Abstract
Over the last decade, biologic therapeutic proteins have advanced the treatment of diseases such as rheumatoid arthritis (RA). Therapeutic antibodies such as infliximab, adalimumab, rituximab, tocilizumab, golimumab, certolizumab pegol, the receptor construct etanercept, and abatacept, an anticluster of differentiation (CD)80/anti-CD86 fusion protein, are used as treatment for RA and ankylosing spondylitis (AS). Infliximab, adalimumab, golimumab, certolizumab pegol, and etanercept are inhibitors of tumor necrosis factor (TNF), a key regulator of inflammation. Left untreated, progression of rheumatic diseases due to inflammation can lead to irreversible joint damage and serious disability. One limitation for the use of therapeutic antibodies is immunogenicity, the induction of antibodies by the adaptive immune system in response to foreign substances. The development of antidrug antibodies (ADAs) has a varying impact on the clinical efficacy of biologic agents for the treatment of RA and AS, depending on whether the ADAs are neutralizing or non-neutralizing. Studies have indicated that neutralizing ADAs are associated with a reduced efficacy, decreased drug survival, increased instances of dose escalation, and adverse events. Comparison studies of anti-TNF biologics have demonstrated that each drug has a different sustained efficacy profile depending on immunogenicity. The purpose of this review is to provide rheumatologists with information regarding the effect of neutralizing antibodies on the sustainable efficacy of anti-TNF biologic therapies. This information will be of value to practicing rheumatologists in Africa and the Middle East who should take into account the potential for changes in the efficacy and safety of biologic therapies and closely monitor patients under their care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the last decade, biologic therapeutic proteins have advanced the treatment of diseases such as rheumatoid arthritis (RA) [1]. Biologics are drugs that are either comprised of native proteins such as hormones, cytokines, and growth factors or engineered molecules such as therapeutic monoclonal antibodies, antibody fragments, or protein constructs [1]. The fastest growing class of human biologics is monoclonal antibodies, with many approved for the treatment of rheumatic diseases [1]. Therapeutic antibodies such as infliximab, adalimumab, rituximab, tocilizumab, golimumab, certolizumab pegol, the receptor construct etanercept, and abatacept, an anticluster of differentiation (CD)80/anti-CD86 fusion protein, are widely used as treatment for RA and ankylosing spondylitis (AS) [1–9]. Infliximab, adalimumab, golimumab, certolizumab pegol, and etanercept are inhibitors of tumor necrosis factor (TNF), a key regulator of inflammation [10]. Left untreated, progression of RA due to aberrant inflammation can lead to irreversible joint damage and serious disability [11]. In Africa and the Middle East, the limited numbers of rheumatologists have an additional responsibility of raising awareness of the treatable nature of RA and AS while utilizing current long-term safety and efficacy data to make treatment decisions for patients under their care [12, 13]. The purpose of this review is to provide rheumatologists in Africa and the Middle East, as well as others in similar practices with critical information regarding the effect of neutralizing antibodies on the sustainable efficacy of anti-TNF biologic therapies.
Immunogenicity
One of the main limitations for the use of therapeutic antibodies is immunogenicity [14]. Immunogenicity refers to the induction of antibodies by the adaptive immune system in response to foreign substances. Immunogenicity of biologic drugs is unpredictable and unforeseeable, and small changes in a macromolecule can completely shift its immunogenic profile [1]. Many biologic therapies cause an immune response leading to the development of antidrug antibodies (ADA); this can reduce efficacy and sometimes lead to life-threatening complications [1, 14]. The propensity of a biologic therapy to induce immunogenicity depends primarily on its structural properties [15]. The immune response against a native biologic (human hormones, growth factors, and cytokines) differs from the immune response against designed biologics containing new foreign epitopes or murine-derived molecules [1, 15]. This immune response occurs only when the natural tolerance against these biologics is broken; however, this type of reaction occurs infrequently [1].
Immunogenic mechanisms and the evolution of biologics
Immunogenicity against designed therapeutic biologics is a normal immune response against a foreign antigen [1]. The first therapeutic antibodies were of mouse origin and close to 90 % of patients treated with these drugs developed human antimouse antibodies. These extreme reactions limited clinical use of therapeutic antibodies derived from murine sources [16]. Immunogenicity of therapeutic antibodies has been reduced by replacing murine constant regions with human ones, resulting in chimeric antibodies such as infliximab and rituximab [1]. However, these antibodies have been shown to induce the formation of human antichimeric antibodies, which can also reduce efficacy and cause allergic reactions [15]. Humanization of the variable regions of the therapeutic antibodies further reduces immunogenicity; however, fully human antibodies may also lead to the production of human antihuman antibodies [15, 16].
