Abstract
To investigate that a 6-month treatment with avocado soybean unsaponifiable (Piascledine® 300 mg) once daily is as effective as with chondroitin sulfate 400 mg three times daily in femorotibial gonarthrosis, and also the carry-over effect for two more months is comparable. Patients were randomized (1:1) to the treatment groups. They received for 6 months 3 capsules chondroitin sulfate per day or one capsule of avocado soybean unsaponifiable (ASU) in a double-dummy technique. A 2-month post-treatment period followed to determine the carry-over effect. Primary efficacy criterion was the change of the WOMAC-index from study begin to end of treatment. Secondary criteria were the changes in Lequesne-index, pain on active movement and at rest, global assessment of efficacy. Three hundred sixty-four patients have been taken up into the trial. Three hundred sixty one patients were eligible for evaluation. One hundred eighty three received ASU 300 mg once daily, one hundred seventy eight chondroitin sulfate three times daily. The WOMAC-index decreased in both groups for approx. 50% to the end of therapy. During the post-treatment observation there was a further slight improvement. There was no statistical significant difference between the treatment groups during the entire observation. All other observed parameters showed the same pattern. The daily intake of rescue medication was reduced continuously. Overall efficacy has been rated excellent and good in more than 80% of the patients in both groups. Both drugs were safe and well tolerated. The first direct comparison between avocado soybean unsaponifiable 300 mg once daily and chondroitin sulfate three times daily reveiled no difference in efficacy or safety aspects between 1 capsule ASU 300 mg per day and 3 capsules chondroitin sulfate per day. It can be assumed that the once daily intake of ASU will lead to a better compliance in routine therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) is a degenerative joint disease. It can result from the effects of cumulative wear at the joint surfaces, trauma, or from genetic factors [1].
Osteoarthritis causes cartilage degeneration, characterized by damage of the cartilage collagen network and the loss of proteoglycans [2]. Twenty-five percent of women and 15% of men over the age of 60 years show some signs of this degenerative disease [3].
The current classification of the medication for osteoarthritis recognizes three types of drugs [4–9]: fast-acting drugs inducing symptomatic relief (acetaminophen, non-steroidal anti-inflammatory drugs); the symptomatics slow-acting drugs for OA (SYSADOA), which later have a carry-over effect [10, 11], the two tested product in this trial, Piascledine® and Chondroïtin® sulfate, belong to this category and lastly, the structure-modifying drugs, which are expected to have a beneficial effect on the progression of the structural changes in osteoarthritis. This group is currently under investigation; some of these substances have shown promising results, but there is no evidence that they can stop or minimize the structural changes due to OA.
Piascledine® 300 consists of avocado soybean unsaponifiable (ASU) in proportions of \({\raise0.7ex\hbox{$1$} \!\mathord{\left/ {\vphantom {1 3}}\right.\kern-\nulldelimiterspace}\!\lower0.7ex\hbox{$3$}}\) and \({\raise0.7ex\hbox{$2$} \!\mathord{\left/ {\vphantom {2 3}}\right.\kern-\nulldelimiterspace}\!\lower0.7ex\hbox{$3$}}\), respectively. It has shown interesting properties in in vitro and in vivo animal models of experimental arthrosis. These results provided evidence on the pharmacological properties for a basic treatment of arthrosis [11–18].
The non-saponifiable residues inhibit interleukin-1 (IL-1) and stimulate the synthesis of collagen in joint chrondrocyte cultures [11].
The anti-collagenolytic activity of non-saponifiable substances and their capacity of partially inhibiting the deleterious effects of IL-1 have been demonstrated in two studies: using bovine joint chrondrocyte cultures [14] and human joint chrondrocyte cultures [15], respectively.
Chondroitin sulfate consists of repeating chains of glycosaminoglycans. It is a major component of cartilage, providing structure, holding water and nutrients and allowing other molecules to move through the cartilage providing resistance and elasticity of the cartilage. It has been shown, in numerous double-blind clinical trials [19–21], to relieve pain and increase joint function and, possibly, be able to slow down progression of the disease. There is no evidence that chondroitin sulfate will cure osteoarthritis.
The objective of the present study was to compare the efficacy of ASU 300 mg once daily as a symptomatic therapy to chondroitin sulfate three times daily during a 6-month treatment (plus 2 months post-treatment observation) in patients with osteoarthritis of the knee.
Patients and methods
Patients
Patients eligible to the study had to be aged 45 years or above and had femoro-tibial osteoarthritis of the knees longer than 6 months with pain and functional discomfort over 1 month during the last 3 months, were complying with the clinical and radiological criteria of the American College of Rheumatology [22] of knee osteoarthritis, had a Lequesne index between 5 and 13 and a radiologic score of stage I, II or III of the modified Kellgren/Lawrence scale [23] on a frontal image of extended knee, on both knees, the image being not older than 6 months, had pain on movement and/or pain at rest in the last 48 h at least 40 mm evaluated on a VAS, and/or at least 40 mm evaluated on at least two items among the five items in the A-section of the WOMAC index, with no intake of analgesics for 48 h and NSAID for 5 days.
