Abstract
Gender identity represents a topic of growing interest in mental health research. People with non-conforming gender identity are prone to suffer from stigmatization and bullying and often present psychiatric issues, which may in turn lead to a high prevalence of suicidal ideation and behaviors. The present meta-analysis aimed to estimate the prevalence of suicidal ideation and suicidal behaviors in gender non-conforming children, adolescents and young adults. A systematic search was performed in Web of Science and PsycINFO from inception to December 2018. We selected cross-sectional and cohort studies including youths (up to 25 years) with a diagnosis confirmed by a clinician according to international classifications, or after a direct interview with a peer. A random-effects meta-analysis was computed for the following outcomes: non-suicidal self-injury (NSSI), suicidal ideation and suicide attempts. Overall, we found a mean prevalence of NSSI of 28.2% (9 studies, 3057 participants, 95% CI 14.8–47.1). A similar prevalence (28%) was found for suicidal ideation (6 studies, 2249 participants, 95% CI 15–46.3), while the prevalence of suicide attempts was 14.8% (5 studies, 1039 participants, 95% CI 7.8–26.3). Subgroup analyses revealed no significant differences according to biological sex. Given the prevalence of suicidal behaviors in gender non-conforming youths, it appears desirable to implement therapeutic and support strategies for this population. Moreover, educational interventions directed to parents, teachers, mental health professionals and general community should be promoted to struggle against stigma and social isolation, factors that may contribute to increasing the risk of suicidal behaviors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gender identity can be defined as the personal sense of one’s own gender [1]. Disorders related to gender identity represent a topic of growing interest for mental health professionals, particularly considering the number of diagnostic refinements occurred over the last years [2]. After abandoning the expressions of transsexualism and gender identity disorder (GID), adopted in previous editions of the Diagnostic and Statistical Manual of Mental Disorders (DSM), the DSM-5 has finally introduced the concept of gender dysphoria. Gender dysphoria refers to the distress felt by a person due to a mismatch between their gender identity and their biological sex [3]. Moreover, while gender identity was previously considered to be dichotomous (male/female), in DSM-5, this concept is better described as a multi-category or a spectrum [4, 5].
More recently, the International Classification of Diseases (ICD-11) has proposed the notion of gender incongruence, which corresponds to a marked and persistent incongruence between an individual's experienced gender and the assigned sex [6]. A remarkable difference from DSM-5 gender dysphoria is that gender incongruence does not require to cause significant distress or impairment. Additionally, in ICD-11, gender incongruence has been moved from the “Mental and behavioral disorders” chapter to the new section “Conditions related to sexual health” [6]. Another umbrella term, frequently used in scientific literature and among the general public, is transgender (often shortened as trans) which indicates a gender identity or gender expression that differs from the sex assigned at birth. The opposite of transgender is cisgender, which describes individuals whose gender identity or expression matches their biological sex. In general, all the conditions described above can be included among the so-called “gender non-conforming identities” [1].
Given the rapid changes occurred in diagnostic classifications and terminology, the debate around non-conforming gender identities has been very animated over the last years. Along with the different conceptualizations, prevalence estimates of gender non-conforming individuals are inconsistent [7, 8]. The DSM-5 reports that the prevalence of gender dysphoria would range between 0.005 and 0.014% for birth-assigned males, and between 0.002 and 0.003% for birth-assigned females regardless of age [3]. However, these data are probably underestimated, since they only rely on those people who seek for gender affirmative treatments in specialty clinics (i.e. hormonal treatment or surgery). A meta-analysis by Collin et al. reported widely varying estimates in the general population: prevalence would range from 0.092%—when considering only people who required gender affirmative treatment—to 3.5%—when referring to individuals who self-identified as transgenders. Focusing on the groups of interest for the present paper, the prevalence of gender incongruence among children has been estimated to be around 1.3% [8]. Other studies have suggested that between 1.6 and 2.7% of youths would identify themselves as gender non-conforming or transgenders [9, 10], with much higher prevalence among biological females (3.6%) than biological males (1.7%) [8].
Gender non-conformity can manifest across all age groups, with different clinical presentations. In children, cross-gender behaviors may start between the ages of 2 and 4, the same age at which most typically developing children begin showing gendered behaviors and interests. In prepubertal individuals, non-conforming gender may be expressed through clothes, activities, games and friendships [3]. While some children express feelings and behaviors relating to gender non-conformity during early childhood, many may not express clear cross-gender behaviors until puberty or much later. Some children may not accept the body changes which typically occurs during puberty. In gender non-conforming adolescents, clinical features may resemble those of children or adults with the condition, depending on developmental level. Accordingly, the incongruence between experienced gender and biological sex is a central feature of the diagnosis [3]. Nevertheless, gender atypical behavior is common among young children and may be part of the normal development, and many children do not continue to experience gender incongruence into adolescence and adulthood. In fact, it has been shown that only a part of youngsters with gender dysphoria continue to report distress and seek services for gender reassignment later in life [11]. Some research has shown that children with more intense symptoms and more persistent in their cross-gender statements and behaviors seemed to be more likely to become transgender adults [11, 12].
