Abstract
Purpose
Persistent inguinal pain, influencing daily activities, is seen in about 5 % of patients following inguinal herniorrhaphy. Surgical treatment of patients with persistent postherniorrhaphy pain has been associated with pain relief and improvement in functional status. However, the detailed long-term outcome effects remain to be clarified. The aim of this study was to determine the long-term effects of mesh removal and selective neurectomy in patients with persistent postherniorrhaphy pain after previous open repair.
Methods
The study consecutively included 54 inguinal postherniorrhaphy pain patients treated with mesh removal and aimed neurectomy. Patients completed questionnaires evaluating pain intensity with a numerical rating scale (NRS) and pain-related functional impairment preoperatively, and, 3, 6, 12, 24, and 36 months postoperatively. Endpoints were changes in pain intensity and functional ability when comparing preoperative and postoperative assessments.
Results
Pain intensities (average, maximum, and during activity) were significantly lower at all time points during follow-up compared to preoperative values (p < 0.01 for all) with a reduction in median (IQR) average pain intensity from 6.0 (5.0–7.0) preoperatively to 3.0 (1.0–5.5) at 36-month follow-up. There was no association between positive pain outcome and intraoperative nerve identification (p = 0.47). The number of patients who reported a long-term negative effect of the operation (≥25 % increase in average pain intensity at 36-month follow-up) was 1 of 8. The functional ability was improved at 3 months after the operation (p < 0.01), but the improvement was not statistically significant in the follow-up period. Preoperative signs of depression, anxiety, and catastrophizing had no influence on outcome.
Conclusions
Mesh removal and attempted neurectomy may provide long-lasting analgesic effects in most patients and with a small proportion being worse, without relation to pain history and operative findings. Detailed multicenter collaboration is required to define preoperative diagnostics and the indication for mesh removal and neurectomy, the exact surgical procedure (type of neurectomy) and with detailed follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Persistent pain after open inguinal herniorrhaphy is a significant clinical problem causing long-term functional impairment in approximately 5 % of patients [1, 2]. Treatment options are limited but surgical exploration has demonstrated significant pain relief in the majority of published studies [3–12]. However, in most studies, interpretation is hindered by limited demographics, pain assessment, and functional consequences, and the different surgical approaches used, as well as a lack of detailed long-term follow-up [13, 14]. The primary aim of the present study was therefore to study 54 consecutive postherniorrhaphy pain patients, operated with a standardized surgical procedure, and with detailed questionnaires evaluating pain intensity and pain-related functional ability with a long-term follow-up.
Methods
Patients
The study was approved by the ethics committee of the Capital Region of Denmark and The Danish Data Protection Agency, and all patients gave written informed consent to participate in the study. The study comprised patients >18 years with inguinal pain, affecting daily activities, occurring after an open inguinal herniorrhaphy. Patients with a well-defined point of maximum pain located in the groin, and pain duration of more than 6 months, were included after clinical examination excluded a recurrence or other explanations to the chronic pain states and based upon thorough interdisciplinary discussion between an anesthesiologist, pain physician, and surgeon.
Surgical technique and anesthesia
One surgeon (HK) performed all operations. The surgical explorations were performed through the prior groin incision, and complete resection of the mesh and suture material was performed. Identification of the spermatic cord, the ilioinguinal nerve, the iliohypogastric nerve, and the genital branch of the genitofemoral nerve were attempted. In case of visually confirmed nerve entrapment by the mesh, scar tissue, sutures, or staples, the involved nerve was transected 3–5 cm proximal to the lesion and tissue samples were sent for histopathological examination. After mesh removal, a conventional Bassini repair was performed. All operations were carried out under general anesthesia with intravenous propofol, remifentanil, and sufentanil, and, additional wound infiltration with 20 ml of 0.5 % bupivacaine at completion of surgery. Postoperatively, the patients received oral acetaminophen 1 g every 6 h and ibuprofen 400 mg every 6 h for the first week.