Exclusion criteria were osteoarthritis of the hip located at the side of the evaluated knee, osteoarthritis of the knee that may require surgical intervention during the planned duration of the study, septic arthritis, inflammatory joint disease, known chondrocalcinosis of the joints, articular fracture of the knee, ochronosis or haemochromatosis, M Paget, chondromatosis, villo-nodular synovitis, haemophilia, gout and pseudo-gout, acromegalia, Wilson's disease, collagen gene mutations, a body mass index of >35, treatments with NSAID within 5 days or an analgesic within 48 h before inclusion, with corticoids within 1 month prior to inclusion, with SYSADOA, intra-articular injection of corticoids, hyaluronic acid into the knee, pulsed electromagnetic field, and synoviorthesis within 3 months prior to inclusion, operations (osteotomy, meniscectomy) on the evaluated knee, diseases requiring the intermittent taking of corticoids (e.g. asthma), serious evolutive heart condition, pulmonary, renal, hepatic, haematological, neoplastic or infectious diseases, allergy to one of the components of the used drugs, leucopenia from a serious hereditary disease, pregnancy or no efficient contraception at the time of inclusion, intricacy following an accident or net psychalgic component and lipid metabolism disorders.
Study design
This was a prospective, controlled, randomized, multinational, multicentre (Table 1), double-blind, double-dummy parallel-group study carried out at five centres in Czech Republic, three in Slovak Republic, five in Hungary, seven in Poland, and six in Romania.
The ethical standards adopted by the XVIII World Medical Assembly (Helsinki, 1964) and subsequent revisions have been strictly observed, as well as the European Union Good Clinical Practice standards for clinical trials. Prior to the study initiation the documentation has been submitted to the local ethics committees and the respective national authorities for review and approval. The study was monitored in regular intervals by a Contract Research Organisation to ensure compliance with the protocol and Good Clinical Practice.
Patients were treated for 180 days followed by a post-treatment observation phase of 60 days. Six visits have been performed during this time (Table 2).
The patients were instructed to keep a diary during the duration of the study, into which the intake of rescue medication had to be recorded.
The dosage of ASU was one capsule per day, the dosage of chondroitin sulfate was three capsules per day. As ASU capsules and chondroitin capsules have a different aspect, a double-dummy technique has been used to blind the medication. Thus, ASU verum and placebo were identical, and chondroitin sulfate verum and placebo were identical. The placebos contained all ingredients of the verum except the active substances. The test medication was packed into blisters according to the following scheme: Blister A contained: one capsule ASU 300 mg and three capsules chondroitin sulfate placebo. Blister B contained: one capsule ASU placebo and three capsules chondroitin sulfate 400 mg. All blisters had an identical batch number and expiry date. Each patient took four capsules per day, two in the morning, one at noon, one in the evening.
Evaluation of efficacy
The main criterion was the WOMAC index [24]. The Western Ontario and Mac Master Universities Osteoartritis Index is an arthrosis-specific self-questionnaire. It evaluates the symptoms related to pain, stiffness and functional discomfort of the last 48 hours. The questionnaire contains 24 questions (five on pain, two on stiffness and 17 on the physical function). Answers to the questions are given on visual analogue scales from 0–100 mm. The total count may vary between 0 and 2,400.
Secondary criteria were Lequesne index [25], pain on active movement and at rest [26], overall evaluation of osteoarthritis, overall assessment of efficacy and consumption of analgesics.
The algo-functional Lequesne index is used in studies evaluating treatment efficacy in arthrosis. The score of the Lequesne index may vary between 0 (indolence and handicap absent) to 24 (pain and maximal handicap). The index reflects the effect felt during the last 48 h.
Changes of pain on active movement and pain at rest assessed on a 100 mm Visual Analogue Scale (VAS) [26]. The VAS consists of a 100-mm long, horizontal line which has short vertical lines (boundaries) at both ends. The left boundary is designated as “no pain”, and the right boundary as “unbearable pain” or “extreme pain”.
The overall evaluation of osteoarthritis of the knee by investigator allows the evaluation of the state of the patient while taking into account all aspects of the patient's life influenced by osteoarthritis of the knee. It was also evaluated by a non-graduated 100 mm VAS. The left boundary was designated as “excellent health status”, and the right boundary as “very bad health status”.
Overall assessment of efficacy was assessed by both investigator and patient on a 4-point rating scale using the descriptors excellent, good, moderate, poor.
Consumption of paracetamol was evaluated during each visit by the investigator by counting the number of tablets left as compared to the number handed over during days 1 to 180 and using the self-evaluation diary from days 1 to 240.
Compliance
The patients were instructed to return the empty or partially empty blisters to the study centre at visit 2, 3, 4 and 5. The investigators counted the returned capsules. After collection of the retrieved study medication there was an additional count of the returned capsules and the appropriate/inappropriate consumption was documented. The patient was regarded as non-compliant, if he/she took less than 80% of the stipulated trial medication and/or if he/she did not take the trial products for 14 consecutive days.
