Abstract
The objective is to investigate the accrual rate and risk factors of chronic kidney disease (CKD) in an inception cohort of patients with systemic lupus erythematosus (SLE) followed at a single tertiary center. A prospectively collected database of 256 consecutive patients with SLE followed over a 25-year period was systematically interrogated for demographic, disease manifestations, co-morbidities, and outcome. Standardized SLE activity and damage scores were determined for the first and last study visits, and estimated glomerular filtration rate (eGFR; MDRD formula) was calculated at the time of diagnosis and at each year of the follow-up. CKD was defined as eGFR <60 ml/min/1.73 m2. Results were analyzed with univariate and multivariate models and Kaplan-Meier curves, as appropriate. The cohort was predominantly female (90 %) and Jewish (91.1 %). Mean age at diagnosis was 38 ± 15.5 years, mean SLE activity score 6.4 ± 3.8, mean disease duration 8.8 ± 6.6 years, and mean damage score 0.2 ± 0.6. Seventy-five patients (30.8 %) were diagnosed with American College of Rheumatology (ACR)-defined lupus renal disease during the study period. There was a progressive decrease in eGFR over time. The prevalence of CKD was 46.7 % in patients with ACR-defined renal lupus disease and 16.4 % in those without. The hazards ratio for CKD was significantly higher in patients with lupus nephritis (LN) than without (p < 0.001). Earlier CKD was positively associated with hypertension (p = 0.01), older age at diagnosis (p = 0.01), and LN (p < 0.001), and negatively associated with hydroxychloroquine treatment (p < 0.001). The prevalence of CKD increases cumulatively in patients with SLE, also in those without overt lupus renal disease. Lupus renal disease poses a significant hazard for earlier development of CKD, and hypertension is a major risk factor for patients with and without nephritis. Antimalarial treatment is associated with renal preservation only in patients with lupus nephritis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic kidney disease (CKD) is defined as a glomerular filtration rate (GFR) below 60 ml/min per 1.73 m2 for 3 months or more, irrespective of the disorder affecting the structure and function of the kidney [1]. Studies have shown that as GFR decreases, the prevalence and severity of cardiovascular disease (CVD) increase: Patients with stages III–IV CKD have a 4- to 5-fold higher prevalence of CVD than the general population [2, 3]. Furthermore, patients with CKD are known to be affected by diabetes, hypertension, and obesity—all traditional risk factors for CVD in the general population [4, 5].
Systemic lupus erythematosus (SLE) is a chronic multisystem autoimmune disorder affecting predominantly young women [6]. Lupus nephritis (LN) is a common manifestation, with reported rates of 50–70 % of patients [7]. It can lead to end-stage renal disease (ESRD) and is associated with a high rate of CVD [8] and an increased risk of death [9, 10]. Although the presence of proteinuria and/or decreased renal function in patients with SLE is generally attributed to LN, studies have reported many other types of kidney disorders, unrelated to nephritis, in this patient population [11]. The long-term course of renal function in patients with SLE without LN was not well studied. Prompted by the effect of CVD on morbidity and mortality in patients with SLE [8], we conducted the present study to determine the accrual time, risk factors, and outcome of CKD in a hospital-based inception cohort of patients with SLE, with or without overt lupus renal disease (LRD), attending a single major tertiary medical center.
Patients and methods
We have interrogated a prospectively collected hospital-based database of SLE patients attending the Lupus Clinic at Rabin Medical Center, a university-affiliated tertiary hospital in central Israel. A total of 256 consecutive patients diagnosed with SLE were included in the study. All patients fulfilled four or more of the SLE classification criteria of the American College of Rheumatology (ACR) [12, 13] at inception (at the time of or within 12 months prior to diagnosis) and underwent continuous follow-up every 3–6 months from diagnosis at our Lupus Clinic from January 1985 to December 2010.
