Abstract
Prenatal maternal depression is associated with developmental disorders in offspring. However, the specific effects of the intensity of prenatal depressive symptoms on infant behavior remain poorly explored. The aim of this work is to explore the links between early neonatal behavior and maternal prenatal depressive symptoms, independently from maternal pre- and postnatal anxiety and early postnatal maternal depressive symptoms. Five hundred and ninety-eight women and their newborns from the MATQUID cohort were prospectively evaluated during the 8th month of pregnancy (T1) and at day 3 postpartum (T2). We analyzed the independent associations between neonates’ behavior (Neonatal Behavioral Assessment Scale—NBAS) at T2 and the intensity of maternal prenatal depressive symptoms (CES-D), taking into account confounding factors including depressive symptoms at T2 and anxiety (T1 and T2). The presence of a major depressive episode (MDE) based on MINI at T1 was also studied, independently. Our results show a significant negative correlation between prenatal CES-D scores and NBAS scores on “habituation” (p = 0.0001), “orientation” (p = 0.015), “motor system” (p < 0.0001), “autonomic stability” (p < 0.0001) dimensions, independently of other variables, including pre/postnatal anxiety and postnatal depressive symptoms. A prenatal MDE was independently associated with lower scores on the “orientation” dimension (p = 0.005). This study reports a specific effect of prenatal depressive symptoms on newborn’s behavior. These results highlight the crucial necessity for antenatal screening and adjusted treatments of maternal depressive symptoms and not only of MDE. Particular attention must be paid to infants of mothers presenting prenatal depressive symptoms to provide them with early developmental care when necessary.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The perinatal period is associated with somatic hormonal and psychological changes, with a high risk of developing psychiatric symptoms [1]. Prenatal maternal depression occurs in 8–12% of women in high-income countries [2] with a higher frequency of emotional, cognitive and behavioral disturbances in their children [3]. Several epidemiological studies reported that maternal depressive symptoms during pregnancy are associated with poorer child neurodevelopment [4,5,6,7]. A recent meta-analysis found maternal prenatal stress is associated with offspring socioemotional development, with the effect size for prenatal depression being more robust than for anxiety [8]. Very early intrauterine genetic, epigenetic as well as biochemical processes have been involved in the occurrence of these developmental disorders [3, 9,10,11]. However, postnatal environmental factors such as exposure to stressful situation and particularly maternal depression have also been associated with impaired neurodevelopment. Infant regulatory behavior problems already during the first month of life could predict neurobehavioral outcomes [12]. In addition, neonatal behavioral characteristics could have a significant impact on later occurrence of maternal postnatal depressive symptoms [13], emphasizing the bi-directionality of the effect of both maternal mental health and infant development. Indeed, infant regulatory behaviors in the first month of life partially mediated the effect of maternal depressive symptoms [12]. Thus, there is a particular interest in looking at the very early characteristics of the neonates to disentangle the part of infant vulnerability from later exposure to maternal depression.
Several studies evaluated the impact of maternal antenatal depression on neonatal behaviors reporting less optimal behaviors in exposed newborns [14,15,16,17,18,19,20,21,22,23,24]. The most replicated finding was for less optimal orientation in association with antenatal depression. Newborns exposed to maternal prenatal depression were more irritable and less consolable [25], responded less to facial expressions compared with newborns of non-depressed mothers [26] and showed more difficulty discriminating mother’s voice [27]. These babies had also more frequent sleep disorders [28] and a lower vagal tone [9].
One of the important limitations of all these studies is their small sample size (between 80 and 160 mothers). Moreover, only few studies have considered the presence of maternal depression [15, 18, 21] or maternal anxiety [18] at the time of the Neonatal Behavioral Assessment Scale (NBAS) as possible confounding factors. In addition, these studies evaluated prenatal depression in a categorical way, using different threshold score on different scales: CES-D (≥ 16: [11, 14]; > 16: [9, 10]), Beck Depression Inventory (BDI) (> 13: [19]; ≥ 13: [14]), Edinburgh Postnatal Depression Scale (EPDS) (> 10: [15]; ≥ 9: [22]), Montgomery–Asberg Depression Rating Scale (MADRS) (≥ 15: [18]). Five studies also associated a standardized interview [14, 18,19,20, 23].
Moreover, subclinical depression during pregnancy, defined as depression that exceeds empirically established symptom scale cutoff scores, but does not meet diagnostic criteria for a MDE, has been found to be associated with problems in women’s functioning equal in severity and breadth to those associated with MDE [28]. Therefore, not only major depression but also depressive symptoms might be associated with lower newborn neurobehavioral functioning compared to non-exposed newborns.
