Abstract
Clinical characteristics of antitumor necrosis factor (TNF) agents-related tuberculosis (TB) in ankylosing spondylitis (AS) are not well described. The aim was to compare the incidences and the characteristics of TB in AS and rheumatoid arthritis (RA) during TNF inhibitor treatment. AS (n = 1,322) and RA (n = 3,154) patients who received medical care between January 2001 and August 2011 were enrolled. The incidence of TB in patients treated, or not, with TNF inhibitors and the clinical features associated with TB were explored. Seven patients with AS and seven with RA developed TB while receiving TNF inhibitor therapy, resulting in an incidence rate of 600.2/100,000 person-years (PYs) (95 % confidence interval (CI), 241.3–1236.3) for those with AS and 771.6/100,000 PYs (95 % CI, 310.2–1589.9) for those with RA. Incidence rate ratios for TNF inhibitor-treated vs. untreated patients were 4.87 for AS (95 % CI, 1.50–15.39; p < 0.001) and 3.61 for RA (95 % CI, 1.38–8.07; p < 0.001). Low body mass index was identified as a significant risk factor for TB in the AS group (odds ratio (OR), 13.0; p = 0.002). Extrapulmonary TB was predominant at 85.7 % during TNF inhibitor treatment. Three (42.8 %) of the AS patients, but none of the RA patients, developed TB with concomitant isoniazid. All AS patients recovered from TB whereas two of seven RA patients died. Treatment with TNF inhibitors significantly increases the risk of extrapulmonary TB in AS. Symptoms of infection should warrant clinicians to evaluate for TB during TNF inhibitor therapy in AS patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tumor necrosis factor (TNF) plays an important role in the pathogenesis of ankylosing spondylitis (AS) and rheumatoid arthritis (RA). As such, treatments aimed at antagonizing TNF improved significantly the outcome of AS and RA [4, 6, 23, 25]. However, TNF also plays a critical role in immune defense against infections, including tuberculosis (TB); thus, the increasing use of TNF inhibitors has led to a marked increase in the incidence of TB [27, 29]. Particularly, in TB endemic areas including South Korea, TB incidence during TNF inhibitor use has been estimated as considerably high [10, 17]. RA patients usually develop TB within 1 year of beginning TNF inhibitor treatment which often manifests as an extrapulmonary infection [2, 5, 7, 10, 12, 14]. Data on TB incidence in AS during TNF inhibitor use remain scarce to date.
Although AS and RA share the joints at the main site of inflammation, they differ in several clinical features; AS primarily affects axial joints with profound bone formation, whereas RA primarily affects the small peripheral joints with bone erosion [20, 24]. Furthermore, AS patients tend to be younger and to have fewer comorbidities. AS is tightly associated with HLA-B27, lacks disease-specific autoantibodies, and is minimally responsive to traditional disease-modifying antirheumatic drugs (DMARDs) including methotrexate (MTX); the mechanism underlying immunologic dysregulation appears to differ from that in RA [3, 20]. Therefore, we speculate that the incidence of TB may differ between AS and RA patients during TNF inhibitor therapy.
The aim of the present study was to investigate the incidence and clinical characteristics of TB in AS and RA patients receiving TNF inhibitors.
Patients and methods
Patients
We enrolled all of the AS (n = 336) and RA patients (n = 222) who started anti-TNF agents (etanercept, infliximab, adalimumab, golimumab, and certorlizumab) at our institution between January 2001 and August 2011. Detailed medical history was obtained by reviewing electronic medical records. AS (n = 986) and RA (n = 2,932) patients who never took anti-TNF agents during the same period were recruited as control groups. All patients met the 1987 RA classification criteria or the 1984 modified New York criteria for AS [1, 26]. Where a patient was treated with two or more TNF inhibitors, the last TNF inhibitor used before the onset of TB was regarded as the causative agent.
Follow-up was censored at the most recent follow-up or death, whichever came first. The study protocol was approved by the institutional review board of Seoul National University Hospital.
TB diagnosis
TB infection was diagnosed according to the presence of fever, night sweats, weight loss, anorexia, coughing, and/or hemoptysis in conjunction with evidence of infection by Mycobacterium tuberculosis. Such evidence included a positive acid-fast bacillus culture, a positive TB polymerase chain reaction result, the presence of caseating granulomas on biopsy, and/or a clinical improvement upon anti-TB treatment. The TB infection site was categorized as pulmonary or extrapulmonary based on imaging and/or tissue biopsy of the involved organs.
