Abstract
The objective of the study was to compare the use of attention deficit hyperactivity disorder (ADHD) medication among children and adolescents in Scandinavia 2010–2020. Using aggregated prescription data for individuals aged 5–19 years, we calculated annual prevalence proportions of ADHD medication (users/1000 inhabitants) for each country, overall and stratified by age and sex. Overall, use of ADHD medication increased during 2010–2020 in all countries. The increase was pronounced in Sweden reaching 35 users/1000 inhabitants in 2020 (119% increase), whereas it reached 22/1000 in Denmark and Norway (equivalent to a 38% and 16% increase, respectively). Methylphenidate was the most frequently used drug and Sweden had the highest use reaching 25/1000 in 2020 compared to 16/1000 and 18/1000 in Denmark and Norway, respectively. Lisdexamfetamine use increased steadily and was also highest in Sweden (13/1000 in 2020). In 2020, atomoxetine use was higher in Sweden (4.6/1000) and Denmark (4.5/1000) compared to Norway (2.2/1000). From 2015, use of guanfacine increased in Sweden reaching 4.4/1000 in 2020 but remained low in Denmark (0.4/1000) and Norway (0.7/1000). Use of dexamphetamine was low (ranging from 0.47 to 0.75/1000 in 2020) in the three countries. ADHD medication use was highest in Sweden across all age groups. In all countries, the prevalence was higher in males compared to females. In conclusion, use of ADHD medication among children and adolescents in Scandinavia is increasing. The prevalence of use is higher in Sweden for all drug groups compared to Norway and Denmark.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Attention deficit hyperactivity disorder (ADHD) is a frequent childhood psychiatric disorder with an estimated overall prevalence of 5% among 6–17 year olds in Europe [1]. Medications to treat ADHD have proven efficient in reducing ADHD symptoms in numerous clinical trials [2]. For the past decades, the number of children and adolescents receiving treatment with ADHD medications has increased worldwide, primarily due to an increase in the use of methylphenidate [3, 4]. However, variations in the trends and in the prevalence of ADHD medication use between the Scandinavian countries have been described [4, 5]. As an example, from 2008 to 2012, the prevalence of ADHD medication use remained rather stable in Norway while it showed a u-shaped increase in Denmark (with a levelling off from 2010) and a steady increase in Sweden. By 2012, the prevalence was highest in Sweden [4].
New pharmacological agents have continuously been marketed and as of 2021, three acting centrally acting stimulants (lisdexamfetamine, dexamphetamine, and methylphenidate) and two non-stimulants (atomoxetine and guanfacine) are approved for treatment of childhood ADHD in the Scandinavian countries. Methylphenidate is considered first line pharmacological treatment in Sweden, while Norwegian guidelines emphasize that choice of drug must be made based on an individual evaluation of benefits and risks [6, 7]. A recent Danish guideline recommends methylphenidate, atomoxetine, lisdexamfetamine, or dexamphetamine to children with major functional impairment based on an individual evaluation [8]. However, reimbursement for atomoxetine, lisdexamfetamine, guanfacine, and dexamphetamine requires that methylphenidate has proven insufficient or is contraindicated rendering methylphenidate the most common first choice treatment [9].
Centrally acting stimulants, such as methylphenidate, have the potential of leading to misuse and abuse. It is a well-known phenomenon among students where stimulants can be used to increase performance [10]. The introduction of new pharmacological treatment options within recent years might interfere with the utilization patterns. Careful screening of the utilization trends with updated data on ADHD medication use is needed to guide initiatives to facilitate rational use of these drugs. Therefore, we aimed to describe the trends in use of ADHD medications among children and adolescents including age and sex differences in Denmark, Norway, and Sweden between 2010 and 2020.
Methods
This study was a descriptive drug utilization study covering the entire Scandinavian population aged 5–19 years from 2010 to 2020.