Evaluation of safety
Laboratory parameters were determined haematology (WBC incl diff. blood counts, RBC incl. MCV, MCH, MCHC, thrombocytes, haematocrit, haemoglobin, ESR), electrolytes (sodium, potassium and calcium), enzymes (GOT, GPT, γ-GT and AP), serum albumin and substrates (cholesterol, glucose, creatinine, bilirubine, and total protein).
A general physical examination (skin, eyes/ears/nose/throat, head/neck, thorax, lungs, heart, abdomen, liver, spleen, pelvis, extremities/joints, neurological and other findings) has been done before therapy begin and after therapy end.
Vital signs (blood pressure, heart rate and breath rate) were determined before therapy begin and at therapy end.
Adverse events including relevant changes of the laboratory parameters were recorded and fully documented concerning onset, duration, intensity, severity, frequency, causal relationship to the study medication, treatment required, outcome and action taken with the investigation drug to all adverse events.
Overall assessment of tolerability was done by both investigator and patient on a 4-point rating scale using the descriptors excellent, good, moderate, poor.
Statistics
The sample size evaluation was based on the assumption based on results from a previous, double-blind, placebo-controlled, 6 months study with ASU versus placebo. A non-inferiority design has been chosen as an approach to investigate efficacy of the treatments. The power was set to 80%, the “true” population means for the two treatments were supposed to be equal, and group sizes should be equal. Under these conditions the number of patients/group was calculated with 157, thus an overall number of 314 evaluable patients was to be taken up into the trial. Expecting a drop-out rate of 10%, the patient number to be included was set to 360.
The randomisation to the two treatment groups was performed using the computer program Rancode 1.0 (idv München, Gauting).
Statistical analyses have been performed according to the ICH E9 guidelines “Statistical Principles for Clinical Trials.”
There were three populations evaluated. The safety analysis population was defined as all patients having had at least one administration of the allocated product. The intention to treat (ITT) population was defined as all randomised patients having the baseline efficacy measurement and at least one more measurement of the WOMAC index. The TPP (treated per protocol) population consists of all patients having completed the study without major protocol violations.
Descriptive statistics have been done for demographic data (n, mean, standard deviation, median, minimum and maximum values for continuous data, counts and frequencies for categorical and ordinal values). Homogeneity across treatment groups was assessed descriptively.
The primary efficacy parameter has been assessed for both the ITT- and the TPP- population. The decision on efficacy was done from the results of the ITT-group.
For the primary efficacy variable, the mean decrease of the WOMAC index from baseline to the end of the therapy, the parametric one-sided 95% confidence interval of the difference between the treatment group means were computed. This confidence interval had to be included in the range [−30%, ∝) of the reference mean.
For the changes from baseline of the WOMAC index at each visit, for pain on active movement assessed on the VAS scale, for pain at rest assessed on the VAS scale and the for the Lequesne index a repeated measures analysis of variance (ANOVA) was to be performed, accounting for the fixed effects of treatment, centre and treatment-centre interaction. If the treatment–centre interaction is significant then the treatment effect were to be assessed for each centre separately.
The centre effect has been determined according to the WOMAC index (as patient-related variable) and the Lequesne index (as investigator-related variable) at visit 1. For the overall evaluation of the treatment made by the patient and by the investigator and for the overall evaluation of treatment tolerability, the one-sided nonparametric 95% confidence interval of the difference between the treatment group means was to be computed.
The number of paracetamol tablets used at each visit was to be compared by the Mann–Whitney U test.
Safety analysis was to be done on the safety population, for all patients included in the study. The number of adverse events and the number of clinically significant abnormalities were compared by Fisher's exact test. The mean percent changes from baseline and their 95% confidence intervals were to be computed for each laboratory parameter.
For all efficacy and acceptability data, descriptive statistics (n, mean, standard deviation, median, upper and lower quartile and extreme values for continuous data, counts and frequencies for categorical and ordinal values) were given per visit and per treatment group (test, comparator). The descriptive statistics is based on the TPP and the ITT population.
Results
Demography and baseline characteristics
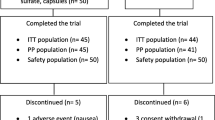
A total of 364 patients has been taken up into the trial. Each centre treated in median 12 patients (minimum three, maximum 24 patients). The disposition of patients is presented in Fig. 1.
The majority of the patients (299) were females (82.8%); 62 were males (17.2%). Relevant previous diseases and/or operations have been registered in 311 patients. Two hundred sixty-three patients had concomitant diseases and/or medications.
The vital signs did not show any abnormalities. The safety laboratory parameters were within the normal range except the following observations: Pathologic elevated values of clinical relevance are found in two patients (SGOT and SGPT in one patient), SGOT, SGPT and γ-GT in one patient—both in the group to get ASU), glucose (four patients, two each in both groups) and cholesterol (six patients, three each in both groups). These elevated values have been assessed to be neglectable for the aim of this study. There were also 5 patients with elevated ESR.