Regarding all these preceding results, we hypothesized that the level of prenatal depressive symptoms could be negatively correlated with NBAS scores. The aim of the present study is to explore the links between prenatal maternal depressive symptoms and very early neonatal behavioral characteristics, independently from pre- and postnatal maternal anxiety, and from postnatal maternal depressive symptoms.
Methods
Participants
The present study used the database of the MATQUID cohort study, previously described [29]. Briefly, women were included if they fulfilled the following criteria: (a) written informed consent to participate in the study; (b) fluency in French language; (c) living in the catchment area of the hospital (Bordeaux or close suburbs); (d) no personal history of psychotic illness; (e) no multiple pregnancy or in vitro fertilization for the current pregnancy; (f) less than 1 week of hospitalization due to complications of pregnancy; and (g) no planned cesarean section. Women were subsequently excluded after delivery in the case of premature birth (fewer than 37 weeks’ gestational age) or unplanned cesarean delivery.
On the 945 women fulfilling the inclusion criteria who were screened for participation in the survey, 598 were assessed during the third trimester of pregnancy (Time 1: T1) and 594 were assessed at day 3 (Time 2: T2): 2 women refused to continue the study, 1 had been lost sight of, and 1 child had died. In addition, neonatal behavior could not be evaluated for 69 infants (Fig. 1).
Ethical considerations
Written consent was obtained.
This study was approved by the ethical committee of the Bordeaux University (Comité Consultatif pour la Protection des Personnes dans les Recherches Biomédicales).
Baseline interview during pregnancy (T1)
This interview was carried out by research psychologists and took place at the maternity hospital during the third trimester. Sociodemographic information were collected: maternal age, parity (primiparous or multiparous), marital status, educational level (categorized as < 12 vs. ≥ 12 years), income in euros per month (categorized in < 1524 euros or ≥ 1524 euros), a history of self-reported depressive episode, psychotropic treatments during pregnancy, and smoking before pregnancy. The presence of maternal obstetrical complications evaluated on women self-report was also considered.
The marital relationship was explored through the French version of the “Dyadic Adjustment Scale”, a 32-item self-report questionnaire which scores can range from 0 to 151 [30, 31].
The mental state of the women at this time was evaluated by different interviews. Dimensional intensity of maternal depressive symptoms was assessed using the French version of the Center for Epidemiological Studies Depression-Scale (CES-D) [32, 33], a 20 self-report questionnaire on which scores can range from 0 to 60. The existence of a characterized MDE was evaluated using the MINI (Mini-International Neuropsychiatric Interview), a standardized diagnostic interview aiming at providing DSM-IV-R diagnosis (Diagnostic and Statistical Manual of Mental Disorders revised, 4th Edition) [28]. Finally, anxiety was assessed using a self-administered questionnaire the Bonis Anxiety Trait-State Inventory (BATE) [29] taking into account psychological factors, somatic factors, and specific fears, a 37-item self-report questionnaire, which scores from 0 to 148.
Interview at day 3 after birth (T2)
This interview was carried out by research psychologists which took place at the maternity hospital, 3 days after delivery.
Maternal mental state was assessed with CES-D [32, 33], MINI [34], and BATE [35].
Infant neonatal data were collected from the infant’s fills: sex, birth weight (low birth weight being < 2500 g), cephalic perimeter (small perimeter being < 33 cm), and Apgar index at 1st min (low index being < 7).
Psychologists were trained to rate the NBAS in a training session performed in a reference centre using a validated standardized procedure for the French NBAS version. Psychologists were not informed of the hypothesis tested in this study. Three days after delivery, infant neonatal behavior was assessed by psychologists trained to reliability, who were blind to maternal mental state, using the Neonatal Behavioral Assessment Scale (NBAS) [36].
This scale is designed to evaluate neonatal behavior until the age of 30 days. It is a standardized assessment tool in which neonatal behaviors are elicited in response to a range of stimuli yielding scores on the seven following clusters of behavioral and reflex items: (a) habituation (ability to respond and to inhibit the response to discontinuous stimuli while asleep), (b) orientation (includes the ability to attend to visual and auditory stimuli and the quality of overall alertness), (c) motor skills (motor performance and quality of movement and tone), (d) range of states (infant arousal and state lability), (e) regulation of states (infant’s ability to regulate his or her states in the face of increasing levels of stimulation), and (f) autonomic stability (signs of stress related to the homeostatic adjustments of central nervous system). Each dimension included several subcategories, which were each rated from 1 (not optimal competence) to 9 (maximum skill). The evaluation of a newborn with the NBAS requires specific conditions to be optimum because infant reactions are state related; for example, the infant must be sleepy at the beginning to test habituation. The number of participants for whom information was available was not the same for the six clusters of the test because some infants did not fulfill the criteria for evaluation of all dimensions at the time of the assessment (e.g., an infant who was not asleep at the beginning of the test was not evaluated on the habituation dimension, but was assessed on the other dimensions).