Data sources
We used information from the three publicly available national prescription databases [11,12,13] that include information on all prescribed drugs dispensed to individuals at pharmacies. Drug information is coded according to the Anatomical Therapeutic Chemical (ATC) classification codes. The databases hold information on number of medication users each year according to sex and age. Information on amount of drug dispensed, expressed in defined daily doses (DDDs), was available in the Danish and Norwegian database [11, 12]. Swedish data on amount of dispensed drug in DDD for methylphenidate and atomoxetine was obtained from the Swedish health authorities. DDD is a unit of quantity defined by the World Health Organization (WHO) [14].
Study population and study medications
The study cohort constituted the entire population aged 5–19 years in Denmark, Norway, and Sweden between January 1st 2010 and December 31st 2020. In the year 2020, the study population covered 3.75 million inhabitants [15]. Due to a very low prevalence of use among patients 0–4 years of age (results not presented), this group was not included in the study. We included the following medications licensed for ADHD treatment in any of the three countries: dexamphetamine (ATC N06BA02), lisdexamfetamine (N06BA12), methylphenidate (N06BA04), atomoxetine (N06BA09), and guanfacine (C02AC02). Further, ‘centrally acting sympathomimetics’ (N06BA) was analyzed as a group and termed ‘any ADHD medication’. N06BA included the following drugs: amphetamine (N06BA01), dexamphetamine, methylphenidate, lisdexamfetamine, atomoxetine, modafinil (N06BA07), and solriamfetol (N06BA14). Use of modafinil, amphetamine, and solriamfetol among children and adolescents in the three countries was negligible during the study period. Methylphenidate is available in both extended and immediate release formulations but a distinction between the two was not possible in the data sources. An individual was defined as a user if at least one prescription for any of the medications listed above was filled within a given year. If an individual filled a prescription for more than one of the included medications, the individual was considered a user of all the relevant medications. Some study medications were marketed later than January 1st 2010 and were included in the analyses consecutively during the study period. An overview of year of marketing authorization is presented in supplementary (Table S1).
Analyses
We calculated the annual prevalence of use for each ADHD medication in each country from January 1st 2010 to December 31st 2020. In addition, the annual prevalence of use of any ADHD medication was calculated. The number of individuals aged 5–19 years in each country per year by January 1st was used as the denominator. Further, for each country, we stratified the annual prevalence of ADHD medication use by age groups (5–9, 10–14, and 15–19 years) and sex, and calculated a male/female ratio for each age group. The number of individuals in the relevant age and sex group in each country per year by January 1st was used as the denominator. For all analyses, the prevalence was presented as the number of users per 1000 individuals.
We estimated the annual coverage of ADHD drug treatment in Norway and Denmark by calculating (1) the annual mean amount of drug dispensed in DDDs per user per day and (2) annual total amount of drug dispensed in DDDs from 2010 to 2020 stratified by the five ADHD medications. In addition, the analyses on amount of drug dispensed in DDDs in 2020 were stratified by age groups and sex. For Sweden, analyses on amount of drug dispensed in DDDs were performed for methylphenidate and atomoxetine only as the information was not available for the other drugs.
All statistical analyses were performed using STATA Release 17.0 (StataCorp, College Station, TX, USA).
Results
Use of ADHD medication 2010–2020
During the study period, use of ADHD medication increased in all three countries. Sweden had the highest relative increase (119%) from 16 users/1000 inhabitants in 2010 to 35/1000 in 2020. This was followed by Denmark (38% relative increase: from 16/1000 to 22/1000) and Norway (16% relative increase: from 19/1000 to 22/1000) (Fig. 1).
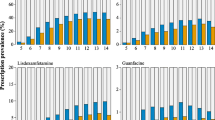
The higher use of ADHD medication in Sweden compared to Denmark and Norway applied to all age groups except for atomoxetine among 15–19 year olds and dexamphetamine among 10–14 year olds, where use was slightly higher in Denmark (Fig. 2). Male/female ratios, stratified by ADHD medication, age groups and country, are presented for 2020 in supplementary (Fig. S1). Across ADHD medications and countries, the male/female ratio was > 1 but the male/female ratio decreased with increasing age. We observed no noticeable changes in the male/female ratio across the study period (results not presented).