In 260 cases, both knees have been X-rayed, in 103 cases only one knee. In 339 cases, the X-ray has been performed in extension, in 13 cases in flexion and in 11 cases in both positions.
TheX-ray has been performed on the day of the examination or the next day in 97 cases. In 15 patients, the X-ray was performed before 1 week maximum, in 60 cases before 1 month maximum. In 56 cases, the X-ray was older than 1 month.
The osteoarthritis has been classified according to a modified Kellgren-scale [23]. Sixty-five patients (17.9%) belonged to stage I, 194 patients (53.4%) to stage II, and 104 patients (28.7%) to stage III.
Other known and radiologically confirmed arthrotic localisations (spine, hip, extremities) have been diagnosed in 121 patients. Demographic and other baseline characteristics are presented in Table 3.
Efficacy
The presented results are based on the ITT-population (see also Table 4). The mean decrease of the WOMAC index from baseline (visit 1) to visit 5 or to the end of the therapy was 546.0 ± 440.45 for ASU, and 587.3 ± 428.43 for chondroitin sulfate (Fig. 2). There is no difference between the two treatment groups (ANOVA p = 0.369).
The total WOMAC index as well as its subcategories decreases in both groups for approx. 50% from visit 1 to the end of therapy at visit 5. Also during the post-treatment observation there is a further slight improvement. There is no statistical significant difference between the treatment groups during the entire observation.
The Lequesne index decreases in both groups with a mean of 3.5 points from visit 1 to the end of therapy at visit 5. During the post-treatment observation there is a further slight improvement.
Pain on active movement, pain at rest and global assessment of knee osteoarthritis decreased in both groups to approx 50% of the initial value at the end of therapy, and remained unchanged until the end of the post-treatment period. There is no statistical significant difference between the treatment groups during the entire observation (Table 4).
Overall efficacy has been rated excellent and good in 80.8% of the ASU-treated patients by the investigator, and 80.2% by the patient. In the chondroitin group, the investigators rated better than the patients (85.3% versus 80.6%).
The daily intake of rescue medication has been reduced continuously during the treatment period, for 24% in the ASU group, for 22% in the chondroitin-group. A further reduction (18% in the ASU group, 17% in the chondroitin group) could be achieved in the post-treatment period (Fig. 3). There was no significant difference between the groups.
All efficacy parameter have been evaluated for both ITT and TPP groups. The results did not differ between the two groups.
The compliance was high in both treatment groups. The mean intake of medication was 101.5% ± 6.14 in the ASU group, and 102% ± 4.54 in the chondroitin-group.
Only two patients were not compliant according to the definition taking 58% and 63% of the required dosage, respectively. Both patients took the medication also less than 15 consecutive days between visits 4 and 5.
There was no centre-effect detectable when comparing both WOMAC index and Lequesne index. The results obtained in the centres were homogenous.
Safety
There were four serious adverse events reported. One patient (ASU group) died during the study (was found dead by her relatives at home), three patients (two ASU, one chondroitine) were hospitalized during the observation time. There was no connection with the treatments given.
Altogether 123 not serious adverse events in 81 patients have been reported (Table 5). There is no statistical significant difference between the two groups (p = 0.62; Fisher's exact test).
Neither laboratory analysis nor vital signs showed any clinically relevant treatment-related changes. In patients with initially elevated ESR, no relevant changes have been observed.
Overall tolerability was assessed by investigator and patient in 173 cases for ASU, and in 172 for chondroitin. The tolerability of the ASU treatment is assessed as excellent and good by the investigators in 96.0%, by the patients in 94.2%, of chondroitin in 98.8% and 96%, respectively. Moderate and poor tolerability for ASU is assessed in 4.1% by investigators, and 5.8% by patients, for chondroitin in 1.2% by investigators, and in 4.1% by patients.
Discussion
This prospective, controlled, randomized, multinational, multicentre, double-blind, double-dummy parallel-group clinical study in 364 patients over 6 months confirms previous data suggesting persistent and 2 months carry-over efficacy of ASU in patients with knee osteoarthritis.
ASU produced varying degree of symptomatic efficacy in several clinical studies in patients with osteoarthritis of the knee and hip [27–30].
In the study conducted by Blotman et al. 163 patients with osteoarthritis of the knee or hip received compulsory oral doses of NSAID for 3 months (one of the seven predefined NSAID) and 300 mg/daily ASU or placebo. The main evaluation criterion was the ratio of patients who returned to NSAID and the time elapsed between day 45 and the resumption. The difference for the whole set of patients was statistically significant between the two treatment groups (p < 0.001). Other assessment criteria (patient and physician global assessment, Lequesne functional index and severity of pain) showed the same trend with the exception of pain measured by a VAS scale [27].
Maheu et al. treated 164 patients with osteoarthritis of the knee (114) and hip (50) for 6 months and followed-up for an additional 2 months either ASU 300 or 600 mg (85 patients) or placebo (79 patients). The primary endpoints were the Lequesne index, pain, overall disability (rated on the visual analogue scale) and intake of NSAIDs. In this study, all parameters ameliorated significantly better in the ASU-treated group than in the placebo group, except NSAIDs intake reduction. The Lequesne score decreased from 9.7 ± 0.3 to 6.8 ± 0.4 in the avocado–soybean and from 9.4 ± 0.3 to 8.9 ± 0.4 in the placebo group. Less patient required NSAID treatment in the ASU (48%) than in the placebo group (63%). The subgroup analysis showed a more marked improvement in patients with hip osteoarthritis [28].