The source of data for the study comprises hospital’s patient charts as well as a computerized system (OFEK) that integrates hospital-community medical information and serves as a virtual medical file, enabling online communication between the various service providers (hospitals, community clinics, laboratories, imaging, etc.) [14]. Our database consists demographic data, lupus-related disease manifestations, and co-morbidities prospectively collected for baseline and each follow-up visit. At each clinic visit, information related to lupus was prospectively obtained and immediately converted by the examining physician into 25 medical history and 29 physical examination variables. At each visit, patients also underwent a laboratory work-up including erythrocyte sedimentation rate, C-reactive protein level, complete blood count, and level of serum creatinine, total protein, and albumin. In patients with urine protein ≥30 mg/dl on urinalysis, a 24-h urine assay was performed for creatinine and protein excretion. Sera were assayed at each visit for anti-double strand DNA antibody (Farr method) and complement level (C3, C4, complement hemolysis-100). At diagnosis, patients were tested for antinuclear antibody (ANA; by immunofluorescence), anti-Smith (Sm), Ro, La, ribonucleaoprotein (RNP), cardiolipin, and β2-glycoprotein I IgG, IgM, and IgA antibodies (by ELISA), as well as lupus anticoagulant. All laboratory tests were done by commercial methods at the hospital’s laboratory.
For the purpose of this study, data on the use of hydroxychloroquine (HCQ), corticosteroids, cyclophosphamide, mycophenolate mofetil (MMF), rituximab, statins, angiotensin converting enzyme inhibitor (ACEI) or angiotensin receptor blocker (ARB) for 3 months or more was collected. The SLE Disease Activity Index 2000 (SLEDAI-2K) [15] and the Systemic Lupus International Collaborating Clinics (SLICC)/ACR Damage Index (SDI) [16] were retrospectively determined for the first and last visits of the study period.
LRD was defined by the ACR criteria for the classification of SLE [13] and/or by kidney biopsy findings compatible with LN, unless there was an evidence for a non-lupus cause for renal disease. The estimated GFR (eGFR) was retrospectively calculated for each patient for the first visit, for each year of follow-up, and for the last visit of the study period using the Modification of Diet in Renal Disease (MDRD) equation [17], which has been validated for estimation of GFR in patients with SLE [18]. CKD was defined as an eGFR of <60 ml/min/1.73 m2 for at least 3 months. Accordingly, kidney damage was classified into five stages: >90 ml/min/1.73 m2 (stage 1), 60–89 ml/min/1.73 m2 (stage 2, mild CKD), 30–59 ml/min/1.73 m2 (stage 3, moderate CKD), 15–29 ml/min/1.73 m2 (stage 4, severe CKD), and <15 ml/min/1.73 m2 (stage 5, ESRD) [1]. ACR-defined LRD was defined if urine protein excretion was ≥500 mg/24 h with or without hematuria (>5 RBC/HPF) and/or urinary casts on two consecutive visits for at least a 3-month period and/or if a kidney biopsy result was compatible with the WHO definition of LN (class I, normal or minimal disease; II, mesangial nephritis; III, focal proliferative nephritis; IV, diffuse proliferative nephritis; V, membranous nephritis) [19]. A kidney biopsy was performed at the attending physician’s discretion according to the common practice for the diagnosis of LN, mainly for the purpose of determining whether therapy with immunosuppressant is indicated for the induction of LN remission. Nephrotic syndrome was defined as 24-h urine protein excretion >3.5 g with plasma albumin <3 g/dl.
Co-morbidities were defined as follows: arterial hypertension, defined as systolic blood pressure >140 mmHg and diastolic pressure >90 mmHg requiring antihypertensive medications; hyperlipidemia, defined as serum total cholesterol >200 mg/dl and/or triglycerides >150 mg/dl and/or anti-lipidemic drug use; diabetes mellitus (DM), defined as hyperglycemia requiring previous or ongoing pharmacologic therapy; and CVD, defined as evidence of ischemic heart disease and/or ischemic stroke and/or peripheral vascular disease. Ischemic heart disease was defined as evidence of myocardial infarction and/or evidence of coronary atherosclerosis and/or evidence of a percutaneous coronary intervention procedure or aortocoronary bypass surgery; stroke was defined as evidence of a neurological deficit and/or signs of a brain infarct on computed tomography or magnetic resonance imaging; and peripheral vascular disease was defined as evidence of peripheral artery atherosclerotic stenosis or occlusion on angiography and/or Doppler sonography and/or evidence of peripheral artery bypass surgery. Due to inconsistent recording of smoking throughout the study period, we did not include smoking among the variables of co-morbidity that might affect renal function.