Use of all five individual ADHD medications increased during the study period, however, most notably for methylphenidate and lisdexamfetamine (Fig. 1 and S2). Methylphenidate was the most commonly used ADHD medication during the study period and use increased in all countries, most distinctly in Sweden (79% increase: from 14 users/1000 in 2010 to 25/1000 in 2020). In Norway, the prevalence of methylphenidate use was relatively stable across the study period with a slight increase from 2019 (3.9%), reaching 18/1000 in 2020. In Denmark, use of methylphenidate decreased by 14% from 2012 to 2016 followed by an increase of 16% reaching 16/1000 in 2020 (Fig. 1). There was a low but increasing use of dexamphetamine (1514% increase in Sweden, 14,225% in Denmark, and 117% in Norway) in all countries during the study period (in 2020; Sweden 0.75/1000, Denmark 0.70/1000, and Norway 0.47/1000) (Fig. S2). Following its introduction to the market, lisdexamfetamine use increased in all countries and in 2020, the use was highest in Sweden (23,884% increase: 13/1000) compared with Norway (2025% increase: 5.2/1000) and Denmark (758% increase: 5.0/1000) (Fig. 1). Atomoxetine use was stable during the study period (2.0–2.2/1000) in Norway but increased in Sweden (reaching 4.6/1000 in 2020 equivalent to a 34% increase) and Denmark (reaching 4.5/1000 in 2020 equivalent to a 69% increase) (Fig. S2). Use of guanfacine increased by 8952% from 2015 in Sweden reaching 4.4/1000 in 2020. In Denmark and Norway, guanfacine use was low but increased (by 310% and 798%, respectively) to 0.45/1000 and 0.67/1000, respectively, in 2020 (Fig. S2). Annual prevalence for Scandinavia in total is presented in supplementary (Fig. S3).
Quantity of dispensed ADHD medication
The quantity of dispensed ADHD medication per user per day during the study period is presented in Table 1. The quantity of individually dispensed methylphenidate decreased in all three countries from 2010 to 2020 (0.93 to 0.75 DDD/user/day in Sweden, 1.1 to 0.79 in Norway, and 1.1 to 0.91 in Denmark). For atomoxetine, the quantity dispensed decreased slightly during the study period in Norway and Sweden (from 0.39 to 0.31 and 0.36 to 0.34 DDD/user/day, respectively) and increased slightly in Denmark (from 0.41 to 0.47 DDD/user/day). The quantity of dispensed dexamphetamine decreased in Denmark (from 0.55 to 0.24 DDD/user/day) and Norway (from 0.67 to 0.32 DDD/user/day). For lisdexamfetamine, DDD/user/day increased reaching 0.94 in Denmark and 0.77 in Norway in 2020. A similar trend was observed for guanfacine, where DDD per user per day increased from 0.44 to 0.76 in Denmark and from 0.24 to 0.64 in Norway.
The quantity of dispensed ADHD medication stratified by sex and age groups in 2020 is presented in supplementary (Table S2). Applying to all medications, males received higher DDD/user/day as compared to females with two exceptions in Norway: dexamphetamine among 10–14 year olds and lisdexamfetamine among 5–9 year olds. DDD/user/day was < 1 for dexamphetamine, atomoxetine, and guanfacine for all age groups and sex. A similar trend was seen for methylphenidate and lisdexamfetamine with few exceptions among 15–19 year olds in Denmark.
Of all ADHD medications, methylphenidate was prescribed in the largest quantity across the study period in Denmark and Norway (Fig. 3). However, its proportional share of the total quantity of ADHD medication dispensed decreased during the study period from 94 to 67% in Denmark and from 95 to 73% in Norway. The proportional share of the total quantity of drug use accounted for by lisdexamfetamine increased in Denmark from 1.3% in 2013 to 21% in 2020 and in Norway from 0.5% in 2014 to 21% in 2020 (Fig. 3). The proportional share of atomoxetine use was larger in Denmark compared to Norway during the study period (Fig. 3). This analysis was not conducted with Swedish data as information on amount of dispensed drug was available for methylphenidate and atomoxetine only, and not for all ADHD medications.