Latent TB infection (LTBI) was diagnosed according to the Korean guidelines for TB: a positive TB skin test (TST) with induration diameter ≥10 mm or a positive interferon-γ release assay (IGRA) plus a normal chest X-ray [21]. Also, patients with an abnormal chest radiograph such as apical fibronodular changes and irregular linear opacities without a sign of active infection and a history of inadequate TB treatment were considered to have a LTBI. Of note, the status of prior Bacille Calmette–Guérin (BCG) vaccination was not be considered when diagnosing a LTBI.
Statistical analysis
The TB incidence rate was expressed as the number of cases per 100,000 person-years (PYs). The 95 % confidence interval (CI) was calculated by assuming that the number of TNF inhibitor-treated patients with TB followed a Poisson distribution. The incidence rate ratio was calculated by dividing the TB incidence rate in TNF inhibitor-treated patients by that in TNF inhibitor-naïve patients. The cumulative rates were estimated using the Kaplan–Meier method, and the incidence rates were compared using log-rank test.
Chi-squared test or Fisher’s exact test (for categorical variables) was used to examine the risk factors associated with TB, and Student’s t test or Mann–Whitney U test (for continuous variables) was used as appropriate to compare the characteristics between AS and RA groups. Risk factors identified by univariate analyses with a significance level of p < 0.20 were included in multivariate logistic regression analysis. All statistical analyses were performed using SPSS 19.0 for Windows (IBM SPSS Inc., Chicago, IL, USA).
Results
Patient characteristics
A total of 1,322 AS patients were identified, of whom 336 (25.4 %) received anti-TNF therapy. Of the 3,154 RA patients identified, only 222 (7.0 %) received anti-TNF therapy (Table 1). Compared with the RA patients, the AS patients were younger, predominantly male, and were treated less frequently with DMARDs and glucocorticoids. In addition, the AS patients tended to have fewer comorbidities (Table 1).
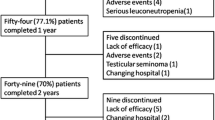
Overall, 336 AS patients were treated with 404 anti-TNF agents: 58 (17.3 %) patients were treated with two anti-TNF agents or more. One hundred sixty-three (40.3 %) patients received etanercept, 150 (37.1 %) received adalimumab, 78 (19.3 %) received infliximab, and 13 (3.2 %) received golimumab. For the RA patients, 277 anti-TNF agents were prescribed: 137 patients (49.5 %) received etanercept, 75 (27.1 %) received adalimumab, 50 (18.1 %) received infliximab, 10 (3.6 %) received golimumab, and 5 (1.8 %) received certorlizumab. Forty-nine (22.1 %) patients were treated with more than one anti-TNF agent. The median follow-up time was 31.2 months (range, 15.8–51.6) for the AS patients and 31.9 months (range, 17.4–59.8) for the RA patients.
TB incidence during TNF inhibitor treatment
Seven AS patients developed TB during 1,166.3 PYs of follow-up, with an incidence of 600.2/100,000 PYs (95 % CI, 241.3–1,236.6). Similarly, seven RA patients were diagnosed with TB during 907.2 PYs of follow-up, with an incidence of 711.6 per 100,000 PYs (95 % CI, 310.2–1589.9). Of note, the incidence of TB among TNF inhibitor-naïve AS and RA patients was 123.1/100,000 PYs and 213.2/100,000 PYs, respectively. Therefore, the use of TNF inhibitors led to a 4.9-fold (95 % CI, 1.5–15.4, p < 0.001) increase in the incidence of TB in AS and a 3.6-fold (95 % CI 1.4–8. 1, p < 0.001) increase in RA (Table 2).
There was no difference in the cumulative incidence of TB between AS and RA patients receiving TNF inhibitors (p = 0.519) (Fig. 1). Also, the incidence of TB did not differ between AS (p = 0.654) and RA (p = 0.232) patients treated with different TNF inhibitors. The median time between TB infection and treatment with anti-TNF agents was similar for AS patients and RA patients (19.4 (95 % CI, 1.9–57.8) months vs. 7.9 (95 % CI, 4.0–36.1) months; p = 0.406).