Statistical analysis
We first conducted a descriptive analysis of socio-demographic data, pregnancy-related and newborn characteristics. Quantitative variables were described by mean and standard deviation and categorical variables by percentages. Note that considering NBAS scores, the number of participants for whom information was available was not the same for the six clusters, as some infants did not fulfill the criteria for evaluation of all dimensions at the time of the assessment (e.g., an infant who was not asleep at the beginning of the test was not evaluated on the habituation dimension, but was assessed on the other dimensions).
Second, we tested the correlations between CES-D scores considered dimensionally and neonatal behavioral characteristics (NBAS) using Pearson correlation test. Multivariate analyzes were then performed, using a multiple linear regression taking into account the missing data with a Gibbs sample [37]. The correlations between the CES-D scores and the different categories of the NBAS score were adjusted on several variables considered as a priori potential confounders (maternal age, child gender, marital status, economic status, education, treatment during pregnancy, smoking before pregnancy, birth weight, cephalic perimeter, Apgar index at 1st min) (Model 1). We then adjusted also on depression and anxiety variables (Model 2): history of self-reported major depressive episode, CES-D score at T2, BATE score at T1 and T2 and dyadic adjustment scale score at T1. The validity of our multiple linear regression statistical model was evaluated by a graph in the statistics software, evaluating the normality of residuals.
Third, to provide data comparable to preceding results on the topic, the sample was divided into two categorical subgroups: MDE and no-MDE according to the MINI (T1). We then explored the association between the presence of prenatal MDE and neonate behavioral characteristics (NBAS) by multivariate analyses performed with the same plan of analyses reported previously.
All statistical analyses were performed using the R Version 2.14.1 software. Statistical tests were two-sided with a significance level set at 0.05.
Results
Characteristics of the sample
The final sample included 598 women at T1 and 594 mother–child dyads at T2. Women were aged 19–42 years [29.38 (4.36) years]. Sixty-four percent of them were primiparous. The majority of women lived with a partner (94.64%), had a good educational level (69.51% had a level higher than bachelor’s degree) and a medium to high economic level (> 1524 euros/month). The majority (82.11%) had no history of self-reported major depressive episode and did not take any psychotropic treatment during pregnancy (87.94%). At T1, mean BATE score was 18.22 (13.94), mean CESD score was 11.35 (7.63), and 30 (5.06%) women had a MDE following the MINI. There was no reported delivery complication for the wide majority of the children (86.31%). At T2, mean BATE score was 18.70 (13.52), mean CESD score was 10.7 (7.77), and 18 (3.26%) women had a MDE.
Regarding newborns, owing to the inclusion criteria, no child was premature. Five (0.91%) of them had a birth weight less than 2500 g, 33 (7.35%) had a cephalic perimeter below 33 cm and 6 (1.17%) had an Apgar index below 7 at 1st min (Table 1). NBAS scores are described in Table 1.
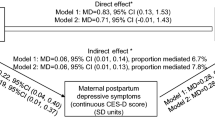
In bivariate analyses, prenatal maternal CES-D scores were significantly negatively correlated to habituation, orientation–interaction, motor system and autonomic stability scores (Table 2). Same results were found in Model 1. In the most adjusted model (Model 2), including past-MDE, CES-D scores at T2, BATE scores during pregnancy and T2, and dyadic adjustment scale scores during pregnancy, assessed quantitatively, prenatal maternal CES-D scores were significantly negatively correlated to habituation, orientation–interaction, motor system and autonomic stability scores (Fig. 2).
Correlations between CES-D scores at T1 and NBAS scores at T2. NBAS Neonatal Behavioral Assessment Scale, p value after adjustment for variables: parity, marital status, sex of the child, socio-educational level, income in euros per month, a history of self-reported depressive episode, treatment during pregnancy, smoking before pregnancy, physical maternal complications, birth weight, cephalic perimeter, Apgar index at 1st min, maternal age, BATE score at T1 and T2, dyadic adjustment score at T1, CES-D at T2
Note that, in the most adjusted model (Model 2), there was no statistically significant association between CES-D scores at T2 and NBAS after taking into account potential confounding variables (gender, child gender, marital status, economic status, education, history of self-reported major depressive episode, treatment during pregnancy, smoking before pregnancy, birth weight, cephalic perimeter, Apgar index at 1st min, maternal age, CES-D score at T1, BATE score at T1 and T2 and dyadic adjustment scale score at T1) (Table 3).