Discussion
In this study, we found an increasing use of ADHD medication, especially methylphenidate and lisdexamfetamine, among children and adolescents from 2010 to 2020 in the three Scandinavian countries. In all three countries, methylphenidate was the most frequently used ADHD medication, but the extent and trend of use over time varied markedly across the countries. The change in use of methylphenidate was more pronounced in Sweden compared to Denmark and Norway where we noticed less fluctuations over time. Lisdexamfetamine use increased in all countries following market approval, however, most notably in Sweden. There were small but marked differences in the use of guanfacine across the three countries, while use of dexamphetamine and atomoxetine was low and stable in all countries. Across all types of ADHD medication, Sweden had the highest use during the last 5 years.
Following previous studies on use of ADHD medication in the Nordic countries [4, 16, 17], we document a continued increase in the use of ADHD medication among children and adolescents in all Scandinavian countries throughout the last decade. The trends in Scandinavia are thus in accordance with those described in other countries, e.g., China [18]. However, in some countries the use of ADHD medication has been found to be stable or even decreasing [19, 20]. We found that the variation in use of ADHD medication between the Scandinavian countries persisted after 2012. In Denmark, the use decreased from 2012 to 2016 after which it increased. In Norway, it was stable but with an increasing trend from 2019 to 2020. Lastly, in Sweden, the use was stable from 2014 to 2018 but increased markedly afterwards. While we have no possible explanations for the trends in the use of methylphenidate in Norway and Sweden, the decreasing use of methylphenidate in Denmark after 2012 could be explained by an increased attention towards the risk/benefit profile of methylphenidate in adults [21] and a discussion in lay-media of potential adverse events associated with long-term treatment [22].
Guanfacine, dexamphetamine, and lisdexamfetamine were approved for treatment of ADHD during the study period and use increased following their market approval, particularly in Sweden. In Denmark and Norway, where information on amount of dispensed drug in DDDs was available, lisdexamfetamine seemed to have increased its share of the total drug use at the expense of methylphenidate. For guanfacine and dexamphetamine, we observed use before the marketing authorization, which is possibly explained by compassionate use permits and use of drugs produced at pharmacies, i.e., magistral medicinal products. When interpreting the results, it should be kept in mind that the date of market approval does not necessarily coincide with January 1 of the relevant year. Data coverage on magistral medicinal products is not complete and, therefore, the extent of use before authorization is unknown. Hence, the presented results prior to approval should be interpreted with caution.
The Scandinavian countries’ healthcare legislations, standards of living, and economic situations are rather similar and the persisting national variation in use of ADHD medication is thus surprising. However, variation in ADHD medication use could reflect national differences in the prevalence rates of ADHD. Up to 4.3% and 1.7% of all 6–17-year-old Norwegian boys and girls were registered with a diagnosis of ADHD from 2008 to 2013 [23]. In Denmark, the number of children diagnosed with ADHD reached 2% in 2016 [24]. The Swedish National Board of Health and Welfare estimated that 9% of boys and 4.5% of girls had an ADHD diagnosis in 2020 [17]. Hence, a higher prevalence of children with severe ADHD in Sweden could explain our results, but methodological differences in the existing literature challenges direct comparison of ADHD prevalence rates between the Scandinavian countries.