LTBIs were diagnosed in 104 (30.9 %) AS and in 56 (25.2 %) RA patients prior to anti-TNF commencement. In accordance with the Korean guidelines for TB, all LTBI patients received anti-TB medication for 6–9 months. Despite the prescription of LTBI treatment, 3/104 (2.9 %) AS patients with LTBI developed TB whereas none of 56 RA patients with LTBI developed TB (p = 0.21).
Clinical characteristics of TB in patients treated with TNF inhibitors
Both disease duration and comorbidities such as diabetes mellitus, malignancy, hypertension, hospitalization, chronic renal disease, osteoporosis, gastrectomy/peptic ulcer, smoking, and chronic obstructive pulmonary disease were similar between AS and RA patients (Table 3).
AS patients with TB had a lower body mass index (BMI) than those without TB (19.9 ± 2.6 vs. 23.6 ± 6.4; p = 0.008) (Table 3). A low BMI (<22 kg/m2) increased the risk of TB by 13-fold (95 % CI, 1.5–111.9) (Table 4).
TNF inhibitor-treated RA patients with TB were older (65.1 ± 3.1 vs. 51.4 ± 12.6 years; p = 0.001). Age >60 was associated with a 15.9-fold increase in the TB risk (95 % CI, 1.8–147.6). Furthermore, for RA patients, hospitalization during TNF inhibitor treatment was associated with a higher incidence of TB (odds ratio (OR) 11.54, 95 % CI 2.1–64.5, p = 0.005) (Table 4). Unlike for AS patients, a low BMI was not associated with TB in RA.
TB outcome
Extrapulmonary TB was the predominant form diagnosed in AS and RA patients treated with TNF inhibitors. Six of the seven AS patients (85.7 %) developed extrapulmonary TB; the disease in five patients involved the pericardium (n = 1), larynx (n = 2), or pleura (n = 2); one developed a disseminated TB. Three out of the seven AS patients were hospitalized due to TB, but all recovered well with no long-term complications.
Of the six of seven (85.7 %) RA patients that developed extrapulmonary TB, the disease involved the peritoneum (n = 2), pleura (n = 1), and lymph node (n = 1) in four patients; the other two suffered disseminated TB. In contrast to AS, six of seven RA patients with TB required hospitalization. Three were treated in the intensive care unit for respiratory failure. Two of these patients died.
Discussion
To the best of our knowledge, this is the first study to show that the TB incidence in AS and RA patients receiving anti-TNF treatment is similar. While extrapulmonary TB was prevalent in both AS and RA patients, the TB in AS appeared to have better outcome.
The similar TB incidence in AS and RA patients during anti-TNF treatment was surprising, since AS patients were generally younger, had fewer comorbidity, and took immunosuppressants infrequently. Indeed, the TB incidence in the TNF inhibitor-naïve AS patients appeared to be lower compared to TNF inhibitor-naïve RA patients (123/100,000 PYs vs. 213/100,000 PYs; p = 0.146). TNF inhibitors tended to increase the TB risk in AS to a greater extent than in RA (OR, 4.87 vs. 3.61; p = 0.637). This suggests that anti-TNF therapy can outweigh conventional risk factors of TB in AS and RA. This is in contrast to a previous report that anti-TNF agents did not increase the incidence of TB infection in AS patients in Korea [15]. The discrepancy arose mainly from a relatively high incidence rate of TB in TNF inhibitor-naïve patients (308/100,000 PY) in the prior study as compared with 123/100,000 PY in our study. In the prior study, TB was diagnosed based on the presence of typical symptoms of TB and compatible radiologic findings in the absence of microbiologic evidence or treatment response. Further, the number of AS patients who took MTX or glucocorticoids was much higher, possibly contributing to the discrepancy in the TB rates between both studies.
In this study, extrapulmonary manifestation was the dominant form of TB disease during TNF inhibitor treatment (diagnosed in 85.7 % of TNF inhibitor-treated AS and RA patients), as compared to <20 % or less observed in the general population [2, 14, 19, 22, 28]. Extrapulmonary TB is associated with a decrease in the production of interferon-γ, TNF, interleukin (IL)-10, and IL-6 by macrophages infected with mycobacteria; therefore, inhibiting TNF likely contributes to systemic spreading of mycobacteria to cause extrapulmonary infection [8]. The symptoms of extrapulmonary TB are less “typical,” delaying diagnosis and treatment [11]; therefore, patients with symptoms of any infection during anti-TNF treatment should be screened for a TB infection.