In the sample, 30 women (5.06%) had a diagnosis of prenatal MDE following the MINI. At T1, these depressed women had a significantly higher anxiety score (p < 0.001), lower quality of dyadic adjustment (p = 0.0001), lower income (p = 0.007), lower educational level (p < 0.05) and more frequent past history of self-reported depressive episode (p < 0.0001) than non-depressed women (Table 4).
In Model 2, a prenatal MDE was significantly associated with lower scores in the orientation–interaction dimension, independently of other variables, compared to no prenatal MDE. In addition, there was a tendency for an association between a prenatal MDE and lower scores in the “motor system” and “habituation” clusters (Table 5).
Discussion
Our study shows in a non-clinical sample a negative impact of the intensity of prenatal depressive symptoms on neonatal infant behavior, independently from neonatal depressive symptoms and from perinatal anxiety. Our results showed a significant negative correlation between maternal prenatal CES-D scores and habituation, orientation, motor system and autonomic stability infant scores, independently from CES-D scores at T2 as well as from pre- and postnatal anxiety. In addition, a prenatal maternal categorical MDE was significantly associated with a lower score in the orientation dimension and a tendency for lower scores in “habituation” and “motor system” clusters, independently of other variables, including a postnatal maternal MDE at T2 and pre- and/or postnatal anxiety.
Previous studies interested in the consequences of a prenatal maternal depressive episode on the NBAS scores showed worse performances for depressed mothers’ newborns in several clusters of infant behaviors: orientation [14, 16, 17, 20, 23, 24], habituation [16, 17, 23], motor system [16, 17, 23], range of states [17, 19], regulation of states [18, 21, 23] and autonomic stability [17, 19, 22, 23]. But the large majority of these studies suffer from a major limitation, that is most often anxiety and neonatal depression were not considered in the analyses. And they used mainly categorical diagnosis.
All the works on this topic, including our, highlights the impact of prenatal maternal depressive symptoms or depression on the abilities of the newborn in dimensions with a high relational potential (specially orientation). Indeed, the orientation cluster involves the visual and sound interactions, which are privileged means of communication for the dyad.
Our results suggest that infants of mothers with depressive symptoms during pregnancy may have early signs of exposure to these symptoms during intrauterine life, with less optimal newborn competencies at birth, especially orientation, possibly leading to an implementation of disturbed infant–mother and vice versa interactions.
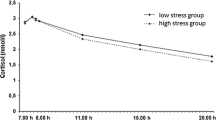
Slower scores on habituation, which refers to the ability to respond to and inhibit discrete stimuli while asleep, could be related to elevated arousal. Indeed, neonates of depressed mothers have higher fetal heart rate (FHR), lower vagal tone and elevated cortisol levels [9].
Lower scores on autonomic stability reflect signs of stress related to homeostatic adjustments of the central nervous system [36]. Lower scores could be linked to less autonomic nervous system (ANS) regulation and lower FHR variability, linked to lower neurobehavioral maturity during gestation in case of mother’s depression [22]. Lower scores on motor items sign lower motor performance and less quality of movement and tone.
Lower scores on orientation are linked to difficulty attending and orientating to stimuli and the quality of overall alertness. This could be related to the lesser attentiveness previously described in face-to-face interactions by infants of depressed mothers [38].
Among the seven established NBAS cluster scores, the most replicated finding was for less optimal orientation in association with antenatal depression [19]. In addition, this subscale has most often been found to predict later infant functioning [19]. Therefore, lower scores on orientation in infant exposed to prenatal maternal categorical MDE could predict impairment development.
One possible explanation is that stress causes increased transfer of maternal cortisol across the placenta to the fetus. Prenatal stress can reduce placental 11β-HSD2, the enzyme which metabolizes cortisol to inactive cortisone. This alters fetal programming [39]. Level of cortisol has been inversely correlated with infant cognitive development. Serotonin is another possible mediator of prenatal stress induced programming effects on offspring development. In addition, epigenetic changes in the child have been reported to start after prenatal stress [40]. Another explanation is the increase of uterine artery resistance with limited blood flow to the fetus. Higher placental NR3C1 mRNA was reported to partly mediate the association between maternal depressive symptoms during pregnancy and infant regulatory behaviors [41].
To our knowledge, our study is the first to evaluate the links between the intensity of maternal prenatal depressive symptoms and infant’s performance on the NBAS in a population of mothers not at risk for postnatal depression. Only Goodman et al. [19] previously searched for a correlation between the intensity of prenatal depressive symptoms and NBAS scores, but in a population at risk for prenatal depression due to a past history of depression and reported a significant negative correlation between the average score on the BDI (Beck Depression Inventory) and some NBAS dimensions scores (orientation, range of state and autonomic stability).
Our work highlights very early effects of the gradient of intensity of maternal prenatal depressive symptoms on the infant skills, and not only the effects of a MDE, in a population at low risk for perinatal depression. Previous studies showed that NBAS is an appropriate tool for detecting behaviors in healthy infants [42,43,44,45,46,47].