Immunogenicity of fusion proteins like etanercept and abatacept depends on their similarity to native proteins [1]. The fusion portion of these biologics may contain new epitopes that can be recognized as foreign by the immune system. Antibody formation had been described in patients treated with etanercept; however, the antibodies do not affect the TNF binding domain [5]. Differences in immunogenicity between the most common anti-TNF biologics are discussed in a later section. For practicing physicians, it is important to consider that immunogenicity is a gradual process, developing and changing over time, and continuation of treatment may either induce tolerance or stimulate further antibody production in patients treated with anti-TNF biologics. Frequent, careful monitoring of patients treated with anti-TNF biologics is critical in preventing reduced long-term efficacy or adverse reactions.
Pharmacologic implications of immunogenic mechanisms
Continued immune responses can have varying consequences, depending on their severity and if the response is caused by neutralizing or non-neutralizing antibodies [1]. There is no structural difference between neutralizing antibodies and non-neutralizing antibodies; however, the key difference is in the effect they have on the efficacy of a biologic. Neutralizing antibodies may neutralize or inactivate the biologic molecule, rendering it therapeutically ineffective. These antibodies cause altered pharmacokinetics and, over a long duration, may be responsible for the loss of efficacy observed in patients treated with biologics [17]. For example, antibodies to infliximab, adalimumab, and other monoclonal antibodies can lower biologic serum levels and therefore “neutralize” the efficacy of these agents [15, 18–20]. Non-neutralizing antibodies do not affect the action of the drug and may not affect clinical outcomes. However, rare but serious autoimmune responses such as anaphylaxis, infusion reaction, cross-reactivity to endogenous proteins, or other adverse events (AEs) can be life-threatening [17]. Importantly, immunogenicity can only be revealed through clinical trials, as the assessment of ADAs is quite complex [1].
Differences in immunogenicity between the different anti-TNF biologics
All monoclonal antibodies that are used in the treatment of RA are associated with antibody formation, and neutralizing antibodies have been associated with most of them [2–6]. As previously discussed, the ability of a biologic therapy to induce ADAs depends primarily on its structural properties and the body’s response to these structures as foreign [15, 21]. Etanercept differs from other anti-TNF biologics in that it is a fully human, recombinant dimeric fusion protein consisting of the extracellular ligand-binding portion of the human TNF receptor linked to the Fc portion of human immunoglobulin G1 [5]. The non-neutralizing antibodies that are developed in response to etanercept bind to the fusion region of the protein, leaving the TNF binding site unobstructed [22].
In contrast, adalimumab, golimumab, and infliximab are all monoclonal antibodies, with adalimumab and golimumab being fully human monoclonal antibodies [2, 8] and infliximab being a humanized mouse monoclonal antibody [2]. Antibodies developed in response to these monoclonal antibodies are elicited to the hypervariable complementary-determining regions on the Fab portions of the antibodies [22]. These neutralizing antibody immune responses obstruct the TNF binding site, which reduces the ability of the monoclonal antibodies to effectively bind TNF [22]. The unbound TNF is released, free to bind to its cellular receptors, thus inducing the inflammatory cascade. In addition to factors associated with the treatment, immunogenicity also seems to be the result of factors associated with the patient. Additionally, immunosuppressors, such as methotrexate, limit the formation of these antibodies [21]. These differences in antibody formation between the anti-TNF biologics have important implications for sustained efficacy in the treatment of rheumatic diseases.