After adjusting for age and sex, a low BMI (<22 kg/m2) was found to be an independent risk factor for TB in AS patients, consistent with a previous report showing poor nutritional status as a risk factor for TB [18]. For RA patients, age >60 years and hospitalization were both associated with TB infection, suggesting that general health status has an effect on susceptibility to TB.
The TB outcome was good in AS: only three of seven patients needed inpatient treatment compared with six of seven RA patients. Two RA patients died from progressive pulmonary TB whereas all AS patients recovered without long-term consequences. Those findings need careful interpretation considering the low TB incidences in this study. However, it is tempting to speculate that the TB severity may be influenced by underlying comorbidities and concomitant immunosuppressive use whereas TB susceptibility is predominantly affected by anti-TNF treatment.
The temporal relationship between the onset of TB and the start of TNF inhibitor treatment and frequent extrapulmonary manifestations during TNF inhibitor treatment emphasizes the critical role of TNF in the defense against TB infection. Although reactivation of latent TB may be a main cause of treatment-associated infections, a new primary extrapulmonary TB infection in TNF-depleted host is still possible especially in endemic areas [9, 12, 13].
Our study has several limitations. First, as a tertiary referral center, patients with higher disease activity might be enrolled in the present study, leading to a selection bias. Therefore, generalization of the present findings should be with caution. Second, as a retrospective study, the ascertainment of the clinical information could be incomplete. As example, the status of prior BCG vaccination could not be evaluated when diagnosing LTBI. This is important since up to two thirds of the population received the vaccination as a child in Korea, and vaccination can give a false-positive TST, leading to a higher estimate of LTBI in the study [16]. However, since all data on RA and AS patients were retrieved in the same manner, the findings comparing the AS and RA cohort should be credible. Third, as a single center experience, the cohort size was relatively small with risk of over- or underestimation of incidence of TB and its outcomes during TNF inhibitor treatment. The findings of the present study need confirmation in a larger cohort, for example in the form of a population-based study.
In conclusion, the incidence of TB was comparable in patients with AS or RA during TNF inhibitor treatment. Any sign of infection should alert physicians to diligently evaluate for a TB infection while receiving TNF inhibitors.
References
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS et al (1988) The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31:315–324
Baronnet L, Barnetche T, Kahn V, Lacoin C, Richez C, Schaeverbeke T (2011) Incidence of tuberculosis in patients with rheumatoid arthritis. A systematic literature review. Joint Bone Spine 78:279–284
Braun J, Sieper J (2002) Therapy of ankylosing spondylitis and other spondyloarthritides: established medical treatment, anti-TNF-alpha therapy and other novel approaches. Arthritis Res 4:307–321
Davis JC, Van Der Heijde D, Braun J, Dougados M, Cush J, Clegg DO et al (2003) Recombinant human tumor necrosis factor receptor (etanercept) for treating ankylosing spondylitis: a randomized, controlled trial. Arthritis Rheum 48:3230–3236
Dixon W, Hyrich K, Watson K, Lunt M, Galloway J, Ustianowski A et al (2010) Drug-specific risk of tuberculosis in patients with rheumatoid arthritis treated with anti-TNF therapy: results from the British Society for Rheumatology Biologics Register (BSRBR). Ann Rheum Dis 69:522–528
Emery P, Breedveld FC, Hall S, Durez P, Chang DJ, Robertson D et al (2008) Comparison of methotrexate monotherapy with a combination of methotrexate and etanercept in active, early, moderate to severe rheumatoid arthritis (COMET): a randomised, double-blind, parallel treatment trial. Lancet 372:375–382
Feldmann M (2002) Development of anti-TNF therapy for rheumatoid arthritis. Nat Rev Immunol 2:364–371
Fiske CT, de Almeida AS, Shintani AK, Kalams SA, Sterling TR (2012) Abnormal immune responses in persons with previous extrapulmonary tuberculosis in an in vitro model that simulates in vivo infection with Mycobacterium tuberculosis. Clin Vaccine Immunol 19:1142–1149