Those results have implications for clinicians working in perinatal care by showing the importance of detecting depressive symptoms, even subclinical. Therefore, this study highlights the crucial necessity for antenatal screening and adjusted psychotherapeutic and/or pharmacological treatments of maternal depressive symptoms and not only in case of MDE.
Limitation
The prevalence of a MDE at T1 (5.06%) was lower than reported in literature, estimated at 8.5% at the third trimester of pregnancy [2]. However, women included in our sample reported a good level of education and a medium to high socio-economic level, which are protective factors for depression [48].
A prenatal MDE was significantly statistically associated only with lower scores in the orientation–interaction dimension in the most adjusted model (Model 2), compared to no prenatal MDE. However, only 30 mothers were diagnosed with prenatal MDE which could limit the statistical power of the analysis.
Our work relies on an assessment of the maternal mental state at 8 month of pregnancy. Therefore, our results regarding the effect of prenatal depression on NBAS scores cannot be generalized to the entire pregnancy period. An absence of third-trimester depression should not be interpreted to no antenatal depression. However, being depressed in the third trimester was associated with infants having a decrease score in state of organization and irritability, when the experience in the two other trimesters was the same [19].
We did not have data on the consumption of tobacco during pregnancy which would have permitted to sort out which are the specific effects of tobacco exposure during pregnancy compared with the effect of antenatal depression on the behavior of the newborn. Indeed, recent data of the French EDEN Mother–Child cohort study highlight the interest of taking into account the role of potential mediating variables in the analysis of maternal mental health and child’s development [49, 50].
However, there is a likely bias in responses regarding consumption with under-reporting expected in the context of pregnancy, especially during the third trimester. Cigarette smoking before pregnancy, which can be a good proxy, was assessed and included in our analyses as potential confounding factor.
Unfortunately, prenatal alcohol and other toxics exposure which can affect infant neurodevelopment [51], were not assessed in this study. Indeed, for example, prenatal alcohol exposure was associated with increased infant emotional withdrawal and decreased activity at 6.5 months [52]. Guidelines recommended systematic screening of alcohol during pregnancy using validated questionnaires (AUDIT-C or T-ACE or TWEAK) [53]. However, as our sample is a non-clinical one, level of consumption of alcohol can be expected to be low.
We did not have details concerning psychotropic medications intake during pregnancy that could have consequences on the baby [54]. However, psychotropic medication intake was included in our analyses as potential confounding factor.
In addition, some of the confounders in the analyses (low birth weight, low cephalic perimeter, low Apgar index 1st min) could rather be potential mediators than confounders. Moreover, CES-D during pregnancy and at birth are highly correlated (Corr: 0.54, 95% CI 0.47–0.60; p < 2.2e−16).
There is a potential risk of multicollinearity. However, the confidence intervals of the CES-D are not wide (CES-D T1: 11.35 [10.70–12.00]; CES-D T2: 10.7 [10.02–11.38]) suggesting that, on a pure statistical point of view, since the confidence intervals of the estimates are rather narrows we do not face this problem here. In addition, bivariate analyses, Models 1 and 2 reported same associations.
The newborn behavior using the NBAS was only assessed at day 3. A second NBAS assessment would have increased the power of the study, even though the test retest validity of the NBAS is known to be poor. It would have been relevant to measure it again 2 weeks later, as recommended [36] and to have information on how the maternal symptoms and the NBAS scores would relate.
In addition, the fact that no association was reported with CESD after birth and NBAS could be explained by the potential relief of depressive symptoms just after the delivery.
Strengths
The MATQUID cohort, with 598 mothers and their infants included is, at our knowledge, the largest one focusing on prenatal depressive symptoms and NBAS scores. Premature birth which could have an impact on neonate’s behavioral characteristics was an exclusion criterion.
Statistical results relied on multivariate analyzes adjusting our results in other potentially explanatory variables. The validity of our multiple linear regression statistical models evaluated by a graph was correct (data not shown). No statistically significant correlation was reported between postnatal CES-D scores and NBAS at T2. In the same way, Pacheco and Figueiredo [21] found that depression at childbirth does not contribute to the effects of antenatal depression (during the third trimester) on neonate behavioral development [21]. In addition, depression during pregnancy but not at birth was found to explain the newborn’s preference for the mother’s face/voice [55].
The cohort included women not at high risk for perinatal MDE (high educational level and socio-economic status, few of them had past histories of depression). This specificity might have led to negative findings (i.e., lack of the association between exposure and outcome variables) by attenuating the strength of the association between MDE and neonatal behavioral characteristics. Thus, the consideration of this bias enhances the strengths of the results.