As suggested in previous studies [25, 26], it is possible that the variation in use of ADHD medication is caused by differences in the availability of mental health care specialists. A study from 2020 found that the number of child and adolescent psychiatrists per inhabitant was approximately twice as high in Sweden compared to Denmark and Norway [27]. Further, differences in prescribing practices, treatment duration, and the extent of non-pharmacological interventions across countries could account for the observed differences. It is possible that patients with ADHD who have easier access to mental health care, more frequently switch to another ADHD medication. This would lead to a higher prevalence in use of the different ADHD medications. The observed higher use of second-line treatments like lisdexamfetamine and guanfacine in Sweden could support this assumption. In addition, Swedish patients seem to receive ADHD treatment for longer time periods compared to recent years [17]. If this change is not paralleled in Denmark and Norway, it could contribute to a relatively higher prevalence of use in Sweden. Given the rather homogenous populations and the observed variation in ADHD medication use across the Scandinavian countries, future studies should aim to unfold the reasons for these variations.
In general, there was a higher use of ADHD medication among males compared to females and a decreasing male/female ratio with increasing age in all three countries. This is in accordance with previous findings and knowledge on diagnostic patterns [3, 5, 28] and reflects that ADHD is diagnosed more often in males compared to females [29]. The decreasing male/female ratio with increasing age might reflect that females are diagnosed with ADHD later than males which is also supported by previous research [30]. No significant differences between the countries were observed. Applying to all ADHD medications, males received higher DDD/user/day compared to females. This suggests that males received higher doses or were treated for longer periods, which could reflect higher severity or more extrovert symptoms (e.g., hyperactivity).
Important strengths of the study comprise use of three complete nationwide study populations with publicly available data which eliminates selection and recall bias. The study had several limitations. The analyses were based on filled prescriptions as proxies for use of ADHD medication, however, it is unknown whether the patients actually consumed the medication. Further, aggregate-level data does not provide information on duration of treatment. Previous data have shown that up to 12.6% of ADHD medication users only fill a prescription once [31], and, therefore, the prevalences reported in this study are most likely an overestimate of the number of users in actual treatment with ADHD medication. No information on treatment indication was available and it is possible that some patients received their medication due to, e.g., narcolepsy. However, as the prevalence of narcolepsy is low among children, we suspect this to be a minor issue. In addition, we were unable to discriminate between prevalent and incident users and information on amount of dispensed drug in DDDs was not available for all medications in Sweden. Lastly, the Scandinavian countries have national clinical guidelines that are quite similar regarding pharmacological treatment of ADHD and all emphasize the importance of non-pharmacological interventions [6,7,8]. Our study did not investigate the extent of psychological or educational initiatives targeted towards subjects with ADHD, and national variation in non-pharmacological treatment interventions might explain our results.
Conclusion
The use of ADHD medication is still increasing among children and adolescents in the Scandinavian countries and clear differences in use exist, with Sweden having the highest use of all five ADHD medications. Methylphenidate is the most frequently used medication and use of lisdexamfetamine is increasing across all countries.
Data availability
The data that support the findings of this study are openly available at Zenondo.org (specific link will be inserted). The data were derived from the following data resources: https://sdb.socialstyrelsen.se/if_lak/val.aspx, www.norpd.no, www.medstat.dk, and https://www.ehalsomyndigheten.se/statistik-och-lakemedelsforsaljning/bestalla-statistik/.
Change history
25 October 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00787-022-02100-9
References
Wittchen HU, Jacobi F, Rehm J et al (2011) The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol 21:655–679. https://doi.org/10.1016/j.euroneuro.2011.07.018
Cortese S, Adamo N, Del Giovane C et al (2018) Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: a systematic review and network meta-analysis. Lancet Psychiatry 5:727–738. https://doi.org/10.1016/S2215-0366(18)30269-4
Raman SR, Man KKC, Bahmanyar S et al (2018) Trends in attention-deficit hyperactivity disorder medication use: a retrospective observational study using population-based databases. Lancet Psychiatry 5:824–835. https://doi.org/10.1016/S2215-0366(18)30293-1
Furu K, Karlstad Ø, Zoega H et al (2017) Utilization of stimulants and atomoxetine for attention-deficit/hyperactivity disorder among 5.4 million children using population-based longitudinal data. Basic Clin Pharmacol Toxicol 120:373–379. https://doi.org/10.1111/bcpt.12724
Zoëga H, Furu K, Halldórsson M et al (2011) Use of ADHD drugs in the Nordic countries: a population-based comparison study. Acta Psychiatr Scand 123:360–367. https://doi.org/10.1111/j.1600-0447.2010.01607.x
Swedish Medical Products Agency Swedish Medical Products Agency (2016) Läkemedel vid adhd—behandlingsrekommendation. Available at https://www.lakemedelsverket.se/sv/behandling-och-forskrivning/behandlingsrekommendationer/sok-behandlingsrekommendationer/lakemedel-vid-adhd--behandlingsrekommendation
Helsedirektoratet Helsedirektoratet (2016) ADHD/Hyperkinetisk forstyrrelse—Nasjonal faglig retningslinje for utredning, behandling og oppfølging [nettdokument]. Oslo: Helsedirektoratet. Available at https://www.helsedirektoratet.no/retningslinjer/adhd.