The annual serum creatinine and eGFR values were evaluated against the demographic, clinical, and serological findings, co-morbidities, and drug use to determine the accrual of CKD and the risk factors associated with deterioration of renal function, for the whole cohort and by presence or absence of ACR-defined LRD [13] and biopsy-proven LN [19].
The study was approved by the hospital institutional review board.
Statistical analysis
All calculations were performed using the SPSS (version 15.0). Results were expressed as mean ± standard deviation (SD). Nominal data were compared with the chi-square test. Renal survival analysis was performed using the Kaplan-Meier method. Log rank Mantel-Cox test was used to test differences between groups, and Cox proportional hazards (hazard ratio, HR) regression analysis was used to adjust renal survival by different covariates. Probability values less than or equal to 0.05 were considered statistically significant.
Results
Baseline demographic, clinical, and laboratory profiles
The study group of 256 consecutive patients with SLE consisted of 230 women (90 %) and 25 men (10 %); 91.1 % were Jewish and 8.9 % Arabic. Mean age at SLE diagnosis was 38.1 ± 15.9 years (range 10–79 years) and at the last study visit 49.9 ± 15.9 years (range 20–93) and mean education was 12.8 ± 2.4 years (range 7–20 years). Mean duration of follow-up was 8.5 ± 6.1 years (range 1–25 years): 15 patients (6 %) were followed for >20 years, 57 patients (22.6 %) for 10–20 years, and 180 patients (71.4 %) for less than 10 years. Table 1 depicts the clinical and laboratory features at inception. The mortality rate during the study period was 11.3 %.
The most often used drugs were hydroxychloroquine by 89.06 % of patients, and corticosteroids by 70.3 %. Statins, 22.7 % and ACEIs or ARBs, 30.8 %. Rates of use of intravenous cyclophosphamide and MMF, administered mostly for treatment of LN, were 15.6 and 3.5 %, respectively. Other drugs included azathioprine in 14.06 % of patients, oral methotrexate in 11.3 %, and intravenous rituximab in 1.9 %.
Chronic kidney disease
Mean serum creatinine level was 0.87 ± 0.38 mg/dl at cohort inception (median 0.8 mg/dl, range 0.4–3.9 mg/dl); 7.8 % of patients had evidence of nephrotic syndrome. The mean eGFR at inception was 91.34 ± 29.64 ml/min/1.73 m2 (median 87.5, range 15.5–207.00 ml/min/1.73 m2). Seventy-five patients (30.8 %) developed evidence of renal involvement according to the ACR criteria [12, 13] and 45 patients (17.9 % of the cohort) had a biopsy-proven LN during the study period. The annual incidence of CKD stage ≥3 in the whole cohort and in the group with biopsy-proven LN was 4 and 7 %, respectively. The histological distribution of LN according to the kidney biopsy findings (WHO classification) was as follows: class I, 2.2 %; class II, 4.4 %; class III, 13.3 %; class IV, 46.7 %; class V, 22.2 %; and mixed type, 11.1 %, mostly proliferative and membranous nephritis. Mean serum creatinine at the last study follow-up visit was 0.95 ± 1.09 mg/dl (median 0.75 mg/dl, range 0.39–11.00 mg/dl), and mean last eGFR was 93.9 ± 35.5 ml/min/1.73 m2 (median 92.3, range 5.9–218.4 ml/min/1.73 m2). CKD stage ≥3 was diagnosed in 42 patients (16.5 %) of our cohort: stage 3 of CKD in 13.2 % [15 patients (8.9 %) with ACR-defined LRD and 17 patients (22.7 %) with biopsy-proven LN]; stage 4, 1.6 % [1 patient (0.6 %) with evidence according to the ACR-defined LRD and 3 patients (4 %) with biopsy-proven LN]; and stage 5, 1.6 % [4 patients (5.3 %) with biopsy-proven LN and none in the patients who had fulfilled the ACR criteria for LRD]. Dialysis was required by 10 patients (3.9 %) of patients, and 6 patients (2.3 %) underwent kidney transplantation during the study period, all with biopsy-proven LN.