Effect of ADAs on drug concentrations in RA patients
Previous short-term studies have indicated that the immunogenicity of monoclonal antibodies led to associations between ADA development and decreased serum drug levels, and ultimately a decreased treatment response [20]. Up until this point, however, little was known about the long-term impact of ADAs on drug concentrations. In a long-term follow-up study of 272 (55 % completed follow-up) RA patients treated with adalimumab, Bartelds et al. [20] assessed serum adalimumab concentrations and anti-adalimumab antibody titers after follow-up at 156 weeks. Clinical outcomes were compared between patients with and without anti-adalimumab antibodies. As shown in Fig. 1, anti-adalimumab antibodies were found in 76 patients (28 %), and 51 of 76 (67 %) of anti-adalimumab antibody-positive patients developed anti-adalimumab antibodies during the first 28 weeks of treatment [20]. Patients with anti-adalimumab antibodies discontinued participation more often due to treatment failure [n = 29 (38 %); hazard ratio (HR) = 3.0; 95 % confidence interval, 1.6–5.5; P < 0.001] compared with anti-adalimumab antibody-negative patients [n = 28 (14 %)]. Patients with anti-adalimumab antibodies also experienced a reduced treatment efficacy, with only 10 of 76 (13 %) in a state of minimal disease activity, compared to 95 of 196 patients (48 %) without anti-adalimumab antibodies [20]. Furthermore, only 3 of 76 patients (4 %) with anti-adalimumab antibodies achieved sustained remission (disease activity score in 28 joints ≤ 2.6) compared with 67 of 196 anti-adalimumab antibody-negative patients (34 %). These data provide evidence that the development of ADAs in response to biologic therapy is associated with reduced drug serum levels and a diminished likelihood of achieving minimal disease activity or clinical remission.
Percentage of patients with anti-adalimumab antibodies over time. Note that 51 of 76 (67 %) of anti-adalimumab antibody-positive patients developed anti-adalimumab antibodies during the first 28 weeks of treatment [20]. Number of patients with available serum samples are shown. Adapted with permission from Bartelds et al. [20]
Clinical impact of ADA development on RA and AS treatment
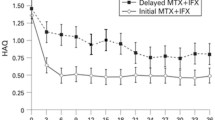
Several studies have demonstrated that ADA development has important clinical consequences in patients with RA and AS. Wolbrink et al. [23] evaluated the clinical impact of anti-infliximab antibodies in 51 patients with RA using European League Against Rheumatism (EULAR) established response criteria. The results of the study demonstrated that the production of anti-infliximab antibodies was associated with a reduction in the clinical response (Fig. 2). However, patients without anti-infliximab antibodies responded to therapy [23]. The development of ADAs also has a negative impact on clinical response in AS patients. In a study conducted by de Vries et al. [25], patients with AS were treated with infliximab and clinical responses were measured according to the AS Assessment of SpondyloArthritis International Society scale of 20 % (ASAS20) response at 54 weeks. The authors found that approximately 75 % of patients without anti-infliximab antibodies achieved an ASAS20 response; in contrast, there was a significant reduction in patients that achieved an ASAS20 response in patients with anti-infliximab antibodies [25]. Overall, the presence of anti-infliximab antibodies with AS patients was associated with undetectable serum infliximab levels, reduced treatment response, and an increased risk of infusion reaction [25].
The production of anti-adalimumab antibodies and resulting alterations in clinical responses are observed with adalimumab treatment in patients with RA and AS [26, 27]. Bartelds et al. found that in RA patients treated with adalimumab, the presence of anti-adalimumab antibodies had an inverse relationship with improvements in EULAR response [26]. As shown in Fig. 2, the proportion of RA patients with a good response increased as the anti-adalimumab antibody concentration decreased, and there were no good responders among patients who developed high concentrations of anti-adalimumab antibodies [26]. In a recent study conducted by Arends et al. [27], approximately 30 % of AS patients treated with adalimumab developed anti-adalimumab antibodies. These patients also had significantly lower serum levels of adalimumab compared to AS patients without anti-adalimumab antibodies and had significantly diminished clinical treatment responses [27]. Importantly, administration of infliximab or adalimumab in combination with methotrexate has been shown to reduce the production of ADA [27, 28].
Treatment with etanercept has been shown to induce antibody production in patients with RA but not AS [29, 30]. Importantly, clinical responses in RA patients are not altered [29], and serum levels of etanercept are not affected by simultaneous use of methotrexate [5]. The impactive difference affecting anti-etanercept antibodies on clinical response is likely due to etanercept being a fully human fusion protein, the ability of maintaining stable drug serum levels, and the non-neutralizing nature of the anti-etanercept antibodies [30]. These findings suggest that etanercept efficacy should be sustained without dose escalation.