Questionnaires
Preoperatively, and, during the follow-up 3, 6, 12, 24, and 36 months postoperatively, a questionnaire was sent to all patients. The questions evaluated pain intensity (pain at rest, average pain, maximum pain, and pain during activity) with a numerical rating scale (NRS 0–10, 0 = no pain, 10 = worst pain imaginable). Pain-related impairment of physical activities (light, moderate, and strenuous physical activities) was also assessed. The questionnaire in addition included psychometric assessments: the Hospital Anxiety and Depression Scale (HADS) [15] and the Pain Catastrophizing Scale (PCS) [16].
Data analysis
The percentage change in average pain intensity (NRS) from baseline (preoperative) to follow-up (3, 6, 12, 24, and 36 months after surgery) was calculated using the following formula:
We considered a pain reduction of at least 25 % to be a clinical relevant improvement after the surgical treatment. Therefore, we calculated the number needed to operate (NNO25) for 1 patient to achieve a reduction of ≥25 % in average pain intensity (NRS). Similarly, we calculated the number needed to operate (NNO50) for 1 patient to achieve a reduction of ≥50 % in average pain intensity (NRS). To assess a negative effect of the operation, the number needed to operate for 1 patient to experience an increase in pain after surgery (NNP25), defined by at pain increase of ≥25 % in average pain intensity (NRS), was calculated in an equivalent way.
Data analyses were performed using SPSS version 18.0 (SPSS, Chicago, IL, USA). Nonparametric statistics was applied. Wilcoxon signed-rank test was used to compare preoperative pain ratings, functional scores, PCS, and HADS with postoperative values at times of follow-up. Fisher’s exact test was used to compare proportions. Values are median (25–75 % interquartile range) unless otherwise stated. In order to minimize the likelihood of type I error, due to multiple comparisons, the significance level was set at p < 0.01.
Results
Demographics
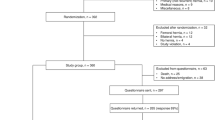
Fifty-six patients underwent surgical treatment for inguinal postherniorrhaphy pain between January 2007 and June 2011, and 54 patients were included in the analysis (Fig. 1). The median age of the patients at the time of surgery was 48 years (40–60 years) (Table 1). In 49 patients (91 %), the pain developed after a primary open groin herniorrhaphy and in 5 patients (9 %) after an open inguinal herniorrhaphy due to a recurrent hernia. Fourteen patients (26 %) had undergone different unsuccessful surgical explorations for pain relief before being referred to our institution. Results for the first 21 operated patients with 6-month follow-up have been reported previously [5].
Operative findings
Mesh/plug removal was performed in all patients except 2 patients where the mesh had been removed at a previous operation. In 20 patients (37 %), the mesh was found severely adherent to the spermatic cord. Results on nerve identification of the ilioinguinal, iliohypogastric and genitofemoral nerve and neurectomy, due to nerve entrapment, are presented in Table 2. In 44 patients (81 %), tissue samples suspected to involve nerve tissue were sent for histopathological examination. Samples in 39 (89 %) patients contained nerve tissue, but a neuroma was only observed in six of these cases.
Pain intensities
A significant reduction in pain intensities was observed after the operation. Thus, pain intensities (at rest, average, maximum, and pain during activity) were lower at all times during follow-up compared to preoperative values (p < 0.01 for all except pain at rest at 24 months where p = 0.1, Fig. 2; Table 3). The median average pain intensity declined from 6.0 (5.0–7.0) preoperatively to 4.0 (2.0–6.0) at 6-month follow-up and to 3.0 (1.0–5.5) at 36-month follow-up.
Pain intensities at rest (upper left panel), in average (upper right panel), as maximum (lower left panel), and during activity (lower right panel), preoperatively and during follow-up (3, 6, 12, 24, 36 months) after surgery. The horizontal lines indicate the median; boxes indicate 25–75 % interquartile range, and the whiskers represent the highest and lowest values that are not outliers. Outliers (values that are between 1.5 and 3 box lengths from either end of the box) are represented by circles beyond the whiskers. Wilcoxon signed-rank test used for paired comparisons with preoperative values (*p < 0.01, **p < 0.001)
The NNO25 were 1.5–1.9 during follow-up after surgery, demonstrating that more than 1 of 2 patients experienced a clinical relevant pain reduction of ≥25 % after the operation (Table 4). Furthermore, the NNO50 were between 2.5 and 3.7 at the various times of follow-up. Estimation of NNP25 demonstrated that the number of patients who reported a negative effect of the operation (≥25 % increase in average pain intensity) was 1 of 13 patients at 6-month follow-up and 1 of 8 patients at 36-month follow-up compared to preoperatively. There was no difference (p = 0.47) in the proportion of patient with positive surgical outcome (≥25 % average pain reduction assessed 3 months after the operation) when comparing 12 patients without identification of any of the three inguinal nerves during operation and 42 patients with identification of one or more inguinal nerves.