Disease features and CKD stage ≥3 in patients with and without ACR-defined renal involvement
In order to evaluate the rate of CKD stage ≥3 in lupus patients who do not have evidence of LRD, we have divided our cohort according to the ACR definition for LRD [13]. Patients with ACR-defined LRD were significantly younger (32.8 ± 13.9 vs. 40.6 ± 15.5 years, p < 0.01), had higher SLEDAI-2K (9.03 ± 4.23 vs. 5.25 ± 2.96, p < 0.01), and had higher level of anti-dsDNA antibody and hypocomplementemia at diagnosis of SLE and had more serositis and psychosis during the study follow-up period and, as expected, were more frequently treated with immunosuppressive and steroid drugs, as well as statins and ACEI/ARB (Tables 2 and 3).
Table 4 depicts renal function parameters according to the ACR definition of LRD [15]. At diagnosis of SLE, serum creatinine of the patients with ACR-defined LRD was higher than of those without evidence of renal disease (1.01 ± 0.61 vs. 0.8 ± 0.19 mg/dl, respectively, p < 0.001), although there was no difference in the mean eGFR (86.8 ± 31.5 vs. 93.3 ± 28.7 ml/min/1.73 m2, respectively, p = 0.13). As expected, at the end of the study follow-up period, patients with ACR-defined LRD had significantly higher serum creatinine than the patients with no evidence of ACR-defined LRD (1.39 ± 1.87 vs. 0.76 ± 0.26 mg/dl, respectively, p < 0.001), lower eGFR (81.9 ± 38.8 vs. 99.3 ml/min/1.73 m2, respectively, p < 0.001), and greater rate of CKD stage ≥3 (eGFR <60 ml/min/1.73 m2) (46.7 vs. 16.4 %, respectively, p < 0.001). Damage accrual scored by SDI [16] was similar in the group of ACR-defined and non-ACR-defined LRD (1.67 ± 2.08 vs. 1.22 ± 2.8, respectively, p = 0.2).
Association of CKD stage ≥3 with biopsy-proven lupus nephritis
As shown in Table 5, CKD stage ≥3 was significantly more prevalent and occurred significantly earlier in patients with histological evidence of LN than in patients without LN (p < 0.001, log rank Mantel-Cox analysis). The 10- and 20-year renal survival (eGFR ≥60 ml/min/1.73 m2) was significantly greater in patients with no biopsy-proven LN than in patients with LN (80.3 ± 4.8 vs. 54.5 ± 6.6 % and 72.7 ± 5.4 vs. 15.0 ± 11.7 %, respectively, p < 0.001, log rank Mantel-Cox analysis).
Risk factors for the development of CKD stage ≥3
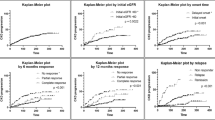
Risk factors for accrual of CKD stage ≥3 for the entire cohort were older age at SLE diagnosis (p = 0.007), increased SDI at diagnosis (p = 0.006), evidence of hypertension (HTN), DM, and CVD at diagnosis (p < 0.001, p = 0.02, p = 0.004, respectively), and diagnosis of LN anytime during the follow-up period (p < 0.001). Adjusted multivariate Cox regression analysis of risk factors for CKD for the entire cohort showed that the hazards ratio for the accrual of CKD were HTN at diagnosis (p < 0.001, HR 6.7, 95 % CI 2.7–16.6) and evidence of LN during the disease course (p = 0.009, HR 3.3, 95 % CI 1.3–7.9). For lupus patients who did not have evidence of ACR-defined LRD, adjusted multivariate Cox regression analysis found only HTN and reduced eGFR at diagnosis as significant risk factors for the accrual of CKD stage ≥3 (p = 0.008 and p < 0.001, respectively). Adjusted multivariate analysis for the 45 patients (17.9 % of the cohort) with biopsy-proven LN showed that an increased risk for the accrual of CKD stage ≥3 was significantly associated with older age at diagnosis (p = 0.001, HR 1.05, 95 % CI 1.02–1.08), worse (class IV and/or V) WHO class of LN (p < 0.001, HR 16.01, 95 % CI 5.9–43.1), and evidence of HTN or DM at SLE diagnosis (p = 0.01, HR 2.9, 95 % CI 1.2–6.9, and p = 0.03, HR 4.1, 95 % CI 1.1–15.1, respectively). As depicted in Table 5, the cumulative proportion of renal survival, defined as eGFR >60 ml/min/1.73 m2, was significantly greater for lupus patients without evidence of LN than for those with LN (p < 0.001). Figure 1 shows the cumulative renal survival (eGFR >60 ml/min/1.73 m2) of patients with and without ACR-defined LRD. On Kaplan-Meier analysis (Fig. 1), mean time from SLE diagnosis to measurement of eGFR <60 ml/min/1.73 m2 was highly significantly shorter for patients with ACR-defined LRD than in patients without during the study period (p < 0.001). Male patients had a higher rate of CKD than female patients, but the difference did not reach a statistical significance (p = 0.06, log rank Mantel-Cox analysis). The SLEDAI-2K score at inception was not associated with a higher risk of CKD accrual. None of the auto-antibodies tested, including anti-dsDNA and antiphospholipid antibodies, or complement level at inception, had a significant effect on the occurrence of CKD in the whole cohort.