It is common in clinical practice to switch from one TNF inhibitor to another in case of inadequate response or AEs [31]. Generally, treatment responses after switching are better in patients who stopped their first-course TNF inhibitor due to AEs rather than inefficacy [32–34]. A recent study by Jamnitski et al. [35] demonstrated that patients who previously discontinued infliximab or adalimumab treatment and who had antibodies against these drugs achieved a clinical response after switching to etanercept that did not differ from patients who were anti-TNF naive. In contrast, switchers without antibodies against adalimumab or infliximab had a significantly lower response to etanercept compared to switchers with antibodies and patients who were TNF naive. These results suggest that there are different types of nonresponders with different underlying mechanisms causing nonresponse and determining immunogenicity can be helpful in deciding if patient switching could be a beneficial treatment regimen.
Impact of ADAs on biologic discontinuation rates in RA
The development of ADAs has been shown to have an impact on discontinuation rates of anti-TNF biologic therapy in RA. Strangfeld et al. [36] compared drug discontinuation rates in combination therapy with a TNF inhibitor (infliximab, adalimumab, or etanercept) plus methotrexate or leflunomide in 1769 patients from the German RA Observation of Biologic Therapy (RABBIT) registry. Figure 3 reveals that discontinuation rates at all time points for biologics in combination with the disease-modifying antirheumatic drugs (DMARDs) methotrexate and leflunomide in RABBIT were highest for infliximab, intermediate for adalimumab, and lowest for etanercept [36]. In a separate study, Marchesoni et al. [37] used data from the Lombardy Rheumatology Network registry to evaluate drug survival in 1,064 patients treated with infliximab, adalimumab, or etanercept. Data showed that long-term survival of etanercept was better than that of both infliximab and adalimumab. The authors concluded that the risk of discontinuing infliximab was mainly due to primary or secondary loss of efficacy, whereas the risk of discontinuing adalimumab was mainly due to AEs [37]. Hetland and colleagues [38] conducted another direct comparison of drug adherence with infliximab, adalimumab, and etanercept using data from 2,326 patients from the Danish Registry for Biological Treatment in Rheumatology registry. Patients with RA who failed one or more DMARDs and initiated adalimumab (675 patients), etanercept (517 patients), or infliximab (1,134 patients) as the first biologic agent were included in the analysis [38]. The investigators found that adherence was highest in patients treated with etanercept (56 %) and lowest in patients treated with infliximab (41 %) [38]. These differences in discontinuation rates among the anti-TNF biologics are important for rheumatologists to consider when choosing an appropriate treatment strategy for patients under their care.
Discontinuation rates in patients treated with etanercept, infliximab, or adalimumab in combination with either methotrexate or leflunomide: data from the RABBIT registry. Note that etanercept therapy resulted in the lowest discontinuation rates across all time points [36]
Impact of ADAs on dose escalation in RA treatment
In instances of reduced serum levels of biologic monoclonal antibodies due to ADAs, some patients may benefit from increased dosages [2, 3]. There are several reports of dose escalation in patients treated with anti-TNF biologics [39], and the prescribing information of adalimumab and infliximab suggest that dose escalation may be considered in patients experiencing a reduction in clinical response [2, 3]. In a recent report, Moots et al. [39] evaluated the prevalence of dose escalation in a retrospective observational study of 739 patients with RA receiving continuous treatment with etanercept, adalimumab, or infliximab for 18 months. As shown in Fig. 4, dose escalation occurred during therapy with adalimumab (3–5 times higher) or infliximab (10 times higher) compared with patients treated with etanercept [39]. The investigators also evaluated secondary escalation, which was defined as intensifying the dose of the biologic or DMARD component of the therapy. The prevalence of secondary escalation was significantly higher during therapy with adalimumab or infliximab compared to therapy with etanercept [39]. Since antietanercept antibodies do not alter clinical responses, dose escalation is not recommended, when compared with monoclonal antibody drugs [2, 3, 5]. These factors are also important for rheumatologists to consider, as increased drug concentrations can lead to increased costs and a greater risk of AEs.
Conclusions
Immunogenicity is the primary factor limiting the use of anti-TNF biologics. The development of ADAs has a varying impact on the clinical efficacy of biologic agents for the treatment of RA and AS, depending on whether the ADAs are neutralizing or non-neutralizing. Several studies have indicated that neutralizing ADAs are associated with a reduced likelihood of achieving a minimal disease activity state or clinical remission, decreased drug survival, increased instances of dose escalation, and AEs. Comparison studies of anti-TNF biologics have demonstrated that each drug has a different sustained efficacy profile depending on immunogenicity. The impact on long-term efficacy and safety should be considered by practicing physicians when making therapeutic decisions for patients with RA or AS.