Danish Health Authority (2020) National clinical guideline for the assessment and treatment of ADHD in children and young people (Udredning og behandling af ADHD hos børn og unge: national klinisk retningslinje). Available at https://www.sst.dk/da/udgivelser/2021/nkr-adhd-hos-boern-og-unge
ADHD: Methylphenidat, atomoxetin, lisdexamfetamin og guanfacin. In: Lægemiddelstyrelsen. Available at https://laegemiddelstyrelsen.dk/da/tilskud/individuelle-tilskud/enkelttilskud/vejledende-kriterier/adhd-methylphenidat,-atomoxetin,-lisdexamfetamin-og-guanfacin/. Accessed on 9 Dec 2021
Clemow DB, Walker DJ (2014) The potential for misuse and abuse of medications in ADHD: a review. Postgrad Med 126:64–81. https://doi.org/10.3810/pgm.2014.09.2801
Schmidt M, Hallas J, Laursen M, Friis S (2016) Data resource profile: Danish online drug use statistics (MEDSTAT). Int J Epidemiol 45:1401–1402g. https://doi.org/10.1093/ije/dyw116
The Norwegian Institute of Public Health (NIPH). Norwegian prescription database
Socialstyrelsen. Statistikdatabas för läkemedel (Statistical database, pharmaceuticals)
World Health Organization (2022) WORLD HEALTH ORGANIZATION. Guidelines for ATC classification and DDD assignment 2022. WHO Collaborating Centre for Drug Statistics Methodology
Nordic Statistics Database
Karlstad Ø, Zoëga H, Furu K et al (2016) Use of drugs for ADHD among adults—a multinational study among 15.8 million adults in the Nordic countries. Eur J Clin Pharmacol 72:1507–1514. https://doi.org/10.1007/s00228-016-2125-y
Socialstyrelsen (2021) Förskrivningen av adhd-läkemedel fortsätter att öka. Available at https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/ovrigt/2021-6-7436.pdf. 7
Wang Z, Wu X, Yu Z, Yu L (2022) Utilization of drugs for attention-deficit hyperactivity disorder among young patients in China, 2010–2019. Front Psychiatry. https://doi.org/10.3389/fpsyt.2021.802489
Beau-Lejdstrom R, Douglas I, Evans SJW, Smeeth L (2016) Latest trends in ADHD drug prescribing patterns in children in the UK: prevalence, incidence and persistence. BMJ Open 6:e010508. https://doi.org/10.1136/bmjopen-2015-010508
Grimmsmann T, Himmel W (2021) The 10-year trend in drug prescriptions for attention-deficit/hyperactivity disorder (ADHD) in Germany. Eur J Clin Pharmacol 77:107–115. https://doi.org/10.1007/s00228-020-02948-3
Vurdering af sikkerheden ved brug af methylphenidat til behandling af ADHD. In: Lægemiddelstyrelsen. Available at https://laegemiddelstyrelsen.dk/da/udgivelser/2010/vurdering-af-sikkerheden-ved-brug-af-methylphenidat-til-behandling-af-adhd/. Accessed on 4 Feb 2022
(2012) Ingen kender fremtiden for Ritalin-brugere. In: Information. Available at https://www.information.dk/indland/2012/06/ingen-kender-fremtiden-ritalin-brugere. Accessed on 24 Nov 2021
Folkehelseinstituttet (2016) ADHD i Norge En statusrapport. Available at https://www.fhi.no/globalassets/dokumenterfiler/rapporter/2017/adhd_i_norge.pdf
Danish Health Authority Prævalens, incidens og aktivitet i sundhedsvæsenet for børn og unge med angst eller depression, ADHD og spiseforstyrrelse
Wesselhoeft R, Jensen PB, Talati A et al (2020) Trends in antidepressant use among children and adolescents: a Scandinavian drug utilization study. Acta Psychiatr Scand 141:34–42. https://doi.org/10.1111/acps.13116