Association of drugs use with CKD stage ≥3 development
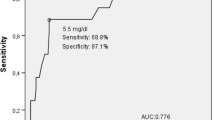
Treatment with HCQ was significantly associated with a lower risk of CKD stage ≥3 in the whole group (p = 0.02, HR 0.4, 95 % CI 0.2–0.9) (Fig. 2). On adjusted multivariate Cox regression analysis, HCQ did not have a protective effect in patients without ACR-defined lupus renal disease. Corticosteroids, cyclophosphamide, azathioprine, MMF, statins, and ACEIs/ARBs did not exert a protective effect in terms of CKD accrual rate during follow-up.
Discussion
CKD stage ≥3 is a common public health problem worldwide, associated with an increased risk of renal failure, CVD, and mortality [1–5]. Given that CVD is a leading cause of morbidity and mortality in patients with SLE [19, 20], and CKD stage ≥3 is a major contributor to the evolution of CVD in patients without SLE [1–5], we sought to determine the causes and prevalence of CKD stage ≥3 in a large inception cohort with SLE followed for up to 25 years and compare the evolution and outcome of CKD stage ≥3 in patients with and without evidence of ACR-defined LRD [13] or biopsy-proven LN [19]. The main findings were as follows: CKD stage ≥3 is a major disease burden in lupus patients with overt renal disease as has been previously shown [6, 7]; however, the accrual of CKD stage ≥3 in SLE increases cumulatively over time also in patients without ACR-defined LRD and/or biopsy-proven LN (Table 5 and Fig. 1). The main underlying factor for the deterioration of renal function for lupus patients with and without evidence of ACR-defined LRD is hypertension as well as older age at SLE diagnosis. Treatment with HCQ exerts a protective effect in patients with LN, but not on renal survival of patients with no overt LRD. Neither SLE activity nor lupus-specific auto-antibodies at diagnosis had an impact on renal outcome.
CKD stage ≥3 was diagnosed in 30.8 % of our whole cohort after a mean follow-up period of 8.8 ± 6.5 years; in 1.6 % of the cohort, CKD evolved to ESRD (stage 5, eGFR <15 ml/min/1.73 m2 or dialysis) and occurred only in patients who were diagnosed with ACR-defined LRD. Moreover, as seen in Table 5, renal survival defined as normal or mildly decreased renal function (eGFR >60 ml/min/1.73 m2) was significantly higher in lupus patients who did not have evidence of LN, and the decline of eGFR after 15 years or more of follow-up was observed solely in those with biopsy-proven LN (Table 5; p < 0.001). These findings reconfirm the grave prognostic implication of LN on the evolution of CKD stage ≥3 and ESRD in SLE [9, 10, 21–28]. The causes and outcome of CKD stage ≥3 in SLE patients without LRD was not widely studied. A recent study of a Canadian inception cohort comprised Caucasian, African Caribbean, and Chinese patients found a rate of CKD stage ≥3 in only 5 % of those without ACR-define LRD that was associated with older age and renal insufficiency at enrollment. In our cohort, the prevalence of CKD stage ≥3 was 46.7 % in patients with ACR-defined LRD and 16.4 % in those without after a long follow-up period, higher than in the Canadian cohort [27]. Our long-term study adds to these data showing the occurrence of CKD rises over time also in patients with SLE without overt LRD, albeit at a significantly lower rate than in patients with LN (Fig. 1).
