Abstract
Three independent complex segregation analyses found that the cause of Attention Deficit/Hyperactivity Disorder (ADHD) was the presence of major genes interacting with environmental influences. In order to identify potential environmental risk factors for ADHD in the Paisa community—a very well described, genetically isolated group—we randomly selected a sample of 486 children between 6 and 11 years of age. This group included 200 children with ADHD (149 males and 51 females) and 286 healthy controls (135 males and 151 females). The ADHD DSM-IV diagnosis was obtained using the DICA and BASC evaluation instruments, and the children’s mothers or grandmothers filled out a questionnaire on each child’s exposure to prenatal, neonatal, and early childhood risk factors. The data were analyzed using cross tabulation and stepwise logistic multiple-regression analyses. Cross tabulation associated ADHD with a variety of factors, including miscarriage symptoms, premature delivery symptoms, maternal respiratory viral infection, moderate to severe physical illness in the mother during gestation, prenatal cigarette and alcohol exposure, neonatal seizures, asphyxia or anoxia, severe neonatal illness, mild speech retardation, moderate brain injury, and febrile seizures (odds ratio ≥ 2, P < 0.05). Stepwise logistic multiple-regression analysis also uncovered a block of variables, including male gender, maternal illnesses, prenatal alcohol exposure, mild speech retardation, febrile seizures, and moderate brain injury (odds ratio ≥ 2.0, P < 0.05). Future studies on the risk of developing ADHD must include these environmental factors as covariates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Attention Deficit/Hyperactivity Disorder (ADHD) (OMIM 143465) is the most common behavioral disorder of childhood [15]. Individuals with ADHD are at heightened risk for poor educational attainment, lower income, underemployment, legal difficulties, and impaired social relationships [13, 30, 65].
Several environmental factors that might increase the risk of developing ADHD have been proposed. Of all of them, prenatal exposure to nicotine and alcohol was found to increase the incidence of ADHD, oppositional disorder (OD), and conduct disorder (CD) [11, 36, 37, 62, 63, 72]. Interestingly, ADHD has been reported as a risk factor for early alcohol and cigarette use and abuse [1, 35, 48].
Low birth weight (LBW) has also been evaluated as a potential risk factor for ADHD. A study found that ADHD children were three times more likely to have low birth weights, even after potential confounders such as exposure to alcohol and cigarettes were taken into account [46]. Season of birth is another postulated ADHD risk factor. Being born during September had an odds ratio (OR) of 5.4 for ADHD with learning disabilities and an OR of 4.5 for ADHD without psychiatric comorbidities. This suggests that a seasonal pattern of birth may exist for subtypes of ADHD, but it is also possible that this pattern is related to maternal respiratory infection (flu) during the first weeks of pregnancy [44], which is more common in winter.
ADHD has also been associated with medication exposure. There is clinical evidence that three-quarters of the children who receive Phenobarbital for febrile seizures or epilepsy develop hyperactivity symptoms, but it is not clear if this phenomenon is caused by the medication or the seizures [66].
It is clear that multiple environmental risk factors contribute significantly to the development of ADHD. Some of them may cause ADHD independently of genetic factors, but it is also possible that environmental influences interact with genetic vulnerabilities to exacerbate or complicate latent or already existing ADHD symptoms.
Over the past decade twin, adoption, family, and association studies have determined that genetic factors contribute to the etiology of ADHD. Phenotype sharing analyses in twins (monozygotic vs. dyzygotic), found that 91% of the variance in ADHD was due to genetic contributions, and only 8% to environmental contributions [2]. Adoption studies also confirmed that genetics, rather than shared environment, cause familial ADHD clustering [10, 20, 27]. In addition, family studies reported that a decrease in the kinship coefficient produced an increase in the relative risk of ADHD family recurrence when the ratio of the prevalence of ADHD in various kinds of relative pairs was compared to the prevalence of the disorder in the general population (λ statistic) [24].