Functional scores
Assessment of pain-related functional impairment demonstrated a statistical significant improvement in functional ability at 3-month follow-up after the operation (Table 5). However, the improvement in functional ability diminished during follow-up and was only statistical significant, compared to preoperatively, for light physical activities up to 3-month follow-up, for moderate physical activities up to 6-month follow-up, and for strenuous physical activities up to 12-month follow-up after the operation.
Psychological factors
PCS was significantly higher preoperatively than at any time during follow-up (p < 0.01 for all comparisons, Table 6). No significant differences were observed when comparing preoperative scores of HADS anxiety and HADS depression with scores reported during follow-up (Table 6). There was no significant relationship between increased preoperative PCS, HADS anxiety or HADS depression scores and surgical outcome assessed at 3-month follow-up (p > 0.01 for all).
Complications
During follow-up, 4 patients had an inguinal hernia recurrence and were treated with a laparoscopic repair. Two patients had the testis impinged in the groin requiring orchidectomy in 1 patient. Two patients had ischemic orchitis with testicular atrophy (Table 2).
Discussion
As previously discussed [14], much of the literature on pain relief and functional outcomes after mesh removal or neurectomy for persistent postherniorrhaphy pain is inconsistent due to differences in surgical technique, follow-up method and limited information on the preoperative demographics. These methodological problems may to some extent explain the variability in success after such re-operations. In studies with a primary focus on neurectomy of the genitofemoral (genital branch) nerve, a successful outcome was reported in more than 80 % of patients [10, 11]; however, detailed objective assessments of pain and functional consequences were not reported. In 3 other studies with a predominant focus on the ilioinguinal nerve (and less so for the other nerves), successful results were observed in 50–100 % of patients [4, 7, 9], although 2 of these studies reported that about 25–30 % of patients had the same or worse pain postoperatively [4, 7]. In addition, one study [9] with 43 patients operated for “neuropathic” pain reported that nerve pathology was verified in 100 % of patients. Although the genital branch was not always dissected, the pain scores (median VAS) decreased from preoperatively 74 (range 53–87) to zero (range 0–34) postoperatively [9].
Detailed analysis of the available studies hinders exact interpretation of the value of preoperative diagnostics before the operation. The most detailed assessment in a follow-up study in 54 patients only demonstrated a triple neurectomy to be performed in 5 patients and neurectomy of the ilioinguinal nerve in 81 %, the genital branch in 46 %, and the iliohypogastric nerve in 17 % of patients [4]. The strength of this study, that demonstrated 52 % of patients being pain free or almost pain free, compared to 24 % having unchanged or increased pain, was a response rate to a detailed follow-up questionnaire of 91 %. Other authors have shown excellent results of triple neurectomy in a large group of patients [8] but with limited details on the follow-up regarding response rate and method of pain assessment and functional consequences. Based on the surgical studies, no specific information or interpretation is possible regarding the importance of mesh removal per se.
The present study, with detailed, repeated postoperative questionnaires and a follow-up up to 3 years is in agreement with most of the above cited studies demonstrating an overall benefit of the reoperation, despite a non-complete demonstration of removed nerve tissue. Therefore, the question of surgical expertise in identification and possibility for neurectomy needs to be addressed [8, 10] and may potentially explain the differences in outcome results. However, the studies do not allow specific explanation for the differences between studies in nerve identification [4–12]. Nevertheless, a greater proportion of patients having benefit of reoperation than having an unchanged or deteriorating condition support the increased attention to reoperation with mesh removal and neurectomy. However, for conclusive interpretation of the long-term outcomes reported in this study, the spontaneous reduction in pain and functional complaints seen in about 50 % in patients with severe pain after 6-year follow-up compared to 1-year follow-up [17] must be addressed.