CKD stage ≥3 affects 10 to 15 % of adults in the general population in the USA, Europe, and Asia [29–31], and the prevalence increases dramatically with age (from 4 % at age 20–39 to 47 % at age ≥70 years in the USA) [29]. Taken into account the relatively young age at inception of our lupus patients, a rate of CKD stage ≥3 of 16.4 % in the group of patients with SLE without overt LRD is higher than expected in an age-adjusted general population [29] and emphasizes the health burden of CKD stage ≥3 in SLE patients even without overt LRD. Arterial hypertension was evident in 11.4 % of our patients despite their relatively young age at diagnosis and was found to be a significant risk factor for the evolution of CKD stage ≥3 in our cohort in patients with and without ACR-defined LRD. Other risk factors for the development of CKD stage ≥3 in SLE were older age and overt LN (Tables 2 and 3). Numerous studies have reported a high prevalence of hypertension in women with SLE—up to 74 % in some cohorts—compared to the age- and sex-matched general population [21, 32–34]. The mechanisms that contribute to SLE hypertension are likely multifactorial and involve cytokine-mediated renal vascular resistance and reduced GFR, as well as metabolic and drug effects [34]. Our results strengthen the importance of early recognition and tight control of hypertension in patients with SLE even in the absence of overt renal disease.
HCQ intake was inversely associated with CKD stage ≥3 development in patients with LN (p < 0.001; Fig. 2), suggesting a protective effect of antimalarial drugs for renal survival. Antimalarials have been shown to prevent lupus flares [31, 35] and reduce accrual of chronic damage [36, 37], as well as decrease the mortality rate in SLE [37–39]. Additionally, in patients with LN, administration of antimalarials retarded the onset of renal damage [40], extended renal remission during concomitant MMF treatment [41], and improved renal outcome [42, 43]. The benefit of HCQ with respect to the evolution of CKD in our patients was significant for those with LN, suggesting that antimalarials exert a specific anti-inflammatory effect on the immune-mediated renal damage. Indeed, a recent study showed that the mechanism underlying the anti-inflammatory effects of antimalarial drugs in SLE involves the inhibition of toll-like receptor (TLR)-9-mediated innate immune activation along with inhibition of inflammatory cytokines production [44]. Accordingly, several authors reported glomerular upregulation of TLR-9 in kidneys of patients with LN [45, 46]. Our results, together with previously published data, strongly support the use of antimalarials in all patients diagnosed with SLE.
Our study was limited by its retrospective design, although the patients’ data were prospectively collected, and all included patients were diagnosed, treated, and continuously followed exclusively at our hospital.
In summary, the prevalence of CKD stage ≥3 in patients with SLE with no evidence of ACR-defined LRD rises along the course of the disease, especially in the presence of concomitant hypertension, and exceeds the expected rate of CKD in the general population. Treatment with antimalarial drugs such as HCQ is associated with renal preservation in patients with LN, but does not protect from renal function decline in patients without LRD. Our results of high rate and earlier occurrence of CKD stage ≥3 among SLE patients without overt renal involvement and given the prognostic effects of CKD stage ≥3 with respect to the development of CVD and overall mortality, strengthen the importance of improving the surveillance of CKD stage ≥3 and vigorous treatment of hypertension in patients with SLE.