In the same vein, two complex segregation analyses on families from ADHD probands demonstrated that the paradigm that best fit ADHD transmission variance was a sex-dependent Mendelian codominant model [21, 25, 39]. A third complex segregation analysis of nuclear families from a genetic isolate (the Paisa community in Colombia, South America) disclosed that dominant and codominant major gene models, and the non-multifactorial effects model, could not be rejected [38]. All the data from these three studies explain the predisposition to ADHD as the consequence of a dominant major gene (or genes interacting under an oligogenic frame), with a penetrance of ∼50%, differential sex liability, and small environmental contributions.
This paper will address the environmental influences that increased the risk of developing ADHD in a sample of children from the genetically isolated Paisa community in Colombia, South America. Previous studies have shown that ADHD in this community is associated with a strong genetic component [2, 4–6, 31], but we think that identifying environmental risk factor covariates will contribute significantly to our understanding the genetic and epidemiological causes of ADHD.
Methods
Participants
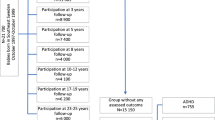
A cohort of 200 children with ADHD and 286 healthy controls between the ages of 6 and 11 with Full Scale Intelligence Quotients (FSIQs) over 80 were selected for the study. Both groups were evaluated with psychiatric, neurological, and psychological interviews and examinations plus several validated rating scales adapted for the Colombian population [49, 52–54, 56, 58, 61]. Sample size was calculated for a non-matched, epidemiological, case–control design.
The prevalence of ADHD in the Colombian population was estimated at 9.5–17%. The prevalence of the DSM-IV-based ADHD subtypes was: combined type, 5–10%; predominantly inattentive type, 4–6%; and hyperactive-impulsive type, 0.5–1% [49, 55, 56]. Risk factor exposure for the control population ranged from 5% to 10% with a 95% confidence interval (CI) and a significant odds ratio (OR) greater than or equal to 2. For these parameters, the sample size should be between 160 and 400 participants in each group.
ADHD cases
Children with ADHD between the ages of 6 and 11 who had been referred to the Neurosciences Group or the Neuropsychology and Conduct Disorder Group for assessment and treatment were randomly selected from the clinical databases of both organizations. Only children with complete evaluations performed during the 2 years prior to the study were chosen. These evaluations used a combined approach that had been approved and validated for clinical, epidemiological, and genetic ADHD research [49, 55, 56].
The cases met all the ADHD DSM IV criteria [3], and all the children were being treated with methylphenidate, to which they had responded well during at least the 3 months prior to the study. Children with depression, bipolar disorder, obsessive-compulsive disorder (OCD), or Tourette’s syndrome were excluded, as were children with an FSIQ below 70 or children whose ADHD had been diagnosed in the previous 6 months.
There were 495 children in the original sample who met these criteria, and 200 were randomly chosen to participate in the study. Their DSM IV ADHD subtypes were 62.5% combined (n = 125), 22.5% inattentive (n = 45), and 15% hyperactive-impulsive (n = 30). All the cases were sorted by gender, age, school level, and socioeconomic status (SES).
Criteria for cases:
-
1.
Psychiatrists and neurologists with extensive experience in ADHD diagnosis evaluated each child using the Diagnostic Interview for Children and Adolescents (DICA) [59] and the Behavior Assessment System for Children (BASC) [50, 51, 61] to ensure that they met all the DSM IV criteria for ADHD.
-
2.
The parents of children who were chosen for the study responded yes to at least six of nine questions about the presence of DSM IV inattention symptoms and/or answered yes to at least six of nine questions about the presence of DSM IV hyperactivity and impulsivity symptoms presented in a questionnaire.
-
3.
Children chosen for the study had a total score of 59 or more for inattention and hyperactivity-impulsivity on the ADHD checklist validated and standardized for Colombian children [49, 54].
-
4.
Children chosen for the study scored 80 or higher on the Wechsler Abbreviated Scale of Intelligence (WASI)(Spanish version) [73].
Control children
In the year 2000, the total estimated Colombian population was 38,000,000, of whom 1,980,000 lived in the metropolitan area of Medellín (95% in the city itself). The control children were selected from the 458 approved elementary schools registered in the State of Antioquia and the city of Medellín. The schools were sorted by geographic distribution and socioeconomic status (SES). Generally, in Colombia, public schools enroll only children of low (1 and 2) and low-middle (3) SES. Children of middle and high SES (4 and 5) attend private schools. This segregation factor facilitates an SES-based design where schools are defined as the unit of selection.