Even if according to the most recent classification (i.e. ICD-11), gender incongruence should not be longer considered a mental disorder per se, it certainly represents a vulnerability factor for the development of social and psychological issues. Young people with gender incongruence often present associated problems, such as bullying [13], stigma [14], difficult relationships with parents or peers [15]. Moreover, this population shows high rates of psychiatric morbidities, such as anxiety, mood disorders or substance abuse [9, 16]. The so-called “minority stress” theory could explain, at least in part, the enormous psychosocial difficulties encountered by gender non-conforming people. This model affirms that stigma, prejudice, and discrimination directed to sexual and gender minorities in our society would create a stressful environment that may provoke serious mental health problems [17, 18]. In fact, the stress perceived by gender non-conforming people, such as the chronic exposure to transphobic stereotypes, stigma, and discriminations, may lead to produce a constant conflict between how a person perceives herself and how she is evaluated by others [17]. For instance, minority stress may favor the internalization of homophobic thoughts, thus leading to the negative self-perceptions by those persons who do not conform to binary gender [19]. In consequence of minority stress, gender non-conforming youths may experience more frequently suicidal ideation, with a higher number of attempted suicides, as well as of non-suicidal self-injury (NSSI) and deliberate self-harm. For example, a recent meta-analysis reported that sexual minority youngsters were 3.5 times at higher risk of attempted suicide [20], and that, more specifically, transgender youths had an increased risk of 5.87 times to attempt suicide compared to cisgender peers, as reported by only one study [21].
Despite the interest of clinicians and researchers for gender-related disorders is rapidly growing, there is still a dearth of knowledge about the phenomenon of suicidality in young people with non-conforming gender identity. A recent large epidemiological study conducted by the Center for Disease Control and Prevention (CDC), involving 131,901 high school students in the United States, showed that suicidal ideation and suicide attempts were significantly higher in adolescents who self-defined as transgender than in cisgender peers, with a prevalence of suicidal ideation of 43.9% and a prevalence of attempted suicide of 34.6% in the previous 12 months among the former [9]. In 2016, a systematic review reported that transgender people had a higher prevalence of NSSI and suicidality compared to the cisgender population. According to the authors, there were also some differences, with biological females being at a greater risk for NSSI behaviors than biological males [22]. More recently, Mann et al. [23] reviewed the prevalence of self-injurious thoughts and behaviors in gender-diverse children and young people in the United Kingdom, essentially confirming the results of the previous review. However, to the best of our knowledge, no updated meta-analyses have been published. Therefore, the aim of the present paper was to critically summarize the current evidence on the topic, in order to estimate the actual magnitude of suicidal ideation and suicidal behaviors in youths with non-conforming gender identity.
Methods
Search strategy
We performed a systematic search following the PRISMA Statement guidelines [24]. We searched Web of Science™ and PsycINFO from inception to December 2018. We used the following search terms: (transsexual OR transgender OR “gender dysphoria” OR “gender identity disorder” OR “gender incongruence”) AND (selfharm OR “self-harm” OR “self-injur*” OR “self-injur*” OR NSSI OR suicide* OR “non suicid*” OR mortality). The search strategy was not restricted to any language, reference type or year of publication. The electronic searching was supplemented by hand-searching of reference lists of the included review articles to identify any additional source.
Study selection
First, two researchers (VC and CA) screened titles and abstracts to identify potentially relevant studies. Then, the authors assessed full texts to determine eligible studies; each researcher worked independently and in duplicate. Any doubt was solved through consultation with a third author (LF). We included only original articles written in English, fulfilling the following criteria:
-
1.
Participants: we included studies recruiting children, adolescents and young adults (up to 25 years) with non-conforming gender identity. Participants who had received a diagnosis of gender dysphoria, gender identity disorder, transsexualism or gender incongruence by a clinician and/or according to valid international diagnostic criteria (i.e. DSM or ICD) were included. Moreover, we included transgender individuals (without a formal clinical diagnosis), only if they have been directly interviewed by a clinician or a trained peer or if it was demonstrated that they were in charge to a health center for transgender people. We excluded participants who were not interviewed in person, such as individuals who had responded to online surveys without a direct or proven evaluation by a clinician or a trained peer.
-
2.
Comparison: if present, the cisgender population (i.e. people whose gender identity and gender expression align with sex assigned at birth) was considered as control group.
-
3.
Outcomes: studies that included the prevalence of suicide rates or suicide attempts or suicidal ideation or non-suicidal self-injury (NSSI) for the selected population.
-
4.
Study design: we selected cohort studies, retrospective studies or case–control studies.
Data collection and extraction process
Data have been extracted in a pre-piloted form by two review authors (TS and RM), working independently and in duplicate. Any doubt was solved through consultation with a third reviewer (LF). The following variables were considered:
-
1.
Study characteristics: author, year, country, study design, methodology of data collection;
-
2.
Participants’ characteristics: age (mean age and age range), biological sex, diagnosis and diagnostic method, sample size (this information was extracted also for the control group, if present);
-
3.
Outcomes: prevalence of suicide, suicidal ideation, suicide attempts and NSSI (extracted as number of events in the overall sample, occurred during the lifetime).