References
Wolbink GJ, Aarden LA, Dijkmans BA (2009) Dealing with immunogenicity of biologicals: assessment and clinical relevance. Curr Opin Rheumatol 21:211–215
EU summary of product characteristics: Remicade (2012) Centocor BV, Leiden
EU summary of product characteristics: Humira (2012) Abbott Biotechnology Deutschland GmBH, Wiesbaden
Prescribing information: Rituximab (2012). Biogen Idec Inc and Genentech, South San Francisco
EU summary of product characteristics: Enbrel (2012) Pfizer, Hampshire
EU summary of product characteristics: Cimzia (2011) UCB Pharma, Bruselles
EU summary of product characteristics: MabThera (2012) Roche Pharma AG, Grenzach-Wyhlen
EU summary of prescribing characteristics: Simponi (2012) Centocor BV, Leiden
EU summary of product characteristics: RoActemra (2011) Roche Registration, Welwyn Garden City
Choy EH, Panayi GS (2001) Cytokine pathways and joint inflammation in rheumatoid arthritis. N Engl J Med 344:907–916
Kvien TK (2004) Epidemiology and burden of illness of rheumatoid arthritis. Pharmacoeconomics 22(2 Suppl 1):1–12
Badsha H, Kong KO, Tak PP (2008) Rheumatoid arthritis in the United Arab Emirates. Clin Rheumatol 27:739–742
Mody GM, Cardiel MH (2008) Challenges in management of rheumatoid arthritis in developing countries. Best Pract Res Clin Rheumatol 22:621–641
Schellekens H (2002) Immunogenicity of therapeutic proteins: clinical implications and future prospects. Clin Ther 24:1720–1740
Emi Aikawa N, de Carvalho JF, Artur Almeida Silva C, Bonfa E (2010) Immunogenicity of anti-TNF-alpha agents in autoimmune diseases. Clin Rev Allergy Immunol 38:82–89
Hwang WY, Foote J (2005) Immunogenicity of engineered antibodies. Methods 36:3–10
Jahn EM, Schneider CK (2009) How to systematically evaluate immunogenicity of therapeutic protiens-regulatory considerations. N Biotechnol 25:280–286
Anderson PJ (2005) Tumor necrosis factor inhibitors: clinical implications of their different immunogenicity profiles. Semin Arthritis Rheum 34(5 Suppl 1):19–22
Radstake TR, Svenson M, Eijsbouts AM, van den Hoogen FH, Enevold C, van Riel PL, Bendtzen K (2009) Formation of antibodies against infliximab and adalimumab strongly correlates with functional drug levels and clinical responses in rheumatoid arthritis. Ann Rheum Dis 68:1739–1745
Bartelds GM, Krieckaert CL, Nurmohamed MT, van Schouwenburg PA, Lems WF, Twisk JW, Dijkmans BA, Aarden L, Wolbink GJ (2011) Development of antidrug antibodies against adalimumab and association with disease activity and treatment failure during long-term follow-up. JAMA 305:1460–1468
Emi Aikawa N, de Carvalho JF, Artur Almeida Silva C, Bonfá E (2010) Immunogenicity of anti-TNF-alpha agents in autoimmune diseases. Clin Rev Allergy Immunol 38:82–89
Fleischmann R, Shealy D (2003) Developing a new generation of TNF alpha antagonists for the treatment of rheumatoid arthritis. Mol Interv 6:310–318
Wolbink GJ, Vis M, Lems W, Voskuyl AE, de Groot E, Nurmohamed MT, Stapel S, Tak PP, Aarden L, Dijkmans B (2006) Development of antiinfliximab antibodies and relationship to clinical response in patients with rheumatoid arthritis. Arthritis Rheum 54:711–715
Bartelds GM, Wijbrandts CA, Nurmohamed MT, Stapel S, Lems WF, Aarden L, Dijkmans BA, Tak PP, Wolbink GJ (2007) Clinical response to adalimumab: relationship to anti-adalimumab antibodies and serum adalimumab concentrations in rheumatoid arthritis. Ann Rheum Dis 66:921–926
de Vries MK, Wolbink GJ, Stapel SQ, de Vrieze H, van Denderen JC, Dijkmans BA, Aarden LA, van der Horst-Bruinsma IE (2007) Decreased clinical response to infliximab in ankylosing spondylitis is correlated with anti-infliximab formation. Ann Rheum Dis 66:1252–1254
Bartelds GM, Wijbrandts CA, Nurmohamed MT, Stapel S, Lems WF, Aarden L, Dijkmans BA, Tak PP, Wolbink GJ (2007) Clinical response to adalimumab: relationship to anti-adalimumab antibodies and serum adalimumab concentrations in rheumatoid arthritis. Ann Rheum Dis 66:921–926