A random sample of 80 schools was contacted and the researchers met with each school’s principal and teachers to present the study. Seventy elementary schools agreed to participate. They gave the research team information on all their children between the ages of 6 and 11, which was placed in a database. Each child in grades 1 through 6 was assigned a random number. Only two to four children were selected for evaluation from each classroom so teachers would not have to fill out multiple rating scales, which might reduce evaluation accuracy.
An initial sample of 400 children was selected from the teacher-evaluated group and their families were contacted by phone. Three hundred of the children whose families agreed to let them participate were randomly chosen by a random numbers generator and were asked to take the DICA, BASC, and WASI. Only 14 of these children did not complete the entire evaluation, and they were excluded from the sample.
Criteria for controls:
-
1.
Control children did not meet the DSM IV criteria for ADHD on either the DICA or BASC.
-
2.
The parents of control children responded yes to no more than four out of nine questions about symptoms of inattention and/or to no more than four out of nine questions about symptoms of hyperactivity and impulsivity presented in an independent questionnaire.
-
3.
Control children had a total score of 55 or less for inattention and hyperactivity-impulsivity on the ADHD checklist validated and standardized for Colombian children.
-
4.
Control children had an FSIQ of 80 or more on the WASI.
Procedure
Cases
All psychiatric, medical, neurological, neuropsychological, and psychological records of the ADHD children were reviewed by neurologists and neuropsychologists. Parents provided information about the current clinical condition of their children and filled out the ADHD retrospective structured risk factor survey.
Controls
Parents of the selected students were contacted by phone and an appointment was arranged for signing the informed consent form, completing the ADHD retrospective structured risk factor survey, and filling out the rating scales. A neurological examination and a brief neuropsychological evaluation were performed on each child at the school. The children selected were in the upper half of their grade for academic achievement and the lower half for disciplinary history. Children with low academic achievement or disciplinary problems were excluded to guarantee that none of the control children had ADHD. If the information was confused or incomplete, whoever had initially provided the data (parents, teachers, or children) was re-contacted and asked to confirm or to complete the data. If this was not possible, the child was excluded from the database.
Instruments
The DSM IV criteria for ADHD [3], using the psychiatric Diagnostic Interview for Children and Adolescents—parent revised Spanish version (DICA-PR) [59, 60]
The DICA-PR is a fully structured interview that supplements a clinical examination. It covers all of the major child/adolescent categories in the DSM-IV. It can be used to screen for and diagnose a broad range of behavioral problems, such as ADHD, oppositional defiant disorder (ODD), conduct disorder (CD), generalized anxiety disorder, phobias, OCD, depression, bipolar disorder, and psychotic symptoms. The test’s reliability is estimated at 0.82–0.87 [59, 60].
DSM-IV-ADHD-symptoms questionnaire
This is a standardized questionnaire that evaluates the 18 DSM-IV ADHD criteria using yes/no queries. The child’s parents were asked to fill it out twice, once with regard to their child’s symptoms and once with regard to their own past behavior. This questionnaire has been used in clinical and epidemiological ADHD studies of the Antioquian population and has concurrent validity with the ADHD-DSM-IV-Checklist [48, 49, 54, 57].
Checklist for ADHD diagnosis
The checklist for ADHD diagnosis is an 18-item scale with questions that correspond directly to each of the nine DSM IV symptoms for inattention and the nine for hyperactivity-impulsivity. Each question is scored on a scale from 0 (never) to 3 (almost always). The maximum expected score for inattention or hyperactivity/impulsivity is 27. The scale can be used by both parents and teachers and has been standardized and validated with Colombian children [48, 49, 54, 57]. We used the checklist in a complementary fashion to assign participants to either the case or the control group. Children in the case group with total scores of 65 or over were excluded from the study.
