusting by individual variables. The prevalence of OA was higher in communities with lower SGIx. This finding of the effect of the variable social underdevelopment in the presence of OA leads us to hypothesize that the effect of social underdevelopment is less in places where social underdevelopment is very high. Reasons include high social underdevelopment, less education, less access to health services, and poor housing. People living in such conditions seem to be more aware of health problems, including MSK diseases and therefore seek medical care early. Alternatively, it is possible that social poverty, among other factors would mask health problems, including OA, as consequence of limitations in education, access to health care, and proper housing. This interpretation is consistent with the fact that in our study, the level of education and household income in patients with OA were much lower than in the control group.
In contrast to our findings, some studies have shown that the prevalence of chronic pain was higher in individuals that live in urban areas characterized by poor education, social networks, and income [16, 20], but high SGIx [15]. On the other hand, a multilevel model study developed in Australia showed a higher prevalence of arthritis in communities with a high SGIx [16]. Explanations for this include the case definitions based on self-reports, the fact that these studies were conducted in developed countries where socioeconomic inequalities are not as marked as those in developing countries, and the use of different social indicators in each study.
Our study has some limitations. The cross-sectional measurement of the data does not allow for the identification of causal inferences that in some cases may be bidirectional. The sample size was different for each state and some of the estimates might vary. The statistical technique used in the study might have some limitations on the model's ability to assign contextual effects to individuals (ecological fallacy) [38]. Additionally, residual confounding may be a problem due to the omission of individual variables related to the characteristics of the group under study and to the prevalence of OA [39]. Nevertheless, we think that such shortcomings did not affect the analysis performed in this study.
Conclusion
The SGIx was positively associated with OA regional prevalence. Female gender, pain intensity, physical limitation, and the use of pain treatments were individual variables associated with OA. These factors were independently associated with the prevalence of OA. The association of SGIx with variations in the prevalence of OA in this study suggests that health inequity in populations with greater social underdevelopment have a higher prevalence of OA and therefore secondary disability. This situation is associated with limited access to healthcare, low educational level, and social disadvantage. It is therefore advisable to design and implement interventional programs aimed primarily at individuals with scarce resources and management tools to improve the health of rheumatic patients in the population.
References
Asada Y (2005) A framework for measuring health inequity. J Epidemiol Community Health 59:700–705
Organization for economic co-operation and development (OECD) (2013) Health at a Glance 2013: OECD Indicators. OECD Publishing PhysicsWeb. doi: 10.1787/health_glance-2013. Accessed 03 April 2014
Cleveland RJ, Luong ML, Knight JB et al (2013) Independent associations of socioeconomic factors with disability and pain in adults with knee osteoarthritis. BMC Musculoskelet Disord 14:297
Putrik P, Sokka T, Ramiro S, Boonen A (2012) Impact of socioeconomic gradients within and between countries on health of patients with rheumatoid arthritis (RA): lessons from QUEST RA. Best Pract Res Clin Rheumatol 26:705–720
Luong ML, Cleveland RJ, Nyrop KA, Callahan LF (2012) Social determinants and osteoarthritis outcomes. Aging health 8:413–437
Calixto OJ, Anaya JM (2014) Socioeconomic status. The relationship with health and autoimmune diseases. Autoimmun Rev 13:641–654