Arends S, Lebbink HR, Spoorenberg et al (2010) The formation of autoantibodies and antibodies to TNF-α blocking agents in relation to clinical response in patients with ankylosing spondylitis. Clin Exp Rheumatol 28:661–668
Maini RN, Breedveld RC, Kalden JR et al (1998) Therapeutic efficacy of multiple intravenous infusions of anti-tumor necrosis factor alpha monoclonal antibody combined with low-dose weekly methotrexate in rheumatoid arthritis. Arthritis Rheum 41:1552–1563
Keystone EC, Schiff MH, Kremer JM, Kafka S, Lovy M, DeVries T, Burge DJ (2004) Once-weekly administration of 50 mg etanercept in patients with active rheumatoid arthritis: results of a multicenter, randomized, double-blind, placebo-controlled trial. Arthritis Rheum 50:353–363
de Vries MK, van der Horst-Bruinsma IE et al (2009) Immunogenicity does not influence treatment with etanercept in patients with ankylosing spondylitis. Ann Rheum Dis 68:531–535
Rubbert-Roth A, Finckh A (2009) Treatment options in patients with rheumatoid arthritis failing initial TNF inhibitor therapy: a critical review. Arthritis Res Ther 11(Supp 11): S1
Gomez-Reino JJ, Carmona L, BIOBADASER Group (2006) Switching TNF antagonists in patients with chronic arthritis: an observational study of 488 patients over a four-year period. Arthritis Res Ther 8:R29
Hyrich KL, Lunt M, Watson KD, Symmons DP, Silman AJ, British Society for Rheumatology Biologics Register (2007) Outcomes after switching from one anti-tumor necrosis factor alpha agent to a second anti-tumor necrosis factor alpha agent in patients with rheumatoid arthritis: results from a large UK national cohort study. Arthritis Rheum 56:13–20
Iannone F, Trotta F, Montecucco C et al (2007) Etanercept maintains the clinical benefit achieved by infliximab in patients with rheumatoid arthritis who discontinued infliximab because of side effects. Ann Rheum Dis 66:249–252
Jamnitski A, Bartelds GM, Nurmohamed MT et al (2011) The presence or absence of antibodies to infliximab or adalimumab determines the outcome of switching to etanercept. Ann Rheum Dis 70:284–288
Strangfeld A, Hierse F, Kekow J, von Hinueber U, Tony HP, Dockhorn R, Listing J, Zink A (2009) Comparative effectiveness of tumour necrosis factor alpha inhibitors in combination with either methotrexate or leflunomide. Ann Rheum Dis 68:1856–1862
Marchesoni A, Zaccara E, Goria R, Bazzani C, Sarzi-Puttini P, Atzeni F, Caporali R, Bobbio-Pallavicini F, Favalli EG (2009) TNF-alpha antagonist survival rate in a cohort of rheumatoid arthritis patients observed under conditions of standard clinical practice. Ann NY Acad Sci 1173:837–846
Hetland ML, Christensen IJ, Tarp U et al (2010) Direct comparison of treatment responses, remission rates, and drug adherence in patients with rheumatoid arthritis treated with adalimumab, etanercept, or infliximab: results from eight years of surveillance of clinical practice in the nationwide Danish DANBIO registry. Arthritis Rheum 62:22–32
Moots RJ, Haraoui B, Matacci-Cerinic M et al (2011) Differences in biologic dose-escalation, non-biologic and steroid intensification among three anti-TNF agents: evidence from clinical practice. Clin Exp Rheumatol 29:26–34
Acknowledgments
Editorial/medical writing support was provided by WC Hatch at ACUMED and was funded by Pfizer Inc. No financial support was provided to the authors for this work.
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alawadhi, A., Alawneh, K. & Alzahrani, Z.A. The effect of neutralizing antibodies on the sustainable efficacy of biologic therapies: what’s in it for African and Middle Eastern rheumatologists. Clin Rheumatol 31, 1281–1287 (2012). https://doi.org/10.1007/s10067-012-2040-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-012-2040-2