Behavioral Assessment System for Children (BASC)
This multidimensional rating scale assesses internalizing and externalizing psychopathology in children and adolescents. The BASC includes questionnaires for parents and teachers and self-reports for children and adolescents [32, 33, 61]. It also has a standardized observation system and a structured interview for detecting medical and neurological disorders, plus a structured survey that retrospectively searches for potential environmental and other associated risk factors, including pregnancy problems, delivery difficulties, neonatal disorders, and neurological events that occurred between the ages of 1 and 5 [32, 33, 61]. The test has been standardized, evaluated using cluster analyses, and is used as a complementary diagnostic instrument for Colombian children and adolescents. A comparative cross-cultural study with Hispanic and African-American children has indicated that the factors do not vary cross-culturally [52, 53, 61].
Data analysis
All data were manually entered into a computer database. SPSS 10.0, EpiInfo 2000, and EPIDAT 2.1 were used to perform descriptive and inferential analyses. A standard χ2 test compared categorical variables between cases and controls. After discarding deviations from the normal distribution using the Kolmogorov–Smirnov test, a standard ANOVA was used to test significant differences between cases and controls for each continuous variable. Bivariate analyses were independently applied to the grouping binary variables and the binary responses (yes or no) to the environmental risk factor questionnaires. In addition, a multivariate logistic regression procedure introduced gender and school achievement as covariates, along with other variables that showed significant differences in the univariate model between cases and controls (OR > 2 with CI 95% >1). Child age was excluded because it was highly correlated (r 2 > 0.9) with school grade. This exclusion eliminated a bias toward enhancing partial relative-risk size effects as consequence of collinear errors.
Results
Characteristics of the sample
Variable counts for cases and controls are summarized in Table 1. Although gender distribution was even in the school databases, statistically significant differences were observed between genders in the results. This is a consequence of the design because ADHD is more prevalent in boys than in girls. There were no differences between cases and controls in intelligence or SES, but control children had a relatively small (0.33) but significantly higher school achievement than ADHD children, which strongly suggests overlapping between the two groups. Child age also showed a similar trend, with a small size effect of 0.26. Only those demographic variables that demonstrated significant differences between groups (gender and school achievement) were used as covariates in the multivariate analysis.
Risk factors
Environmental risk factor distributions for cases and controls are summarized in Table 2. In general, ADHD children had a higher incidence of all prenatal, neonatal, and early childhood risk factors; but after adjusting OR > 2 with adjusted CI 95% >1, only 11 of 35 of the analyzed risk factors remained. The highest risks were observed for prenatal alcohol exposure (adjusted OR = 14.1, CI 95%: 1.7–114), moderate brain injury (adjusted OR = 12.5, CI 95%: 1.5–102.3), and high prenatal cigarette exposure (adjusted OR = 8.9, CI 95%: 1.0–78.4).
The multivariate logistic regression model determined that high school achievement is a protective associated covariate (OR = 0.8, CI 95%: 0.7–0.9), while male gender was a susceptibility covariate (OR = 3.4, CI 95%: 2.2–5.2). In the multivariate logistic regression model, the most significant environmental risk factor was high prenatal alcohol exposure (OR = 11.7, CI 95%: 1.5–94.1). Four additional variables (child’s moderate brain injury before 5 years of age, maternal illness during pregnancy, child’s mild speech retardation, and febrile seizures) were included in the model (see Table 3).
Discussion
This research found that 11 of 35 prenatal, neonatal, and early-childhood health variables studied as risk factors for ADHD were significant (OR > 2, CI 95% >1). As reported in other studies [7, 18, 29, 36], high maternal alcohol consumption (defined in our study as drunkenness at least once during the first 2 months of pregnancy) and prenatal cigarette exposure [37] should be considered the highest risk factors for developing ADHD during childhood. Since the multivariate logistic model excluded prenatal cigarette exposure when gender was added, prenatal cigarette exposure appears to be a male gender-specific vulnerability. Maternal high alcohol consumption had the highest OR (11.7). One recent study with 7-year old children found a fairly significant association between symptoms as a quantitative trait, using a 0–8 point scale, but in this study, also, boys had a higher risk than girls [68] (Table 4).