Quality assessment
The Joanna Briggs Institute (JBI) Critical Appraisal checklist for Prevalence Studies was used to evaluate the studies quality [25]. Each study was reviewed independently by two researchers (AR, PB). Any doubt was solved after consultation with a third review author (LF). The JBI checklist is composed by the following ten questions:
-
1.
Was the sample representative of the target population?
-
2.
Were study participants recruited in an appropriate way?
-
3.
Was the sample size adequate?
-
4.
Were the study subjects and setting described in detail?
-
5.
Is the data analysis conducted with sufficient coverage of the identified sample?
-
6.
Were objective, standard criteria used for measurement of the condition?
-
7.
Was the condition measured reliably?
-
8.
Was there appropriate statistical analysis?
-
9.
Are all important confounding factors/subgroups/differences identified and accounted for?
-
10.
Were subpopulations identified using objective criteria?
Similar to a well-conducted meta-analysis on prevalence recently published [26], we divided the checklist questions in three domains: participants (questions 1, 2, 4, 9, and 10), outcome measurement (6 and 7), and statistics (3, 5, and 8). An included study was considered as having high quality when all domains were methodologically accurate, i.e. when we answered “yes” to all questions.
Strategy for data synthesis
We provided a narrative synthesis of the study characteristics. Moreover, we computed meta-analyses for each outcome using a random-effects model. We pooled the event rate and sample size and calculated the 95% confidence intervals and the two-sided p values for each outcome. Heterogeneity between studies was assessed using the Cochrane Q and I2 statistics. Thresholds for the interpretation of heterogeneity were consistent with those of the Cochrane Collaboration (I2 0–40%: might not be important; 30–60%: may represent moderate heterogeneity; 50–90%: may represent substantial heterogeneity; 75–100%: considerable heterogeneity) [27]. When data regarding biological sex (i.e. M-to-F or F-to-M) were available, a subgroup analysis for each outcome was performed. All statistical analyses were conducted using Comprehensive Meta-Analysis (CMA) v. 2.2.
Results
Search results and selection process
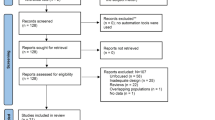
Our search yielded a total of 1068 articles, while 5 papers were retrieved from other sources. After duplicates removal, we screened a total of 911 abstracts. The full texts of 179 papers were examined in detail in order to assess the fulfillment of inclusion criteria. After a careful examination of full-texts, 73 studies were excluded because participants had a self-reported diagnosis or studies were conducted through online surveys; in 47 studies the sample did not include children, adolescents or young adults up to 25 years; 23 studies did not examine the selected outcomes (suicide rates, suicidal ideation, NSSI or suicide attempts); 12 papers were abstracts, reviews or articles not written in English; 9 studies did not have an appropriate design; finally, in 5 papers data regarding the gender-diverse population were not reported distinctly from those of the lesbian, gay and bisexual population. In conclusion, 10 articles were included both in the qualitative and in the quantitative synthesis. Details about the study selection process have been reported in the PRISMA flow diagram (Fig. 1).
Characteristics of included studies and participants
We finally included ten studies, among which nine were cross-sectional and one was a historical cohort study [28]. Studies were conducted mainly in the United States and in the United Kingdom. One study was multicentric and was conducted in UK, USA and Australia [28], while one study was conducted in Japan [29]. Only two studies [28, 30] compared the prevalence of suicidal behaviors in the sample of interest to a control group; therefore, we decided not to consider controls in the meta-analyses.
Samples of youngsters with non-conforming gender identity varied from 55 [31] to 1082 [30], while control samples were generally larger, including 911 [28] and 21,317 [30] cisgender individuals. Participants were diagnosed with gender dysphoria in seven studies. Exceptions were Grossman et al. [31] that recruited transgender individuals, Thorne et al. [32] that recruited people with a diagnosis of gender incongruence, and Becerra-Culqui et al. [30] in which participants were diagnosed with transsexualism or gender identity disorder. Studies mostly included mixed samples of children, adolescents and young adults, with ages ranging from 3 to 25 years. All studies, except from Aitken et al. [28] and Terada et al. [29] reported the presence and/or prevalence of psychiatric comorbidities. Only in four studies [33,34,35,36], the transition period of participants was specified. Characteristics of included studies and participants have been described in detail in Table 1.
Outcome measures
Outcome measurement was different across studies: three papers evaluated suicidal behaviors through a direct clinical interview [29, 31, 34], while in three articles, electronic medical records [30] or clinical charts [35, 37] were consulted. Scales were administered in four out of ten studies. Specifically, in two papers, [28, 36], the authors used the Child Behavior Checklist (CBCL), a widely used caregiver report form identifying problem behaviors in children [38]. One paper [33] used the Suicidal Ideation Questionnaire, a 30-item self-report tool specifically developed to screen suicidal ideation in adolescents [39]. Finally, Thorne and colleagues [32] used the Self-Injury Questionnaire—Treatment Related (SIQ-TR), a self-report questionnaire used to measure the type, frequency, and duration of self-injurious behaviors [40]. Outcome measures are reported in Table 1.