References
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group (2013) KDIGO clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 3:1–150
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY (2004) Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 351:1296–1305
Culleton BF, Larson MG, Wilson PW, Evans JC, Parfrey PS, Levy D (1999) Cardiovascular disease and mortality in a community-based cohort with mild renal insufficiency. Kidney Int 56:2214–2219
Sarnak MJ, Levey AS, Schoolwerth AC, American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention et al (2003) Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation 108:2154–2169
Goicoechea M, de Vinuesa SG, Gómez-Campderá F, Luño J (2005) Predictive cardiovascular risk factors in patients with chronic kidney disease (CKD). Kidney Int Suppl 93:S35–S38
D’Cruz DP, Khamashta M, Hughes GR (2007) Systemic lupus erythematosus. Lancet 369:587–596
Seshan SV, Jennette JC (2009) Renal disease in systemic lupus erythematosus with emphasis on classification of lupus glomerulonephritis. Advances and implications. Arch Pathol Lab Med 133:233–248
Zhang W, Agheh E, Reich HN et al (2011) Glomerular filtration rate predicts arterial events in women with systemic lupus erythematosus. Rheumatology 50:799–805
Croca SC, Rodrigues T, Isenberg D (2011) Assessment of a lupus nephritis cohort over a 30-year period. Rheumatology 50:1424–1430
Faurschou M, Dreyer L, Kamper AL, Starklint H, Jacobsen S (2010) Long-term mortality and renal outcome in a cohort of 100 patients with lupus nephritis. Arthritis Care Res 62:873–880
Baranowska-Daca E, Choi YJ, Barrios R, Nassar G, Suki WN, Truong LD (2001) Nonlupus nephritides in patients with systemic lupus erythematosus: a comprehensive clinicopathologic study and review of the literature. Hum Pathol 32:1125–1135
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40:1725
Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfield NF (1982) The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 25:1271–1277
Nirel N, Rosen B, Sharon A, Blondheim O, Sherf M, Samuel H, Cohen AD (2010) The impact of an integrated hospital-community medical information system on quality and service utilization in hospital departments. Int J Med Inform 79:649–657
Gladman DD, Ibanez D, Urowitz MB (2002) Systemic Lupus Erythematosus Disease Activity Index 2000. J Rheumatol 29:288–291
Gladman DD, Urowitz MB, Goldsmith CH et al (1997) The reliability of the Systemic Lupus International Collaborating Clinics/American College of Rheumatology Damage Index in patients with systemic lupus erythematosus. Arthritis Rheum 40:809–813
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D, Modification of Diet in Renal Disease Study Group (1999) A more accurate method to estimate glomerular filtrating rate from serum creatinine: a new prediction equation. Ann Intern Med 130:461–470
Leung YY, Lo KM, Szeto CC, Li EK, Kun EW (2006) Estimation of glomerular filtration rate in patients with systemic lupus erythematosus. Lupus 15:276–281
Austin HA, Muenz LR, Joyce KM et al (1983) Prognostic factors in lupus nephritis. Contribution of renal histologic data. Am J Med 75:382–391
Ward MM (1999) Premature morbidity from cardiovascular and cerebrovascular diseases in women with systemic lupus erythematosus. Arthritis Rheum 42:338–346
McMahon M, Hahn BH, Skaggs BJ (2011) Systemic lupus erythematosus and cardiovascular disease: prediction and potential for therapeutic intervention. Expert Rev Clin Immunol 7:227–241
Mok CC (2005) Prognostic factors in lupus nephritis. Lupus 14:39–44
Donadio JV Jr, Hart GM, Bergstralh EJ, Holley KE (1995) Prognostic determinants in lupus nephritis: a long-term clinicopathologic study. Lupus 4:109–115
Mok CC, Wong RW, Lau CS (1999) Lupus nephritis in southern Chinese patients: clinicopathologic findings and long-term outcome. Am J Kidney Dis 34:315–323
Korbet SM, Lewis EJ, Schwartz MM, Reichlin M, Evans J, Rohde RD, Lupus Nephritis Collaborative Study Group (2000) Factors predictive of outcome in severe lupus nephritis. Am J Kidney Dis 35:904–914
Austin HA III, Boumpas DT, Vaughan EM, Balow JE (1995) High-risk features of lupus nephritis: importance of race and clinical and histological factors in 166 patients. Nephrol Dial Transplant 10:1620–1628