Unfortunately, in the current study the structured risk factor survey obtained from the BASC neurological interview, did not allow us to obtain information about the presence of fetal alcohol syndrome (FAS), which is characterized by physical malformations, generalized learning disabilities, and psychological impairment with an increased risk of developing ADHD and CD. The BASC interview does not inquire about the neonatal period or the presence of FAS signs and symptoms; but because all subjects were required to have a normal FSIQ, we are assuming that children with generalized learning disabilities or serious intellectual deficits caused by their mother’s alcoholism were not included in the sample.
There are reports in the literature that cocaine and marijuana use during pregnancy are associated with child ADHD [47, 70, 71]. Our study found that drug abuse (frequent use during pregnancy of cocaine, marijuana, basic cocaine paste, and other strong drugs) was not a significant risk factor, and only 1.0% of the case mothers and 1.4% of the control mothers reported it. It may be a cultural trend in Colombia for young women to consume alcohol and smoke cigarettes rather than use strong drugs. It is also possible that the general Colombian population perceives alcohol and cigarettes as very soft drugs (or not drugs at all), and assumes they are not dangerous to fetal health. This assumption would explain the significant number of women that continued smoking and drinking during pregnancy.
Moderate and severe traumatic brain injuries have been reported as the cause of ADHD and other child and adolescent psychiatric disorders [14, 40–43]. In one study, approximately 48% of the children and adolescents who were followed after suffering a brain injury developed persistent ADHD symptoms [14]. A longitudinal study that used MRIs to measure the volume and spatial distribution of brain lesions in children and adolescents 3 months after they suffered a moderate or severe closed traumatic brain injury, found that 19.7% of the subjects developed severe ADHD symptoms [26, 28]. Lesions in the right putamen were more frequent in those patients who developed secondary ADHD [26, 28].
A set of multiple logistic regression models found that the odds ratio of developing ADHD symptoms was 3.6 in children with thalamic lesions and 3.2 in those with basal ganglia damage [26]. Even when pre-injury learning problems and ADHD were controlled for in the analysis, high impairments in executive function, verbal phonological fluency, and inhibitory control were observed in children after severe or moderate closed head injury [19]. These cognitive changes are similar to those reported in children with ADHD [16, 74], and these findings agree with the results of the current study, which found a significantly high association between a history of moderate brain injury (defined as closed head injury with loss of consciousness for more than 1 h and less than 24 h) and ADHD diagnosis.
There are two important caveats about this risk factor: (1) there is probably event-related memory bias about brain injury in the case parent group that does not exist in the control parent group, and (2) it is common for people to associate neurological and psychiatric disorders of any type with head injuries. Unfortunately, medical records and neuroimaging studies were not analyzed to confirm the data obtained from the retrospective risk factor survey.
Early-childhood febrile seizures have also been associated with ADHD symptoms in school age children [16, 19, 67], and this phenomenon could be caused by the convulsions themselves or the anti-epileptic medications the child received. Phenobarbital causes severe hyperactivity in 76% of treated children, and the corresponding figure for other anti-epileptic medications is 31% [19]. Although a prospective study [16] of 4,340 children who were followed from birth to age six did not find behavioral disorders or disadvantages in school performance in the 103 children in the sample who suffered febrile seizures at age three, our retrospective study found that febrile seizures were a risk factor for developing ADHD (OR = 2.0).
As expected, male gender appeared to be a demographic risk factor (OR = 3.4). Several other studies confirm that boys develop severe and complicated form of ADHD more often than girls [9, 17, 22, 45]. Girls develop the inattentive form of the disease more often than boys and appear to have more intellectual and learning impairment, while the combined type linked to oppositional and conduct disorders affected boys mostly [3, 9].
An association between both ADHD and CD with low SES, social adversity, low parent income, low parent school achievement, poor familial structure, parent drug abuse, and familial psychopathology has been extensively reported [64]. These studies involved populations with low school performance, low FSIQ, and generalized learning disabilities. Our study did not link ADHD with SES differences, and these findings were similar to those obtained by several prevalence studies, independently developed on the same isolated population, which found that low, middle, and high SES were not linked to the incidence of ADHD [55, 56]. One study of extended families that had several members who suffered from ADHD, ODD, and CD also found no significant SES differences between affected and unaffected family members [48].