Appelbooom et al. treated 260 patients with knee osteoarthritis 300 or 600 mg daily ASU for 3 months. The primary endpoint (NSAIDs and analgesics intake) between days 30 and 90 decreased by more than 50% in 71% of the patients compared with 36% of the patients receiving placebo. Among the secondary endpoints the Lequesne functional index decreased from 9.6 ± 2.5 to 5.5 ± 3.6 and 9.8 ± 2.7 to 6.5 ± 3.5 points in ASU 300 and 600 mg groups, respectively, against 9.8 ± 2.4 to 7.8 + −3.4 in those receiving placebo [29].
Lequesne et al. in a placebo-controlled trial treated 163 patients with hip osteoarthritis with ASU for 2 years to evaluate the structure-modifying effect. One hundred and eight patients were radiologically evaluable at the end of the study but there was no difference in the joint space loss between the two groups. In a post-hoc analysis, they were able to demonstrate that avocado–soybean significantly reduced the joint space loss compared to placebo in the patient with advanced joint space narrowing [30].
Several systematic reviews on SYSADOA and a meta-analysis of ASU analyzed the results of previous studies [31–33].
Moe et al. performed an umbrella review of the previous meta-analysis. They found a low-quality evidence that ASU reduce pain in hip OA, and they concluded that further primary studies are needed [31].
Bruyere et al. found that ASU and other drugs of SYSADOA group have demonstrated pain reduction and physical function improvement. They highlighted the low toxicity rate of these drugs. This analysis was based on a critical review of three studies [27–29]. Contrary to the previous meta-analysis [31], they considered the quality of evidence with moderate to high [33].
Christensen et al. in their meta-analysis concentrated only to the efficacy of ASU in osteoarthritis. The study result was based on four manufacturer-supported trials [27–30]. In these trials, 664 patients with either hip (275) or knee (389) osteoarthritis were treated with 300 mg ASU (336) or placebo (328) with a mean treatment duration of 6 months (3–12 months). The pain reduction favoured ASU with an effect size of 0.39 (0.01–0.76) and the amelioration of Lequesne index also was better in the ASU treated group with an effect size of 0.45 (0.21–0.70). This is a modest, but clinically significant clinical effect. They calculated that one patient out of six [2, 4–7, 10–15, 19, 22–26, 28] was needed to be treated with ASU compared with placebo to have a benefit from the ASU treatment [32].
Chondroitin sulfate has been shown in numerous double-blind clinical trials to relieve pain and increase joint function and, possibly, be able to slow down progression of the disease.
In a study of Mazieres et al. 1 g/day of chondroitin sulfate was compared with placebo in the treatment of osteoarthritis of the knee in 130 patients. The treatment duration was 3 months. There was a significant improvement with respect to the Lequesne index. All variables tended towards a greater improvement in the chondroitin sulfate than in the placebo group and efficacy persisted one month after stopping medication [20].
Morreale et al. compared the efficacy of chondroitin sulfate and diclofenac in a randomized, multicenter, double-blind clinical study in 146 patients with osteoarthritis of the knee. Patients in the diclofenac group showed a prompt improvement of clinical symptoms, which, however, reappeared after the end of treatment. In the chondroitin sulfate group the therapeutic response appeared later in time but lasted for up to 3 months after the treatment [21].
Kahan et al. concluded from a placebo-controlled multicentre study in 622 patients over 2 years that chondroitin sulfate reduces significantly the progression of the joint space associated with a significant difference in the clinical findings in comparison to placebo [34].
Several meta-analysis on the effectiveness of chondroitin sulfate resulted in conflicting evidence. Leeb et al. found that the Lequesne index and the VAS for pain had improved by a mean of 50% in treated patients, but only by 20% in the controls [19]. In a more recent meta-analysis, however, Reichenbach et al. concluded after analysing 20 trials of varying duration (6–103 weeks) with altogether 3,846 patients with osteoarthritis of the hip or knee that chondroitin sulfate has minimal effect in joint pain, while the effects on joint space were inconclusive. In two thirds of the studies, 800–1,000 mg daily chondroitin sulfate was applied, less than in our study [35].
Pavelka et al. demonstrated that long-term (3 years) treatment with glucosamin sulfate retarded the progression of osteoarthritis of the knee, according to the radiographic minimum joint space measurements [36].
Meta-analysis of 19 studies over 1,328 diacerein—another member of the SYSADOA group—treated and 1,309 patients treated with a comparator showed that diacerein was significantly superior to placebo and equal efficacious to NSAIDs with a 3 months carry-over effects with excellent tolerability [37].