Lifetime prevalence of suicide attempts, suicidal ideation, and NSSI in gender non-conforming youths
Overall, we found a mean prevalence of NSSI of 28.2% (9 studies, 3057 participants, 95% CI 14.8–47.1). Heterogeneity was low (Q = 6.75, df = 8, I2 = 0%). A similar prevalence (28%) was found also for suicidal ideation, even if this outcome was reported in a lower number of studies (6 studies, 2249 participants, 95% CI 15–46.3). Heterogeneity was low (Q = 7.13, df = 5, I2 = 29.84%). Finally, the prevalence of suicide attempts was of 14.8% (5 studies, 1039 participants, 95% CI 7.8–26.3), with low heterogeneity (Q = 3.69, df = 4, I2 = 0%). The meta-analyses are reported in Fig. 2.
Subgroup analyses revealed no significant differences according to biological sex (M-to-F vs. F-to-M) in none of the considered outcome (NSSI: Q = 0.67, df = 1, p = 0.413; suicidal ideation Q = 0.001, df = 1, p = 0.981; suicide attempts: Q = 0.383, df = 1, p = 0.536).
Appraisal of quality
According to the Joanna Briggs Institute (JBI) Critical Appraisal checklist for Prevalence Studies, only two of ten studies were rated as having high quality [30, 33] (i.e. they had good quality in all domains); the others had limitations in at least one of the three pre-specified domains (participants, outcome measurement, and statistics).
Considering participants, we judged the sample of three studies [31, 34, 36] not representative of the entire population (Question 1). Specifically, Nahata et al. [34] and Spack et al. [36] recruited individuals in endocrinology clinics, with subjects presumably at a later stage of the transition period, and thus not representative of the whole population of non-conforming gender youngsters; additionally, in Grossman et al. [31], participants were recruited from social and recreational service agencies for LGBT (Lesbian, Gay, Bisexual, and Transgender) youth. For the same reason, the recruitment method of the latter study (Question 2) was not considered appropriate, as the sampling strategy could limit the generalizability of results. Seven out of ten studies described in detail the participants (Question 4) included in the sample, that could, therefore, be considered comparable to the population of interest. Three papers [34,35,36] did not identify all important confounding factors or subgroups (Question 9). Moreover, in one study [34], subjects were mostly white, and all identified themselves as binary; therefore, findings may not apply to non-white or nonbinary transgender youths. Objective criteria have been used to identified subpopulations and subgroups in almost all the articles (Question 10); nevertheless, three studies [34,35,36] did not identify important subgroups and differences as ethnicity.
As far as concerns outcome measurement, all papers identified objective, standard criteria (Question 6). However, in two studies [35, 37], the authors recorded the outcome on the basis of clinical records, raising concerns about a possible risk of under-reporting suicidal behaviors and ideation (Question 7); conversely, this issue has been addressed by Becerra-Culqui et al. [30].
Finally, in seven studies [31,32,33,34,35,36,37], the sample size was not adequate (Question 3) and in two papers [31, 34], data analysis was not conducted with sufficient coverage of the identified sample (Question 5). Statistical analysis (Question 8) was judged not methodologically accurate in two studies [34, 36]. Quality of the included studies according to the JBI Critical Appraisal has been reported in Table 2.
Discussion
Main findings
The present paper aimed to systematically review the prevalence of suicidal ideation and behaviors in gender non-conforming youths. Our findings showed that the prevalence of suicidal ideation, suicide attempts and NSSI are much higher compared to the general population and specifically to cisgender youths, regardless of the presence of psychiatric issues. For instance, literature reports that the pooled prevalence of suicidal ideation would be around 25% considering all children and young people in charge of mental health services, and around 11% of peers not in care. Also, the prevalence of suicide attempts would be 3.6% in children and young people in care and 0.8% in the non-clinical population [41]. Concerning NSSI, Muehlenkamp et al. [42] recently estimated a prevalence of 18% among adolescents of the general population. Notably, all the rates found in the population of interest of our meta-analyses are much higher than those reported above.
Of note, our results are in line with a recent epidemiological survey conducted in the United States, showing that transgender high school students have a significantly higher prevalence of suicidal ideations and attempts compared to their cisgender counterparts [9]. Also, we replicated the results of a previous systematic review [23] examining suicidality and self-harm in transgender youths, explaining also the magnitude of this phenomenon. Overall, our findings confirm that suicidal behaviors in people with non-conforming gender identity should be considered an important issue by mental health professionals.
The high rate of suicidal behaviors could be explained by both social and biological reasons. First, the theory of “minority stress” could at least in part explain this increase in suicidal ideation and behaviors. According to this theory, the psychopathological issues of people with non-conforming gender identity would be related to the presence of a stressful environment [17, 18]. In fact, many studies have shown that transgenders are subjected to a great amount of stigma by the society in general, and in particular by peers, teachers and family members, also receiving less support than their cisgender counterparts. Literature has provided evidence that gender-diverse youths experience more bullying at school than their peers [43], also reporting a link between gender-based victimization at school and suicidal behaviors [44]. Of note, parental stigma can be perceived worse than other forms of stigma and may be the result of different factors, such as a low educational level, religious beliefs, and the sense of guilt and loss for the child. Furthermore, many families feel blamed or shamed by society for their child’s gender non-conformity [45]. Family rejection has in turn been related to a higher probability of being homeless, engaging in sex activities at risk, and also to an increased risk of depression and suicidality [46]. Therefore, favoring measures for inclusion of gender-diverse youngsters may help them accept their diversity [47].