Mould-Quevedo J, Peláez-Ballestas I, Vázquez-Mellado J et al (2008) El costo de las principales enfermedades reumaticas inflamatorias desde la perspectiva del paciente en México. Gac Med Mex 144:225–231
Álvarez-Hernández E, Peláez-Ballestas I, Boonen A et al (2012) Catastrophic health expenses and impoverishment of households of patients with rheumatoid arthritis. Reumatol Clin 8:168–173
Peláez-Ballestas I, Sanin LH, Moreno-Montoya J et al (2011) Epidemiology of the rheumatic diseases in Mexico. A study of 5 regions based on the COPCORD methodology. J Rheumatol 38(Suppl 86):3–8
Altman R, Asch E, Bloch D et al (1986) Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum 29:1039–1049
Altman R, Alarcon G, Appelrouth D et al (1990) The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hand. Arthritis Rheum 33:1601–1610
Altman R, Alarcon G, Appelrouth D et al (1991) The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum 34:505–514
Alvarez-Hernández E, Peláez-Ballestas I, Vázquez-Mellado J et al (2008) Validation of the Health Assessment Questionnaire Disability Index in patients with gout. Arthritis Rheum 59:665–669
Hernández-Avila M, Garrido-Latorre F, López-Moreno S (2000) Diseños de estudios epidemiológicos. Salud Pub Mex 42:142–144
Jordan KP, Thomas E, Peat G, Wilkie R, Croft P (2008) Social risk for disabling pain in older people: a prospective study of individual and area characteristics. Pain 137:652–661
Brennan SL, Turrell G (2012) Neighborhood disadvantage, individual-level socioeconomic position, and self-reported chronic arthritis: a cross-sectional multilevel study. Arthritis Care Res 64:721–728
Winkleby M, Sundquist K, Cubbin C (2007) Inequities in CHD incidence and case fatality by neighborhood deprivation. Am J Prev Med 32:97–106
Cramm JM, Moller V, Nieboer AP (2012) Individual- and neighbourhood-level indicators of subjective well-being in a small and poor Eastern Cape township: the effect of health, social capital, marital status, and income. Soc Indic Res 105:581–593
Hart JE, Laden F, Puett R, Costenbader KH, Karlson EW (2009) Exposure to traffic pollution and increased risk of rheumatoid arthritis. Environmental Health Perspectives 117:1065–1069
Brekke M, Hjortdahl P, Kvien TK (2002) Severity of musculoskeletal pain: relations to socioeconomic inequality. Soc Sci Med 54:221–228
21.United Nations Development Program (UNDP)(2004) Human development index. UNDP Publishing PhysicsWeb. http://hdr.undp.org/es/content/informe-sobre-desarrollo-social-y-humano-mexico-2004. Accessed 07 April 2014
National Council for the Evaluation of Social Development Policy(CONEVAL) ( 2005) Gini index. CONEVAL Publishing PhysicsWeb. http://www.coneval.gob.mx/Medicion/Paginas/Mapas-de-desigualdad-2000-2005-en.aspx. Accessed date 16 April 2014
United Nations Development Program (UNDP) (2005) Urbanization level by municipalities. UNDP Publishing PhysicsWeb. http://www.undp.org/content/undp/en/home.html. Accessed date 07 August 2012
National Council for the Evaluation of Social Development Policy (CONEVAL) (2010) Gross national product by municipality. CONEVAL Publishing PhysicsWeb. http://www.coneval.gob.mx/Paginas/principal.aspx. Accessed date 07 August 2012
National Institute of Statistics and Geography(INEGI) (2009) Percentage of persons with health insurance by municipality .INEGI Publishing PhysicsWeb. http://www.inegi.org.mx/. Accessed date 13 August 2012
National Population Council (CONAPO) (2002) Migration Index. CONAPO Publishing PhysicsWeb. http://www.conapo.gob.mx/es. Accessed date 07 August 2012
National Institute of Statistics and Geography(INEGI) (2011) Desempleo.INEGI Publishing PhysicsWeb. http://www.inegi.org.mx/. Accessed date 13 August 2012
National Population Council (CONAPO) (2000) Marginalization Index. CONAPO Publishing PhysicsWeb. http://www.conapo.gob.mx/es/CONAPO/Indices_de_marginacion_2000_. Accessed date 03 April 2014
National Council for the Evaluation of Social Development Policy(CONEVAL) (2010) Social Gap Index 2005.CONEVAL Publishing PhysicsWeb. http://www.coneval.gob.mx/Medicion/Paginas/Índice-de-Rezago-social-2010-en.aspx. Accessed date 14 August 2012