Esdaile JM, Federgreen W, Quintal H, Suissa S, Hayslett JP, Kashgarian M (1991) Predictors of one year outcome in lupus nephritis: the importance of renal biopsy. Q J Med 81:907–918
Reich HN, Gladman DD, Urowitz MB et al (2011) Persistent proteinuria and dyslipidemia increase the risk of progressive chronic kidney disease in lupus erythematosus. Kidney Int 79:914–920
Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, Van Lente F, Levey AS (2007) Prevalence of chronic kidney disease in the United States. JAMA 298(17):2038–2047
Hallan SI, Coresh J, Astor BC, Asberg A, Powe NR, Romundstad S, Hallan HA, Lydersen S, Holmen J (2006) International comparison of the relationship of chronic kidney disease prevalence and ESRD risk. J Am Soc Nephrol 17(8):2275–2284
Zhang L, Zhang P, Wang F, Zuo L, Zhou Y, Shi Y, Li G, Jiao S, Liu Z, Liang W, Wang H (2008) Prevalence and factors associated with CKD. Am J Kidney Dis 51(3):373–384
Al-Herz A, Ensworth S, Shojania K, Esdaile JM (2003) Cardiovascular risk factor screening in systemic lupus erythematosus. J Rheumatol 30:493–496
Budman DR, Steinberg AD (1976) Hypertension and renal disease in systemic lupus erythematosus. Arch Intern Med 136:1003–1007
Ryan MJ (2009) The pathophysiology of hypertension in systemic lupus erythematosus. Am J Physiol Regul Integr Comp Physiol 296:R1258–R1267
Molad Y, Gorshttein A, Wysenbeek AJ et al (2002) Protective effect of hydroxychloroquine in systemic lupus erythematosus. Prospective long-term study of an Israeli cohort. Lupus 11:356–361
Esdaile J (1991) For the Canadian Hydroxychloroquine Study Group. A randomized study of the effect of withdrawing hydroxychloroquine sulfate in systemic lupus erythematosus. N Engl J Med 324:150–154
Fessler BJ, Alarcón GS, McGwin G Jr, LUMINA Study Group et al (2005) Systemic lupus erythematosus in three ethnic groups. XVI. Association of hydroxychloroquine use with reduced risk of damage accrual. Arthritis Rheum 52:1473–1480
Alarcon GS, McGwin G, Bertoli AM, LUMINA Study Group et al (2007) Effect of hydroxychloroquine on the survival of patients with systemic lupus erythematosus: data from LUMINA, a multiethnic US cohort (LUMINA L). Ann Rheum Dis 66:1168–1172
Ruiz-Irastorza G, Khamashta MA (2008) Hydroxychloroquine: the cornerstone of lupus therapy. Lupus 17:271–273
Pons-Estel GJ, Alarcón GS, McGwin G Jr, Lumina Study Group (2009) Protective effect of hydroxychloroquine on renal damage in patients with lupus nephritis. LXV. Data from a multiethnic US cohort. Arthritis Rheum 61:830–839
Kasitanon N, Fine DM, Haas M, Magder LS, Peti M (2006) Hydroxychloroquine use predicts complete renal remission within 12 months among patients treated with mycophenolate mofetil therapy for membranous lupus nephritis. Lupus 15:366–370
Sisó A, Ramos-Casals M, Bové A et al (2008) Previous antimalarial therapy in patients diagnosed with lupus nephritis: influence on outcomes and survival. Lupus 17:281–288
Sisó A, Ramos-Casals M, Bové A et al (2010) Outcomes in biopsy-proven lupus nephritis: evaluation of 190 white patients from a single center. Medicine (Baltimore) 89:300–307
Kuznik A, Bencina M, Svajger U, Jeras M, Rozman B, Jerala R (2011) Mechanism of endosomal TLR inhibition by antimalarial drugs and imidazoquinolines. J Immunol 186:4794–4804
Papadimitraki ED, Tzardi M, Bertsias G, Sotsiou E, Boumpas DT (2009) Glomerular expression of toll-like receptor-9 in lupus nephritis but not in normal kidneys: implications for the amplification of the inflammatory response. Lupus 18:831–835
Frieri M, Samih MA, Dzhindzhikhashvili M, Liu H, Balsam L, Rubinstein S (2012) Toll-like receptor 9 and vascular endothelial growth factor levels in human kidneys from lupus nephritis patients. J Nephrol 25:1041–1046
Conflicts of interest
The authors declare no conflicts of interest.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pokroy-Shapira, E., Gelernter, I. & Molad, Y. Evolution of chronic kidney disease in patients with systemic lupus erythematosus over a long-period follow-up: a single-center inception cohort study. Clin Rheumatol 33, 649–657 (2014). https://doi.org/10.1007/s10067-014-2527-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-014-2527-0