From a biological point of view, the stigma surrounding children, adolescents and young adults with gender incongruence and the bullying behaviors may cause an increase in cortisol levels, which in turn could explain the high prevalence of suicidal behaviors and self-injury. In fact, the literature has reported that the vulnerability to suicidal behavior could have a correlation with hypothalamic–pituitary–adrenal (HPA) axis [48], as cerebrospinal and plasma cortisol levels are higher in people who attempted suicide than controls. Interestingly, a decreased hippocampal glucocorticoid receptor expression has also been reported in suicide victims with childhood trauma indicating that environmental events associated with increased HPA activity enhance the risk of suicide [49]. For this reason, we could hypothesize that the increased plasma cortisol levels, consequential to the minority stress, could influence the risk of suicidal behaviors. In fact, preliminary evidence has suggested that stigma affects HPA axis functioning among sexual minority individuals specifically [50].
Another significant factor potentially linked to the high prevalence of both suicidality and self-harm in gender non-conforming youths is related to the elevated rates of psychiatric morbidities, which are more common and often more severe than in the gender-conforming counterparts [30]. This finding has been confirmed also by the studies included in our review: depression and anxiety appeared highly prevalent in the included samples, followed by attention deficit-hyperactivity disorder (ADHD), bipolar disorder and eating disorders. All these psychiatric conditions are typically associated with an increased risk of suicidality and NSSI [51]. In particular, it has been shown that some disorders, such as ADHD [52], eating disorders and substance abuse [53], are associated with high levels of impulsivity that, in turn, could represent a risk factor for suicidal behaviors [54].
Finally, transition into puberty could be even more challenging and difficult for gender non-conforming children as they become increasingly uncomfortable with the changes in their body and self-esteem is seriously affected by this transformation [55].
Limitations
To our knowledge, this is the first meta-analysis to specifically examine the prevalence of suicidal behaviors in young people with non-conforming gender identity. Nevertheless, our review presents several limitations. First, the number of included studies, and thus of the number of participants, is low. Second, the studies included in the meta-analysis were quite heterogeneous for several reasons. For instance, data for children, adolescents and young adults were often mixed, hampering the possibility to conduct separate analyses for the different age groups; therefore, we cannot exclude that the rates of suicidal conducts might be variable between children, adolescents and young adults. This is true also for the presence of mental health conditions: the inclusion of individuals with psychiatric diagnoses of different types, as well as subjects without any psychiatric comorbidity, may have partially confounded the results. Moreover, participants were in different transition periods: this is another important limitation to take into consideration, since gender affirmative treatments may help individuals to cope with their difficulties, thus changing the risk of suicidal behaviors. In relation to heterogeneity, it is also worth underlying that the continuous and rapid updates of classifications and terminology did not allow us to include homogeneous groups in term of diagnosis, diagnostic criteria, and levels of impairment (i.e. people with gender incongruence and transgender individuals do not necessarily feel distressed for their condition). Notably, we included only studies in which the diagnoses were clinical or in which participants were interviewed in person: therefore, we excluded those youngsters who simply self-identified as transgender responding to online surveys. On one hand, this restriction undoubtedly limited the number of studies included in the meta-analysis; on the other hand, our selection criteria reduced the risk of including misdiagnosed individuals or people completing self-report surveys without external direct control. Another important source of heterogeneity was represented by the outcome measures used in the studies, which were sometimes self-reported, in some cases deducted from clinical charts, and in others ascertained through a direct clinical interview.
Furthermore, only two of the selected papers compared the prevalence of suicidal behaviors in the gender non-conforming sample to those of cisgender peers: for this reason, it was not possible to insert these data in the meta-analysis. Also, we evaluated only the lifetime prevalence: this was due to the non-conformity of included studies, which measured the outcome across different timespans. Therefore, we could not investigate the prevalence in specific periods of time, as it is possible that the risk of suicidal behaviors increases in specific age groups or according to specific life events or stressors. Finally, it is worth underlining that the studies included in our review were conducted exclusively in Western nations, and mainly in English-speaking countries. This could represent a bias since estimates in other populations, such as in developing countries, might be slightly different.
Implications for clinical practice and future research
Our review represents a first attempt to clarify an emerging challenge for mental health professionals and researchers. As the prevalence of suicidal and self-injurious behaviors in gender non-conforming youths is much higher than in the general population and in cisgender peers, it appears of primary importance to elucidate the causes and the mechanisms underlying this phenomenon, in order to prevent suicidal conducts in this group at-risk.