Finally, this study relies on the largest cohort evaluating the consequences of prenatal depressive symptoms on neonatal skills with different approach considering the dimensional intensity of depressive symptoms with CES-D scores and the diagnosis of MDE based on MINI.
Conclusions
Our study highlights the effects of the intensity of maternal prenatal depressive symptoms on newborns’ behavior, and not only the effects of a MDE.
Perinatal health professionals should be trained to screen factors of psychological vulnerability and maternal depressive symptoms, because the early management of perinatal depressive symptoms could possibly decrease the vulnerability of these newborns. A particular attention must be paid to early developmental characteristics of infants of mothers with prenatal depressive symptoms to provide them with early developmental care when necessary.
The multidisciplinary management starting in pre-partum should be continued in the postpartum period with vigilance paid to interaction within the dyad and clinical observation of the baby to support and optimize neonatal skills.
Further studies are needed to better characterize the specific mechanisms involved in the association between prenatal depressive symptoms and infant developmental consequences.
References
Howard LM, Molyneaux E, Dennis CL, Rochat T, Stein A, Milgrom J (2014) Non-psychotic mental disorders in the perinatal period. Lancet 384:1775–1788
Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner G, Brody S, Miller WC (2005) Perinatal depression: prevalence, screening accuracy, and screening outcomes. Evid Rep Technol Assess (Summ) 119:1–8
Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, Howard LM, Pariante CM (2014) Effects of perinatal mental disorders on the fetus and child. Lancet 384:1800–1819
Tuovinen S, Lahti-Pulkkinen M, Girchenko P, Lipsanen J, Lahti J, Heinonen K, Reynolds RM, Hämäläinen E, Kajantie E, Laivuori H, Pesonen AK, Villa PM, Räikkönen K (2018) Maternal depressive symptoms during and after pregnancy and child developmental milestones. Depress Anxiety 35:732–741
Ruisch IH, Buitelaar JK, Glennon JC, Hoekstra PJ, Dietrich A (2018) Pregnancy risk factors in relation to oppositional-defiant and conduct disorder symptoms in the Avon Longitudinal Study of Parents and Children. J Psychiatr Res 101:63–71
Velders FP, Dieleman G, Henrichs J, Jaddoe VW, Hofman A, Verhulst FC, Hudziak JJ, Tiemeier H (2011) Prenatal and postnatal psychological symptoms of parents and family functioning: the impact on child emotional and behavioural problems. Eur Child Adolesc Psychiatry 20(7):341–350
Robinson M, Oddy WH, Li J, Kendall GE, de Klerk NH, Silburn SR, Zubrick SR, Newnham JP, Stanley FJ, Mattes E (2008) Pre- and postnatal influences on preschool mental health: a large-scale cohort study. J Child Psychol Psychiatry 49:1118–1128
Madigan S, Oatley H, Racine N, Fearon RMP, Schumacher L, Akbari E, Cooke JE, Tarabulsy GMA (2018) A meta-analysis of maternal prenatal depression and anxiety on child socioemotional development. J Am Acad Child Adolesc Psychiatry 57:645–657
Field T (2011) Prenatal depression effects on early development: a review. Infant Behav Dev 34:1–14
Graignic-Philippe R, Dayan J, Chokron S, Jacquet AY, Tordjman S (2014) Effects of prenatal stress on fetal and child development: a critical literature review. Neurosci Biobehav Rev 43:137–162
Oberlander TF, Weinberg J, Papsdorf M, Grunau R, Misri S, Devlin AM (2008) Prenatal exposure to maternal depression, neonatal methylation of human glucocorticoid receptor gene (NR3C1) and infant cortisol stress responses. Epigenetics 3:97–106
Toffol E, Rantalainen V, Lahti-Pulkkinen M, Girchenko P, Lahti J, Tuovinen S, Lipsanen J, Villa PM, Laivuori H, Hämäläinen E, Kajantie E, Pesonen AK, Räikkönen K (2019) Infant regulatory behavior problems during first month of life and neurobehavioral outcomes in early childhood. Eur Child Adolesc Psychiatry 28:847. https://doi.org/10.1007/s00787-018-1243-8(epub ahead of print)
Sutter AL, Murray L, Glatigny-Dallay E, Verdoux H (2003) Newborn behavior and risk of postnatal depression in the mother. Infancy 4:589–602
Abrams SM, Field T, Scafidi F, Prodromidis M (1995) Newborns of depressed mothers. Infant Ment Health J 16:233–239