Limitations
Short-term follow-up of the first 21 patients has previously been presented, including a more detailed assessment of functional outcome, than in the present study [5]. Detailed analyses of compiled data from the 54 patients revealed chronological inconsistencies in the questionnaires, and therefore, a condensed version of the functional outcome score was used, with uniform and common assessments recovered from all 54 patients.
Conclusion
In conclusion, based upon the results of the present study and those reported in the literature, surgical treatment with either mesh removal or triple or selective neurectomy seems to be beneficial in a large proportion of patients. However, due to diversity of patient demographics, preoperative diagnostics, specific type of surgical intervention, and details for follow-up, future research will require larger patient series, probably within the context of multicenter studies and with identical methodology to allow sufficient interpretation in regard to which patients benefit from reoperation and which patients do not.
References
Aasvang E, Kehlet H (2005) Chronic postoperative pain: the case of inguinal herniorrhaphy. Br J Anaesth 95:69–76
Simons MP, Aufenacker T, Bay-Nielsen M et al (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13:343–403
Amid PK (2004) Causes, prevention, and surgical treatment of postherniorrhaphy neuropathic inguinodynia: triple neurectomy with proximal end implantation. Hernia 8:343–349
Loos MJ, Scheltinga MR, Roumen RM (2010) Tailored neurectomy for treatment of postherniorrhaphy inguinal neuralgia. Surgery 147:275–281
Aasvang EK, Kehlet H (2009) The effect of mesh removal and selective neurectomy on persistent postherniotomy pain. Ann Surg 249:327–334
Keller JE, Stefanidis D, Dolce CJ, Iannitti DA, Kercher KW, Heniford BT (2008) Combined open and laparoscopic approach to chronic pain after inguinal hernia repair. Am Surg 74:695–700
Zacest AC, Magill ST, Anderson VC, Burchiel KJ (2010) Long-term outcome following ilioinguinal neurectomy for chronic pain. J Neurosurg 112:784–789
Amid PK, Hiatt JR (2007) New understanding of the causes and surgical treatment of postherniorrhaphy inguinodynia and orchalgia. J Am Coll Surg 205:381–385
Vuilleumier H, Hubner M, Demartines N (2009) Neuropathy after herniorrhaphy: indication for surgical treatment and outcome. World J Surg 33:841–845
Amid PK, Chen DC (2011) Surgical treatment of chronic groin and testicular pain after laparoscopic and open preperitoneal inguinal hernia repair. J Am Coll Surg 213:531–536
Giger U, Wente MN, Buchler MW, Krahenbuhl S, Lerut J, Krahenbuhl L (2009) Endoscopic retroperitoneal neurectomy for chronic pain after groin surgery. Br J Surg 96:1076–1081
Delikoukos S, Fafoulakis F, Christodoulidis G, Theodoropoulos T, Hatzitheofilou C (2008) Re-operation due to severe late-onset persisting groin pain following anterior inguinal hernia repair with mesh. Hernia 12:593–595
Hakeem A, Shanmugam V (2011) Current trends in the diagnosis and management of post-herniorrhaphy chronic groin pain. World J Gastrointest Surg 3:73–81
Aasvang E, Kehlet H (2005) Surgical management of chronic pain after inguinal hernia repair. Br J Surg 92:795–801
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67:361–370
Sullivan MJL, Bishop SR, Kivik J (1995) The pain catastrophizing scale: development and validation. Psych Assess 7:524–532
Aasvang EK, Bay-Nielsen M, Kehlet H (2006) Pain and functional impairment 6 years after inguinal herniorrhaphy. Hernia 10:316–321
Acknowledgments
The research leading to these results is part of the European Collaboration, which has received support from the Innovative Medicines Initiative Joint Undertaking, under Grant Agreement No 115007, resources of which are composed of financial contribution from the European Union’s Seventh Framework Programme (FP7/2007-2013) and EFPIA companies’ in kind contribution. The authors thank Morten Bay-Nielsen for surgical collaboration.
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bischoff, J.M., Enghuus, C., Werner, M.U. et al. Long-term follow-up after mesh removal and selective neurectomy for persistent inguinal postherniorrhaphy pain. Hernia 17, 339–345 (2013). https://doi.org/10.1007/s10029-013-1073-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-013-1073-z