Although osteoarthritis is a localized disorder of the diarthrodal joints and lacks any signs of general inflammation, but some degree of local inflammatory activity can be shown by different methods during the course of the disease. In a histological study ninety percent of the cartilage specimens of knee and hip joints of patients with osteoarthritis contained pannus like tissue on the articular surface [38]. Furthermore, these pannus-like lesions showed similar qualitative metabolic characteristics and pro-inflammatory cytokine response like the pannus in rheumatoid arthritis [39]. During the course of osteoarthritis joint effusion, as sign of local inflammation often can be detected clinically, but also by ultrasonography and magnetic resonance imaging [40]. Further on, subchondral bone marrow lesions can be detected by MRI which is also suggestive of a local inflammation [41].
These findings point out the importance to inhibit the inflammatory cascade also in osteoarthritis. NSAIDs exert beside their analgesic properties a well known anti-inflammatory effect upon the inhibition of the prostaglandin production. Although the exact biochemical pathway responsible for the efficacy of ASU is not fully clarified, ASU in vitro demonstrated anti inflammatory properties in different test systems [11–18]. It inhibits the production of IL-1, prostaglandin E2, nitric oxide synthase and matrix metalloproteinase-13, and enhances the production of transforming growth factor and aggrecan [14, 15, 17, 42].
Osteoarthritis is a major public health problem in the world due to its prevalence, its impact of quality of life and its huge direct cost. Therefore the diagnosis and treatment of OA should be based on solid scientific evidences and cost-effective practice. Several international and national treatment recommendations have been developed to influence medical practice. In this respect it is important to clarify the position of ASU in the recommended treatment of OA.
In 2000 the EULAR recommendation for the management of knee osteoarthritis the authors stated that “SYSADOA may possess structure-modifying properties, but more studies using standardised methods are required.” In this recommendation, ASU was not mentioned among the drugs belonging to the SYSADOA group [43].
Three years later in a new recommendation, the authors go further by stating that the drugs belonging to SYSADOA—in this case including ASU too—have symptomatic effects and may modify structure. For ASU they calculated an effect size of 0.32–1.72 which is comparable to the traditional NSAIDs (0.47–0.96) and this recommendation based on 1B level of evidence [8].
Patient preference also in favour of effective but less toxic drugs in the treatment of chronic painful condition like OA. It was shown in a survey of primary care physicians prescribed traditional NSAIDs for the management of knee osteoarthritis, although the 54.3% of the patients used complementary medicines including drugs like the SYSADOA, especially glucosamine sulfate and chondroitin sulfate [44].
This is the first study that compares ASU 300 mg once daily and chondroitin sulfate 400 mg three times daily directly for efficacy, safety and carry-over effect. The results of this trial demonstrate that there is no difference in efficacy or in safety aspects between ASU and chondroitin sulfate. Also, the compliance was identical under these test conditions, in which all patients had to take four capsules daily over 6 months.
Pain and the parameters of the WOMAC index have been reduced in intensity for approximately 50% in both groups. Taking into consideration the results of Tubach et al. [45] that a relevant reduction in pain is achieved with approx. 40%, in WOMAC index in 26%, and in global assessment of the patient in 39%, a relevant improvement of the symptoms has been achieved in this trial after 3 months of treatment.
The results of this trial can add a further evidence on the effectiveness of ASU 300 mg in the treatment of osteoarthritis.
References
Cohen ZA, McCarthy DM, Kwak SD, Legrand P, Fogarasi F, Ciaccio EJ, Ateshian GA (1999) Knee cartilage topography, thickness, and contact areas from MRI: in-vitro calibration and in-vivo measurements. Osteoarthr Cartil 7(1):95–109
van Valburg AA, Wenting MJ, Beekman B, Te Koppele JM, Lafeber FP, Bijlsma JW (1997) Degenerated human articular cartilage at autopsy represents preclinical osteoarthritic cartilage: comparison with clinically defined osteoarthritic cartilage. J Rheumatol 24(2):358–364
Martini FH et al (2001) Fundamentals of anatomy and physiology, 5th edn. Prentice Hall, Upper Saddle River, New Jersey
Lequesne M, Brandt K, Bellamy N, Moskowitz R, Menkes CJ, Pclletier JP, Altman RD (1994) Guidelines for testing slow acting drugs in osteoarthritis. J Rheumatol 21(suppl 41):GS-73