Wesselhoeft R, Rasmussen L, Jensen PB et al (2021) Use of hypnotic drugs among children, adolescents, and young adults in Scandinavia. Acta Psychiatr Scand 144:100–112. https://doi.org/10.1111/acps.13329
Barrett E, Jacobs B, Klasen H et al (2020) The child and adolescent psychiatry: study of training in Europe (CAP-STATE). Eur Child Adolesc Psychiatry 29:11–27. https://doi.org/10.1007/s00787-019-01416-3
Siffel C, Page M, Maxwell T et al (2020) Patterns of lisdexamfetamine dimesylate use in children, adolescents, and adults with attention-deficit/hyperactivity disorder in Europe. J Child Adolesc Psychopharmacol 30:439–447. https://doi.org/10.1089/cap.2019.0173
Rucklidge JJ (2010) Gender differences in attention-deficit/hyperactivity disorder. Psychiatr Clin North Am 33:357–373. https://doi.org/10.1016/j.psc.2010.01.006
Murray AL, Booth T, Eisner M et al (2019) Sex differences in ADHD trajectories across childhood and adolescence. Dev Sci 22:e12721. https://doi.org/10.1111/desc.12721
Pottegård A, Bjerregaard BK, Kortegaard LS, Zoëga H (2015) Early discontinuation of attention-deficit/hyperactivity disorder drug treatment: a Danish nationwide drug utilization study. Basic Clin Pharmacol Toxicol 116:349–353. https://doi.org/10.1111/bcpt.12325
Acknowledgements
Anton Pottegaard is acknowledged for his assistance and discussion of the study idea and final analyses. Niels Bilenberg is acknowledged for his assistance with interpreting the results.
Author information
Authors and Affiliations
Contributions
RW and LR conceived the study idea. AMSS, RW, JR, CEC, KF, IH, and LR designed the study and directed the analyses, which were carried out by JHA. AMSS, RW, LR, CEC, JHA, and JR retrieved the data. AMSS, RW, and LR drafted the first manuscript. All authors participated in the discussion and interpretation of the results. All authors critically revised the manuscript and approved the final version of the article. All listed authors meet authorship criteria.
Corresponding author
Ethics declarations
Conflict of interest
Johan Reutfors and Carolyn Cesta are employed at the Centre for Pharmacoepidemiology, Karolinska Institutet, which receives grants from several entities (contract research organizations, regulatory authorities, and pharmaceutical companies including AbbVie, AstraZeneca, Bayer, Janssen, Pfizer, Servier, and Takeda) for performance of drug safety and drug utilization studies, with no relation to the work reported in this paper. The other authors did not receive support from any organization for the submitted work.
Ethical approval
The aggregated data used for this study are publicly accessible in the three countries and, therefore, approval from ethical committees or data protection agencies was not needed.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sørensen, A.M.S., Wesselhöeft, R., Andersen, J.H. et al. Trends in use of attention deficit hyperactivity disorder medication among children and adolescents in Scandinavia in 2010–2020. Eur Child Adolesc Psychiatry 32, 2049–2056 (2023). https://doi.org/10.1007/s00787-022-02034-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-022-02034-2