The development of specific psychoeducational therapies for gender non-conforming youths and their families might be useful to help them cope with the stress related to social discrimination and stigma. Indeed, minority stress theory recognizes the important roles of social support and coping in moderating the impact of stress. Since parents usually help the child getting medical treatment of any kind, it is crucial, for the general well-being of gender non-conforming children, to have their parents understanding and supporting their needs in this particularly delicate period of life. Therefore, therapy might be essential not only for gender-diverse youths, but also for their parents, to help them process their feelings and learn how to accept, support and protect their child. In fact, minority stress theory suggests that members of some socially stigmatized communities, such as young people with gender incongruence, are not likely to share their stigmatized status with their families and may not experience family or community support [56, 57]. This is a potential limitation to the possibility of openly expressing themselves and may force them to shape their behaviors according to the dominant gender-normative culture [58].
Notably, gender-affirmative interventions, capable of interrupting the influence of minority stress, are the only evidence-based therapies for young people with gender incongruence. In fact, the approaches traditionally used to address psychological distress (e.g. cognitive-behavioral therapy) often do not adequately consider some of the identity-specific stressors perceived by this group of people [58]. Gender-affirmative interventions assume that gender is not binary and that gender-diverse expressions and identities are part of the expected human diversity and not pathological [59]. The gender-affirmative model provides an individualized and comprehensive approach to ensure gender-diverse youths and their families to receive not only medical and mental health treatment when indicated, but also adjunctive services for the social adjustment of the individual in different contexts (e.g. with peers, at school, in the community) [59]. Recently, a group coping skills intervention tailored on the experiences of sexual and gender minorities has been implemented, to help them improve their mood and coping skills by teaching them how to identify, challenge, and change maladaptive thoughts, beliefs, and behaviors [58, 60].
Since non-conforming gender identity is a rapidly evolving concept, researchers should implement studies with well-characterized and homogeneous samples, including participants who have been evaluated by clinicians and not only through indirect surveys, possibly belonging to the same age group and in the same transition period. It would be extremely interesting to understand how suicidal ideation and behaviors are related to the levels of functional and social impairment, as well as to the quality of life and to the stigma perceived by both young people with non-conforming gender identities and their families. Also, there is the urgent need of longitudinal studies investigating whether suicidal behaviors and ideation may improve after a comprehensive and integrated care program, consisting not only in a psychological and medical support of the child, but also of the family and the educational environment. At this regard, a notable issue is related to the outcome measures, which should be standardized, reliable, and replicable at different time points (e.g. before and after a psychosocial intervention or hormonal therapy). Studies should be conducted in different countries, for instance non-English-speaking countries, where individuals with non-conforming gender identity might be even more stigmatized and scarcely accepted by the society, due to cultural or religious beliefs.
It would be desirable to implement programs to educate both the general population and mental health professionals to the existence of non-conforming gender identities also in childhood and adolescence. More specifically, teachers, parents, and educators should become aware of the condition, in order to recognize it and refer youths to appropriate medical centers. In turn, the creation of specific services for young people could help to improve the knowledge of the multiple aspects and difficulties of individuals with gender incongruence, to help them learn to accept their diversity.
Young people who refer to services for gender incongruence probably represent only “the tip of the iceberg”, since there is still much stigma and poor knowledge of the condition. Future research should consider the important issue of suicidality in gender non-conforming youths in order to sensitize both the general population and mental health professionals about this crucial topic.
References
American Psychiatric Association (2019) Guidelines for psychological practice with transgender and gender nonconforming people. Am Psychologist 70:832–864
Beek T, Cohen-Kettenis PT, Kreukels BPC (2016) Gender incongruence/gender dysphoria and its classification history. International Review of Psychiatry. Int Rev Psychiatry 28:5–12
American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders, 5th edn. American Psychiatric Association, Arlington, VA
Cohen-Kettenis PT, Pafflin F (2010) The DSM diagnostic criteria for gender identity disorder in adolescents and adults. Arch Sex Behav 39:499–513