Diego MA, Field T, Hernandez-Reif M, Cullen C, Schanberg S, Kuhn C (2004) Prepartum, postpartum, and chronic depression effects on newborns. Psychiatry 67:63–80
Field T, Diego MA, Dieter J, Hernandez-Reif M, Schanberg S, Kuhn C, Yando R, Bendell D (2001) Depressed withdrawn and intrusive mothers’ effects on their fetuses and neonates. Infant Behav Dev 24:27–39
Field T, Diego MA, Dieter J, Hernandez-Reif M, Schanberg S, Kuhn C, Yando R, Bendell D (2004) Prenatal depression effects on the fetus and the newborn. Infant Behav Dev 27:216–229
Gerardin P, Wendland J, Bodeau N, Galin A, Bialobos S, Tordjman S, Mazet P, Darbois Y, Nizard J, Dommergues M, Cohen D (2011) Depression during pregnancy: is the developmental impact earlier in boys? A prospective case–control study. J Clin Psychiatry 72:378–387
Goodman SH, Rouse MH, Long Q, Ji S, Brand SR (2011) Deconstructing antenatal depression: what is it that matters for neonatal behavioral functioning? Infant Ment Health J 32:339–361
Lundy B, Jones N, Field T, Nearing G, Davalos M, Pietro P, Schanberg S, Kuhn C (1999) Prenatal depression effects on neonates. Infant Behav Dev 22:121–137
Pacheco A, Figueiredo B (2012) Mother's depression at childbirth does not contribute to the effects of antenatal depression on neonate's behavioral development. Infant Behav Dev 35:513–522
Figueiredo B, Pinto TM, Pacheco A, Field T (2017) Fetal heart rate variability mediates prenatal depression effects on neonatal neurobehavioral maturity. Biol Psychol 123:294–301
Osborne S, Biaggi A, Chua TE, Du Preez A, Hazelgrove K, Nikkheslat N, Previti G, Zunszain PA, Conroy S, Pariante CM (2018) Antenatal depression programs cortisol stress reactivity in offspring through increased maternal inflammation and cortisol in pregnancy: the Psychiatry Research and Motherhood—Depression (PRAM-D) Study. Psychoneuroendocrinology 98:211–221
Zhang H, Su Q, Yao D, Wang S, Dang S, Ding D, Zhu Z, Shao S, Li H (2017) Prolactin, a potential mediator of reduced social interactive behavior in newborn infants following maternal perinatal depressive symptoms. J Affect Disord 215:274–280
Lundy B, Field T, Pickens J (1996) Newborns of mothers with depressive symptoms are less expressive. Infant Behav Dev 19:419–424
Hernandez-Reif M, Field T, Diego M, Ruddock M (2006) Greater arousal and less attentiveness to face/voice stimuli by neonates of depressed mothers on the Brazelton Neonatal Behavioral Assessment Scale. Infant Behav Dev 29:594–598
Field T, Diego M, Hernandez-Reif M, Figueiredo B, Schanberg S, Kuhn C (2007) Sleep disturbances in depressed pregnant women and their newborns. Infant Behav Dev 30:127–133
Goodman SH, Tully EC (2009) Recurrence of depression during pregnancy: psychosocial and personal functioning correlates. Depress Anxiety 26:557–567
Verdoux H, Sutter AL, Glatigny-Dallay E, Minisini A (2002) Obstetrical complications and the development of postpartum depressive symptoms: a prospective survey of the MATQUID cohort. Acta Psychiatr Scand 106:212–219
Spanier GB (1976) Measuring dyadic adjustment: new scales for assessing the quality of marriage and similar dyads. J Marriage Fam 38:15–28
Baillargeon J, Dubois G, Marineau R (1986) Traduction française de l'Échelle d'ajustement dyadique. Can J Behav Sci 18:25–34
Radloff L (1977) The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1:385–401
Fuhrer R, Rouillon F (1989) La version française de l'échelle CES-D (Center for Epidemiologic Studies-Depression Scale). Description et traduction de l'échelle d'autoévaluation. Psychiatr Psychobiol 4:163–166
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC (1998) The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 59:22–33
De Bonis M (1973) Etude de l’anxiété par la méthode des questionnaires, problèmes généraux. Revue Psychol Appl 23:31–47
Brazelton TB, Nugent JK (1995) Neonatal behavioral assessment scale, 3rd edn. Mac Keith Press, London
Yang X, Belin TR, Boscardin WJ (2005) Imputation and variable selection in linear regression models with missing covariates. Biometrics 61:498–506
Cohn JF, Campbell SB, Matias R, Hopkins J (1990) Face-to-face interactions of postpartum depressed and nondepressed mother–infant pairs at 2 months. Dev Psychol 26:15–23
Barker DJP (2004) The developmental origins of adult disease. J Am Coll Nutr 23:588S–595S