Dougados M, Devogelaer JP, Annefeld M, Avouac B, Bouvenot G, Cooper C, the Members of the Group for the Respect of Ethics and Excellence in Science et al (1996) Recommendations for the registration of drugs used in the treatment of osteoarthritis. Ann Rheum Dis 55:552–557
Bellamy N, Kirwan J, Altman R, Boers M, Brandt KD, Brooks P, Dougados M, Lequesne M, Strand V, Tygwcll P (1997) Recommandations for a score set of outcome measures for future phase III clinical trials in knee, hip and hand osteoarthritis. Results of consensus development at OMERACT III. J Rheumatol 24:799804
Altman R, Brandt K, Hochberg M, Moskowitz R, Bellamy N, Bloch DA et al (1996) Design and conduct of clinical trials in patients with osteoarthritis: recommendations from a task force of the Osteoarthritis Research Society. Results of a Workshop. Osteoarthritis Cart 4:217–243
Jordan KM et al (2003) EULAR resommendations 2003: an evidence based approach to the management of knee osteoarthritis: Report of a Task Force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis 62:1145–1155
Zhang W et al (2008) OARSI Recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based expert consensus guidelines. Osteoarthr Cartil 16:137–162
Lequesne M (1994) Les anti-arthrosiques symptomatiques d'action lente: un nouveau concept therapeutique? Rev Rhum 61:75–79
Mauviel A, Daireaux M, Hartmann DJ, Galera P, Loyaux G, Pujol JP (1987) Effets des insaponifiables d'avocat et de soja (PIAS) sur la production de collagene par des cultures de synoviocytes, chondrocytes articulaires et fibroblastes dermiques. Rev Rhum Mal Osteoartic 56:207–211
Loyau G, Pujol JP, Mauviel A (1991) Effet des insaponifiables d'avocat/soja (Piascledine) sur 1'activite collagenolytique de culture de synoviocytes rhumatoides humains et de chondrocytes articulaires de lapin traites par 1'interleukine 1. Rev Rhum Mal Osteoartic 58:241-S
Mazieres B, Tempesta C, Tiechard M, Vaguier G (1993) Pathologic and biochemical effects of a lipidic avocado and soja extract (LASE) on an experimental post-contusive model of OA (abstract). Osteoarthr Cartil 1:46
Henrotin YE, Labasse AH, Jaspar JM, Dc Groote DD, Zheng SX, Guillou GB, Reginster JYL (1998) Effects of three avocado/soybean unsaponifiable mixtures on metalloproteinases, cytokines and prostaglandin E2 production by human articular chondrocytes. Clinical Rheum 17:31–39
Boumediene K, Bogdanowicz P, Felisaz N, Galera P, Pujol JP (1999) Avocado/soya unsaponifiables enhance expression of transforming growth factor and plasminogen activator inhibitor-1 in cultured articular chondrocytes. Arthritis Rheum 39:S227
Gabay O et al (2008) Stress-induced signaling pathways in hyaline chondrocytes: inhibition by Avocado–soybean unsaponifiables (ASU). Osteoarthr Cartil 16(3):373–384
Henrotin YE et al (2003) Avocado/soybean unsaponifiables increase aggrecan synthesis and reduce catabolic and proinflammatory mediator production by human osteoarthritis chondrocytes. J Rheumatol 30(8):1825–1834
Henrotin YE et al (2006) Avocado/soybean unsaponifiables prevent the inhibitory effect of osteoarthritic subchondral osteoblasts on aggrecan and type II collagen synthesis by chondrocytes. J Rheumatol 33(8):1668–1678
Leeb B, Schweitzer H, Montag K, Smolen JS (2000) A metaanalysis of chondroitin sulfate in the treatment of osteoarthritis. J Rheumatol 24:205–211
Mazieres B, Combe B, Phan-Van A, Tondut J, Grynfel M (2001) Chondroitin sulfate in osteoarthritis of the knee: a prospective, double blind, placebo controlled multicenter clinical study. J Rheumatol 28:173–181
Morreale P, Manopulo R, Galati M, Boccanera L, Saponati G, Bocchi L (1996) Comparison of the antiinflammatory efficacy of chondroitin sulfate and diclofenac sodium in patients with knee osteoarthritis. J Rheumatol 23:1385–1391
Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, Christy W, Cooke TD, Greenwald R, Hochberg M, Howell D, Kaplan D, Koopman W, Longley S, Mankin H, McShane DJ, Medsger T, Meeman R, Mikkelsen W, Moskowitz R, Murphy W, Rothschild B, Segal M, Sokoloff L, Wolfe F (1986) Development of criteria for the classification and reporting of osteoarthritis. Arthritis Rheum 29:1039–1049
Kellgren JH, Laurence JS (1957) Radiological assessment of osteoarthritis. Ann Rheum Dis 16:494–501
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW (1988) Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 15:1833–1840
Lequesne M, Mery C, Samson M, Gerard P (1987) Indexes of severity for osteoarthritis of the hip and knee. Scand J Rheumatol 65:85–89
Huskisson EC (1974) Measurement of pain. Lancet 2:1127–1131
Blotman F, Maheu E, Wulwik A, Caspard H, Lopez A (1997) Mid-term efficacy and safety of avocado and soya unsaponifiables (ASU) in the treatment of knee and hip osteoarthritis: results of a three-month prospective, randomized, double-blind, placebo-controlled, parallel-groups, multi-center clinical trial. Rev Rhum Engl Ed 64:825–834