Zucker KJ, Cohen-Kettenis PT, Drescher J, Meyer-Bahlburg HF, Pfäfflin F, Womack WM (2013) Memo outlining evidence for change for gender identity disorder in the DSM-5. Arch Sex Behav 42:901–914
Reed GM, Drescher J, Krueger RB, Atalla E, Cochran SD, First MB et al (2016) Disorders related to sexuality and gender identity in the ICD-11: revising the ICD-10 classification based on current scientific evidence, best clinical practices, and human rights considerations. World Psychiatry 15:205–221
Collin L, Reisner SL, Tangpricha V, Goodman M (2016) Prevalence of transgender depends on the “case” definition: a systematic review. J Sex Med 13:613–626
Zucker KJ (2017) Epidemiology of gender dysphoria and transgender identity. Sex Health 14:404–411
Johns MM, Lowry R, Andrzejewski J, Barrios LC, Demissie Z, McManus T et al (2019) Transgender identity and experiences of violence victimization, substance use, suicide risk, and sexual risk behaviors among high school students—19 states and large urban school districts, 2017. Morb Mortal Wkly Rep 68:67
Rider GN, McMorris BJ, Gower AL, Coleman E, Eisenberg ME (2018) Health and care utilization of transgender and gender nonconforming youth: a population-based study. Pediatrics 141:e20171683
Steensma TD, McGuire JK, Kreukels BP, Beekman AJ, Cohen-Kettenis PT (2013) Factors associated with desistence and persistence of childhood gender dysphoria: a quantitative follow-up study. J Am Acad Child Adolesc Psychiatry 52:582–590
Steensma TD, Biemond R, de Boer F, Cohen-Kettenis PT (2011) Desisting and persisting gender dysphoria after childhood: a qualitative followup study. Clin Child Psychol Psychiatry 16:499–516
Witcomb GL, Claes L, Bouman WP, Nixon E, Motmans J, Arcelus J (2019) Experiences and psychological wellbeing outcomes associated with bullying in treatment-seeking transgender and gender-diverse youth. LGBT Health 6:2016–2229
Bockting W (2014) The impact of stigma on transgender identity development and mental health. In: Kreukels BPC, Steensma TD, de Vries ALC (eds) Focus on sexuality research. Gender dysphoria and disorders of sex development: progress in care and knowledge. Springer, New York, pp 319–330
Shiffman M, VanderLaan DP, Wood H, Hughes SK, Owen-Anderson A, Lumley MM et al (2016) Behavioral and emotional problems as a function of peer relationships in adolescents with gender dysphoria: a comparison with clinical and nonclinical controls. Psychol Sex Orientat Gend Divers 3:27
de Vries AL, Doreleijers TA, Steensma TD, Cohen-Kettenis PT (2011) Psychiatric comorbidity in gender dysphoric adolescents. J Child Psychol Psychiatry 52:1195–1202
Meyer IH (2003) Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull 129:674–697
Meyer IH (2019) Rejection sensitivity and minority stress: a challenge for clinicians and interventionists. Arch Sex Behav. https://doi.org/10.1007/s10508-019-01597-7
Williamson IR (2000) Internalized homophobia and health issues affecting lesbians and gay men. Health Educ Res 15:97–107
Di Giacomo E, Krausz M, Colmegna F, Aspesi F, Clerici M (2018) Estimating the risk of attempted suicide among sexual minority youths: a systematic review and meta-analysis. JAMA Pediatr 172:1145–1152
Clark TC, Lucassen MF, Bullen P, Denny SJ, Fleming TM, Robinson EM et al (2014) The health and well-being of transgender high school students: results from the New Zealand adolescent health survey (Youth'12). J Adolesc Health 55:93–99
Marshall E, Claes L, Bouman WP, Witcomb GL, Arcelus J (2016) Non-suicidal self-injury and suicidality in trans people: a systematic review of the literature. Int Rev Psychiatry 28:58–69
Mann G, Taylor A, Wren B, de Graaf NM (2019) Review of the literature on self-injurious thoughts and behaviours in gender-diverse children and young people in the United Kingdom. J Child Psychol Psychiatry 24:304–321
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151:264–269
Munn Z, Moola S, Riitano D, Lisy K (2014) The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int J Health Policy Manag 3:123
Righy C, Rosa RG, da Silva RTA, Kochhann R, Migliavaca CB, Robinson CC et al (2019) Prevalence of post-traumatic stress disorder symptoms in adult critical care survivors: a systematic review and meta-analysis. Crit Care 23:213
Higgins JP, Green S (2011) Cochrane handbook for systematic reviews of interventions. Wiley, Hoboken
Aitken M, VanderLaan DP, Wasserman L, Stojanovski S, Zucker KJ (2016) Self-harm and suicidality in children referred for gender dysphoria. J Am Acad Child Adolesc Psychiatry 55:513–520
Terada S, Matsumoto Y, Sato T, Okabe N, Kishimoto Y, Uchitomi Y (2011) Suicidal ideation among patients with gender identity disorder. Psychiatry Res 190:159–162
Becerra-Culqui TA, Liu Y, Nash R, Cromwell L, Flanders WD, Getahun D et al (2018) Mental health of transgender and gender nonconforming youth compared with their peers. Pediatrics 141:e20173845
Grossman AH, D'Augelli AR (2007) Transgender youth and life-threatening behaviors. Suicide Life Threat Behav 37:527–537
Thorne N, Witcomb GL, Nieder T, Nixon E, Yip A, Arcelus J (2019) A comparison of mental health symptomatology and levels of social support in young treatment seeking transgender individuals who identify as binary and non-binary. Int J Transgend 20:241–250
Arcelus J, Claes L, Witcomb GL, Marshall E, Bouman WP (2016) Risk factors for non-suicidal self-injury among trans youth. J Sex Med 13:402–412
Nahata L, Quinn GP, Caltabellotta NM, Tishelman AC (2017) Mental health concerns and insurance denials among transgender adolescents. LGBT Health 4:188–193