Glover V (2014) Prenatal stress and its effects on the fetus and the child: possible underlying biological mechanisms. Perinatal programming of neurodevelopment. Springer Science + Business Media, New York
Räikkönen K, Pesonen AK, O'Reilly JR, Tuovinen S, Lahti M, Kajantie E, Villa P, Laivuori H, Hämäläinen E, Seck JR, Reynolds RM (2015) Maternal depressive symptoms during pregnancy, placental expression of genes regulating glucocorticoid and serotonin function and infant regulatory behaviors. Psychol Med 45:3217–3226
Sostek AM, Anders TF (1977) Relationships among the Brazelton Neonatal Scale, Bayley Infant Scales and early temperament. Child Dev 48:320–323
Tirosh E, Harel J, Abadi J, Berger A, Cohen A (1992) Relationship between neonatal behavior and subsequent temperament. Acta Paediatr 81:829–831
Vaughn B, Taraldson B, Crichton L, Egeland B (1980) Relationships between neonatal behavioral organization and infant behavior during the first year of life. Infant Behav Dev 3:47–66
Risholm-Mothander P (1989) Predictions of developmental patterns during infancy: assessments of children 0–1 years. Scand J Psychol 30:161–167
Canals J, Esparó G, Fernández-Ballart JD (2006) Neonatal behaviour characteristics and psychological problems at 6 years. Acta Paediatr 95:1412–1417
Canals J, Hernández-Martínez C, Esparó G, Fernández-Ballart J (2011) Neonatal Behavioral Assessment Scale as a predictor of cognitive development and IQ in full-term infants: a 6-year longitudinal study. Acta Paediatr 100:1331–1337
Leigh B, Milgrom J (2008) Risk factors for antenatal depression, postnatal depression and parenting stress. BMC Psychiatry 8:24
Peyre H, Albaret JM, Bernard JY, Hoertel N, Melchior M, Forhan A, Taine M, Heude B, De Agostini M, Galéra C, Ramus F, EDEN Mother-Child Cohort Study (2019) Developmental trajectories of motor skills during the preschool period. Eur Child Adolesc Psychiatry 78:89. https://doi.org/10.1007/s00787-019-01311-x(epub ahead of print)
Ibanez G, Bernard JY, Rondet C, Peyre H, Forhan A, Kaminski M, Saurel-Cubizolles MJ, EDEN Mother-Child Cohort Study Group (2015) Effects of antenatal maternal depression and anxiety on children's early cognitive development: a prospective cohort study. PLoS One 10:e0135849
Higley AM, Morin KH (2004) Behavioral responses of substance-exposed newborns: a retrospective study. Appl Nurs Res 17:32–40
Molteno CD, Jacobson JL, Carter RC, Dodge NC, Jacobson SW (2014) Infant emotional withdrawal: a precursor of affective and cognitive disturbance in fetal alcohol spectrum disorders. Alcohol Clin Exp Res 38:479–488
Thibaut F, Chagraoui A, Buckley L, Gressier F, Labad J, Lamy S, Potenza MN, Rondon M, Riecher-Rössler A, Soyka M, Yonkers K (2019) WFSBP and IAWMH guidelines for the treatment of alcohol use disorders in pregnant women. World J Biol Psychiatry 20:17–50
Oberlander TF, Warburton W, Misri S, Aghajanian J, Hertzman C (2006) Neonatal outcomes after prenatal exposure to selective serotonin reuptake inhibitor antidepressants and maternal depression using population-based linked health data. Arch Gen Psychiatry 63:898–906
Figueiredo B, Pacheco A, Costa R, Conde A, Teixeira C (2010) Mother's anxiety and depression during the third pregnancy trimester and neonate's mother versus stranger's face/voice visual preference. Early Hum Dev 86:479–485
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Regarding potential conflicts of interest, all of them were indirect: F. Gressier has given talks for Eisai, Lundbeck and Servier and received a Grant from Servier for a postdoctoral degree (2011–2012). B. Falissard has been a consultant, expert or has given talks for E. Lilly, BMS, Servier, Sanofi, GlaxoSmithKline, HRA, Roche, Boeringer Ingelheim, Bayer, Almirall, Allergan, Stallergene, Genzyme, Pierre Fabre, Astra Zeneca, Novartis, Janssen, Astellas, Biotronik, Daiichi-Sankyo, Gilead, MSD, and Lundbeck. A. Letranchant, E. Glatigny-Dallay and A. L. Sutter-Dallay report no financial relationships with commercial interests.
Rights and permissions
About this article
Cite this article
Gressier, F., Letranchant, A., Glatigny-Dallay, E. et al. Negative impact of maternal antenatal depressive symptoms on neonate’s behavioral characteristics. Eur Child Adolesc Psychiatry 29, 515–526 (2020). https://doi.org/10.1007/s00787-019-01367-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-019-01367-9