Maheu E, Mazières B, Le Loët X, Loyau G, Valat JP, Grouin JM, Bourgeois P, Rozenberg S (1998) Symptomatic efficacy of avocado/soybean unsaponifiables in the treatment of osteoarthritis of the knee and hip. A prospective, randomized, double-blind, placebo-controlled, multicenter clinical trial with a six-month treatment period and a two-month follow-up demonstrating a persistent effect. Arthritis Rheum 41:81–91
Appelboom T, Schuermans J, Verbruggen H, Henrotin Y (2001) Symptoms modifying effect of avocado/soybean unsaponifiables (ASU) in knee osteoarthritis. A double-blind, prospective, placebo-controlled study. Scand J Rheumatol 30:242–247
Lequesne M, Maheu E, Cadet C, Dreiser RL (2002) Structural effect of avocado/soybean unsaponifiables on joint space loss in osteoarthritis of the hip. Arthritis Rheum 47:50–58
Moe RH, Haavardsholm A, Christie A, Jamtvedt G, Dahm KT, Hagen KB (2007) Effectiveness of nonpharmacological and nonsurgical interventions for hip osteoarthritis: an umbrella review of high-quay systematic reviews. Phys Ther 87:1716–1727
Christensen R, Bartels EM, Astrup A, Bliddal H (2007) Symptomatic efficacy of avocado-soybean unsaponifiables (ASU) in osteoarthritis (OA) patients: meta analysis of randomized controlled trials. Osteoarthr Cartil 16:399–408
Bruyere O, Burlet N, Delmas PD, Rizzoli R, Cooper C, Reginster JY (2008) Evaluation of symptomatic slow acting drugs in osteoarthritis using the GRADE system. BMC Musculoskelet Disord 9:165–174
Kahan A et al (1031) STOPP (Study on Osteoarthritis Progression Prevention): etude internationale, prospective, randomisée, en double insu, contrôlée contre placebo, évaluant la prévention de la progression radiologique de l’ arthrose du genou pendant deux ans avec la chontroitine 5 × 6 sulfate. Revue Rheum 2008:73
Reichenbach S et al (2007) Meta-analysis: chondroitin for osteoarthritis of the knee or hip. Ann Intern Med 146:580–590
Pavelka K, Gatterova J, Olejarova M, Machacek S, Giacovelli G, Rovati LC (2002) Glucosamine sulfate use and delay of progression of knee osteoarthritis: a 3 year, randomized, placebo-controlled, double-blind study. Arch Intern Med 162:2113–2123
Rintelen B, Neumann K, Leeb BF (2006) A Meta-analysis of Controlled Clinical Studies With Diacerein in Treatment of Osteoarthritis. Arch Intern Med 166:1899–1906
Shibakawa A, Aoki H, Masuko-Hongo K, Kato T, Tanaka M, Nishioka K et al (2003) Presence of pannus-like tissue on osteoarthritic cartilage and its histological character. Osteoarthr Cartil 11:133–140
Furuzawa-Carballeda J, Macip-Rodriguez PM, Cabral AR (2008) Osteoarthritis and rheumatoid arthritis pannus have similar qualitative metabolic characteristics and pro-inflammatory cytokine response. Clin Exp Rheumatol 26:554–560
Tarhan S, Unlu Z (2003) Magnetic resonance imaging and ultrasonographic evaluation of the patients with knee osteoarthritis: a comparative study. Clin Rheumatol 22:181–188
Hunter DJ, Zhang Y, Niu J, Goggins J, Amin S, LaValley MP et al (2006) Increase in bone marrow lesions associated with cartilage loss: a longitudinal magnetic resonance imaging study of knee osteoarthritis. Arthritis Rheum 54:1529–1535
Boileau C, Martel-Pelletier M, Caron J, Msika P, Gouillou GB, Baudouin C et al (2009) Protective effects of total fraction of avocado/soybean unsaponifiables on the sructural changes in experimental dog osteoarthritis: inhibition of nitric oxide synthase and matrix metalloproteinase-13. Arthritis Res Ther 11:R41
Pendleton A, Arden N, Dougados M, Doherty M, Bannwarth B, Bijlsma JWJ et al (2000) EULAR recommendations for the management of knee osteoarthritis: report of a task force of the Standing Committee for International Clinical Studies including Therapeutic Trials (ESCISIT). Ann Rheum Dis 59:936–944
Jordan KM, Sawyer S, Coakley P, Smith HE, Cooper C, Arden NK (2004) The use of conventional and complementary treatment for knee osteoarthritis in the community. Rheumatology 43:381–384
Tubach F et al (2005) Evaluation of clinically relevant changes in patient reported outcomes in knee and hip osteoarthritis: the minimal clinically important improvement. Ann Rheum Dis 64:29–33
Disclosures
None
Author information
Authors and Affiliations
Corresponding author
Additional information
The study has been supported by Laboratoire Expanscience, F-92400 Courbevoie, France.
An erratum to this article can be found at http://dx.doi.org/10.1007/s10067-010-1471-x
Rights and permissions
About this article
Cite this article
Pavelka, K., Coste, P., Géher, P. et al. Efficacy and safety of piascledine 300 versus chondroitin sulfate in a 6 months treatment plus 2 months observation in patients with osteoarthritis of the knee. Clin Rheumatol 29, 659–670 (2010). https://doi.org/10.1007/s10067-010-1384-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-010-1384-8