Skagerberg E, Parkinson R, Carmichael P (2013) Self-harming thoughts and behaviors in a group of children and adolescents with gender dysphoria. Int J Transgend 14:86–92
Spack NP, Edwards-Leeper L, Feldman HA, Leibowitz S, Mandel F, Diamond DA et al (2012) Children and adolescents with gender identity disorder referred to a pediatric medical center. Pediatrics 129:418–425
Holt V, Skagerberg E, Dunsford M (2016) Young people with features of gender dysphoria: demographics and associated difficulties. Clin Child Psychol 21:108–118
Achenbach TM, Edelbrock CS (1983) Manual for the child behavior checklist and revised child behavior profile. University Vermont/Dept Psychiatry, Burlington
Reynolds WM (1987) Suicidal ideation questionnaire (SIQ). Psychological Assessment Resources, Odessa
Claes L, Vandereycken W (2007) The self-injury questionnaire—treatment related (SIQ-TR): construction, reliability, and validity in a sample of female eating disorder patients. In: Goldfarb PM (ed) Psychological Tests and testing research trends. Nova Science Publishers, New York, pp 111–139
Evans R, White J, Turley R, Slater T, Morgan H, Strange H et al (2017) Comparison of suicidal ideation, suicide attempt and suicide in children and young people in care and non-care populations: Systematic review and meta-analysis of prevalence. Child Youth Serv Rev 82:122–129
Muehlenkamp JJ, Claes L, Havertape L, Plener PL (2012) International prevalence of adolescent non-suicidal self-injury and deliberate self-harm. Child Adolesc Ment Health 6:10
Fedewa AL, Ahn S (2011) The effects of bullying and peer victimization on sexual-minority and heterosexual youths: a quantitative meta-analysis of the literature. J GLBT Fam Stud 7:398–418
Goldblum P, Testa RJ, Pflum S, Hendricks ML, Bradford J, Bongar B (2012) The relationship between gender-based victimization and suicide attempts in transgender people. Prof Psychol Res Pract 43:468
Coolhart D, Shipman DL (2017) Working toward family attunement: Family therapy with transgender and gender-nonconforming children and adolescents. Psychiatr Clin N Am 40:113–125
Aparicio-García M, Díaz-Ramiro E, Rubio-Valdehita S, López-Núñez M, García-Nieto I (2018) Health and well-being of cisgender, transgender and non-binary young people. Int J Environ Res Public Health 15:2133
Day JK, Perez-Brumer A, Russell ST (2018) Safe schools? Transgender youth’s school experiences and perceptions of school climate. J Youth Adolesc 47:1731–1742
Mann JJ, Currier D (2007) A review of prospective studies of biologic predictors of suicidal behavior in mood disorders. Arch Suicide Res 11:3–16
McGowan PO, Sasaki A, D'Alessio AC, Dymov S, Labonté B, Szyf M et al (2009) Epigenetic regulation of the glucocorticoid receptor in human brain associates with childhood abuse. Nat Neurosci 12:342
Hatzenbuehler ML, Pachankis JE (2016) Stigma and minority stress as social determinants of health among lesbian, gay, bisexual, and transgender youth: research evidence and clinical implications. Pediatr Clin N Am 63:985–997
Turecki G, Brent DA (2016) Suicide and suicidal behaviour. Lancet 387:1227–1239
Patros CH, Alderson RM, Kasper LJ, Tarle SJ, Lea SE, Hudec KL (2016) Choice-impulsivity in children and adolescents with attention-deficit/hyperactivity disorder (ADHD): a meta-analytic review. Clin Psychol Rev 43:162–174
Mole TB, Irvine MA, Worbe Y, Collins P, Mitchell SP, Bolton S et al (2015) Impulsivity in disorders of food and drug misuse. Psychol Med 45:771–782
Liu RT, Trout ZM, Hernandez EM, Cheek SM, Gerlus N (2017) A behavioral and cognitive neuroscience perspective on impulsivity, suicide, and non-suicidal self-injury: meta-analysis and recommendations for future research. Neurosci Biobehav Rev 83:440–450
Peterson CM, Matthews A, Copps-Smith E, Conard LA (2017) Suicidality, self-harm, and body dissatisfaction in transgender adolescents and emerging adults with gender dysphoria. Suicide Life Threat Behav 47:475–482
DiPlacido J (1998) Minority stress among lesbians, gay men, and bisexuals: A consequence of heterosexism, homophobia, and stigmatization. In: Herek GM (ed) Psychological perspectives on lesbian and gay issues Stigma and sexual orientation: understanding prejudice against lesbians, gay men, and bisexuals, vol 4. Sage Publications Inc, Thousand Oaks, pp 138–159
Ryan C, Huebner D, Diaz RM, Sanchez J (2009) Family rejection as a predictor of negative health outcomes in white and Latino lesbian, gay, and bisexual young adults. Pediatrics 123:346–352
Craig SL, Austin A (2016) The AFFIRM open pilot feasibility study: a brief affirmative cognitive behavioral coping skills group intervention for sexual and gender minority youth. Child Youth Serv Rev 64:136–144
Keo-Meier CE, Ehrensaft DE (2018) The gender affirmative model: An interdisciplinary approach to supporting transgender and gender expansive children. American Psychological Association, Washington
Craig SL, McInroy LB, Eaton AD, Iacono G, Leung VW, Austin A et al (2019) An Affirmative Coping skills intervention to improve the mental and sexual health of sexual and gender minority youth (project youth AFFIRM): protocol for an implementation study. JMIR Res Protoc 8:e13462
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
All authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Surace, T., Fusar-Poli, L., Vozza, L. et al. Lifetime prevalence of suicidal ideation and suicidal behaviors in gender non-conforming youths: a meta-analysis. Eur Child Adolesc Psychiatry 30, 1147–1161 (2021). https://doi.org/10.1007/s00787-020-01508-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-020-01508-5