Coneval.gob.mx. Maps of Poverty in Mexico. Technical methodological Appendix [homepage on the Internet]. Mexico City Available from: http://www.coneval.gob.mx/Medicion/Paginas/Medici%C3%B3n/Anexo-Estadistico-Pobreza-2010-en.aspx. Accessed date 14 August 2012
Snijders TA (2005) Power and sample size in multilevel modeling. In: Everitt BS, Howell DC (eds) Encyclopedia of statistics in behavioral science. Wiley, Chichester, pp 1570–1573
Larsen K, Merlo J (2005) Appropriate assessment of neighborhood effects on individual health: integrating random and fixed effects in multilevel logistic regression. Am J Epidemiol 161:81–88
StataCorp (2009) Statistical software: release 11. Stata Corporation, College Station
Callahan LF (2003) Social epidemiology and rheumatic disease. Curr Opin Rheumatol 15:110–115
Ostlin P, Schrecker T, Sadana R et al (2011) Priorities for research on equity and health: towards an equity-focused health research agenda. PLoS Med. doi:10.1371/journal.pmed.1001115
World Health Organization(WHO) (2008) Closing the gap in a generation: health equity through action on the social determinants of health. Commission on Social Determinants of Health Final Report. Geneva: World Health Organization. WHO Publishing PhysicsWeb. http://www.who.int/social_determinants/thecommission/finalreport/en/. Accessed 03 April 2014
Knight JB, Callahan LF, Luong ML et al (2011) The association of disability and pain with individual and community socioeconomic status in people with hip osteoarthritis. Open Rheumatol J 5:51–58
Diex-Roux AV (1988) Bringing context back into epidemiology: variables and fallacies in multilevel analysis. Am J Public Health 88:216–222
Diez-Roux AV (2000) Multilevel analysis in public health research. Annu Rev Public Health 21:171–192
Acknowledgments
The authors wish to thank Dr. Adolfo Hernandez-Garduño for his thorough review of the methodology and statistical analysis and Sergio Lozano-Rodriguez, M.D. for his review of the manuscript.
Funding
Consejo Nacional de Ciencia y Tecnología (CONACYT). CONACYT-Salud 2007-C01-69439, CONACYT-Salud 2007-C01 69765 and the Fundación Mexicana para Enfermos Reumáticos (FUMERAC) who receives unconditional financial support from Abbot, Novartis, Roche, Sanofi-Aventis, and Schering-Plough.
Contributors
RA-J and PB-I were involved in the conception and design of the study, acquisition of data and/or analysis and interpretation of data; drafting of manuscript and revising it critically for important intellectual content; final approval of the version to be published. MM-J, AN-J,GR-MV,SL-H, BV-R,GE-M,MM, CM-H were involved in the conception of the study; drafting of manuscript and revising it critically for important intellectual content; final approval of the version to be published. MMJ, PB-I performed the biostatistical analysis.
Conflict of interest
Dr. Burgos-Vargas has received grant/research support from Abbvie; has been a consultant for Abbvie, Bristol Myers Squibb, Janssen, Pfizer, Roche, UCB; and participated as a speaker for Abbvie, BMS, Janssen, MSD, Pfizer, Roche, UCB. Dr. Cardiel has received honoraria for consultations and/or speaking for Pfizer, Lilly, Bristol Myers Squibb, and GSK. Dr. Garza-Elizondo has been a consultant and/ or speaker for MSD, Pfizer, Bristol Myers Squibb, and UCB.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
(GEEMA) Grupo de Estudio Epidemiológico de Enfermedades Músculo Articulares
Jorge A. Esquivel Valerio, Hospital Universitario “Dr. Jose Eleuterio Gonzalez”, Monterrey, Nuevo Leon; Jorge A. Zamudio Lerma,Hospital General de Culiacan, Secretaria de Salud Sinaloa; Natalia Santana Portillo, Instituto Mexicano del Seguro Social, Chihuahua.
Rights and permissions
About this article
Cite this article
Rodriguez-Amado, J., Moreno-Montoya, J., Alvarez-Nemegyei, J. et al. The Social Gap Index and the prevalence of osteoarthritis in the community: a cross-sectional multilevel study in Mexico. Clin Rheumatol 35, 175–182 (2016). https://doi.org/10.1007/s10067-014-2776-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-014-2776-y