Galloway JB, Hyrich KL, Mercer LK, Dixon WG, Fu B, Ustianowski AP et al (2011) Anti-TNF therapy is associated with an increased risk of serious infections in patients with rheumatoid arthritis especially in the first 6 months of treatment: updated results from the British Society for Rheumatology Biologics Register with special emphasis on risks in the elderly. Rheumatology (Oxford) 50:124–131
Gómez–Reino JJ, Carmona L, Valverde VR, Mola EM, Montero MD (2003) Treatment of rheumatoid arthritis with tumor necrosis factor inhibitors may predispose to significant increase in tuberculosis risk: a multicenter active–surveillance report. Arthritis Rheum 48:2122–2127
Hou CL, Tsai YC, Chen LC, Huang JL (2008) Tuberculosis infection in patients with systemic lupus erythematosus: pulmonary and extra-pulmonary infection compared. Clin Rheumatol 27:557–563
Jacobs M, Samarina A, Grivennikov S, Botha T, Allie N, Fremond C et al (2007) Review: reactivation of tuberculosis by tumor necrosis factor neutralization. Eur Cytokine Network 18:1–9
Keane J (2004) Tumor necrosis factor blockers and reactivation of latent tuberculosis. Clin Infect Dis 39:300–302
Keane J, Gershon S, Wise RP, Mirabile-Levens E, Kasznica J, Schwieterman WD et al (2001) Tuberculosis associated with infliximab, a tumor necrosis factor α-neutralizing agent. N Engl J Med 345:1098–1104
Kim EM, Uhm WS, Bae SC, Yoo DH, Kim TH (2011) Incidence of tuberculosis among Korean patients with ankylosing spondylitis who are taking tumor necrosis factor blockers. J Rheumatol 38:2218–2223
Lee H, Dockrell HM, Kim DR, Floyd S, Oh SY, Lee JB et al (2012) The current status of BCG vaccination in young children in South Korea. Tuberc Respir Dis 72:374–380
Lee SK, Kim SY, Kim EY, Jung JY, Park MS, Kim YS et al. (2013) Mycobacterial Infections in patients treated with tumor necrosis factor antagonists in South Korea. Lung (in press)
Leung CC, Lam TH, Chan WM, Yew WW, Ho KS, Leung G et al (2007) Lower risk of tuberculosis in obesity. Arch Intern Med 167:1297
Mayordomo L, Marenco JL, Gomez-Mateos J, Rejon E (2002) Pulmonary miliary tuberculosis in a patient with anti-TNF-alpha treatment. Scand J Rheumatol 31:44–45
McInnes IB, Schett G (2011) The pathogenesis of rheumatoid arthritis. N Engl J Med 365:2205–2219
Park JS (2012) Korean guidelines for the treatment of tuberculosis. Korean J Med 82:269–273
Querini PR, Vecellio M, Sabbadini M, Ciboddo G (2002) Miliary tuberculosis after biological therapy for rheumatoid arthritis. Rheumatology 41:231
St Clair EW, van der Heijde DM, Smolen JS, Maini RN, Bathon JM, Emery P et al (2004) Combination of infliximab and methotrexate therapy for early rheumatoid arthritis: a randomized, controlled trial. Arthritis Rheum 50:3432–3443
Tam LS, Gu J, Yu D (2010) Pathogenesis of ankylosing spondylitis. Nat Rev Rheumatol 6:399–405
van der Heijde D, Dijkmans B, Geusens P, Sieper J, DeWoody K, Williamson P et al (2005) Efficacy and safety of infliximab in patients with ankylosing spondylitis: results of a randomized, placebo–controlled trial (ASSERT). Arthritis Rheum 52:582–591
van der Linden S, Valkenburg HA, Cats A (1984) Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum 27:361–368
Wallis R, Broder M, Wong J, Hanson M, Beenhouwer D (2004) Granulomatous infectious diseases associated with tumor necrosis factor antagonists. Clin Infect Dis 38:1261–1265
Weir MR, Thornton GF (1985) Extrapulmonary tuberculosis. Experience of a community hospital and review of the literature. Am J Med 79:467–478
Westhovens R, Yocum D, Han J, Berman A, Strusberg I, Geusens P et al (2006) The safety of infliximab, combined with background treatments, among patients with rheumatoid arthritis and various comorbidities: a large, randomized, placebo–controlled trial. Arthritis Rheum 54:1075–1086
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, H.W., Park, J.K., Yang, JA. et al. Comparison of tuberculosis incidence in ankylosing spondylitis and rheumatoid arthritis during tumor necrosis factor inhibitor treatment in an intermediate burden area. Clin Rheumatol 33, 1307–1312 (2014). https://doi.org/10.1007/s10067-013-2387-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-013-2387-z