In the same vein, one study of male offenders and CD adolescents in the Antioquian population, matched by age and SES with healthy non-offenders and non-CD adolescents, discovered a high association between ADHD symptoms, very low education level, low FSIQ, and familial adversity [53]. We interpret these findings to mean that risk factors related to SES and social adversity change when samples are recruited from ADHD or CD pools or if the members of the sample are only children, adolescents, or both. This is true whether or not the sample is controlled for FSIQ.
A complex matter that must be addressed in future studies is the fact that, in this population, a multigenerational linkage analysis of behavioral phenotypes in extended families found that ADHD is associated with disruptive behaviors, which was evidenced by highly significant pair-wise linkages among ADHD and ODD (LOD = 14.19), ADHD and CD (LOD = 5.34), ODD and CD (LOD = 6.68), and CD and alcohol abuse/dependence (LOD = 3.98) [6]. The highly significant LOD scores and the presence of linkage homogeneity through all the sets of families suggest the pleiotropic expression of specific vulnerability genes. The results of this study support the hypothesis that major genes underlie a broad behavioral phenotype in these families that can manifest as a range of symptoms, including ADHD, disruptive behaviors (ODD and CD), and alcohol abuse or dependence. In other words, different behavioral phenotypes comprise a nosological entity and the concept of comorbidity is inadequate [34]. In this context, we strongly suspect that the partial ADHD variance associated with alcohol and nicotine consumption might be the result of genetic cosegregation between these phenotypes and ADHD.
Although, a twin-based study found that maternal smoking was still a risk factor for ADHD development, even after controlling for genetic influences [68, 69], we think that recruiting large family samples and systematically examining them for environmental influences would uncover independent genetic and environmental risk factors for ADHD.
In summary, our data define environmental factors for ADHD in the genetically isolated Paisa community of Antioquia, Colombia, which has a high incidence of ADHD. These data are similar to those reported for multiple studies in developed countries. Our general findings support the theory of ADHD as a clinical and epidemiological problem caused by environmental factors interacting with genetic vulnerabilities [2, 8, 12, 23, 39]. Future investigations on the risk of developing ADHD should include the environmental factors we found to be significantly linked to ADHD as covariates that interact with susceptibility loci.
Limitations
Our results should be accepted with caution because:
-
1.
Our samples came from very healthy school children with a fairly pure type of ADHD.
-
2.
Since the ADHD risk factor survey is part of the BASC general neurological interview and does not evaluate behavior problems, it will probably not produce clinically significant associations.
-
3.
The retrospective approach could have missed some important clinical information.
-
4.
The sample sizes only allowed the detection of the most common risk factors.
-
5.
Size effects could only be calculated for some demographic quantitative variables and not for risk factors, which were considered binary variables.
-
6.
Comorbidities and the way they interact with ADHD and ADHD risk factors were not taken into account.
-
7.
Detected risk factors could be overestimated because control children could belong to a supernormal healthy group.
References
Abrantes AM, Strong DR, Ramsey SE, Lewinsohn PM, Brown RA (2005) Substance use disorder characteristics and externalizing problems among inpatient adolescent smokers. J Psychoactive Drugs 37:391–399
Acosta MT, Arcos-Burgos M, Muenke M (2004) Attention deficit/hyperactivity disorder (ADHD): complex phenotype, simple genotype? Genet Med 6:1–15
American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders. American Psychiatric Association, Washington, DC
Arcos-Burgos M, et al. (2002) Attention-deficit/hyperactivity disorder (ADHD): feasibility of linkage analysis in a genetic isolate using extended and multigenerational pedigrees. Clin Genet 61:335–343
Arcos-Burgos M, et al. (2004) Pedigree disequilibrium test (PDT) replicates association and linkage between DRD4 and ADHD in multigenerational and extended pedigrees from a genetic isolate. Mol Psychiatry 9:252–259
Arcos-Burgos M, et al. (2004) Attention-deficit/hyperactivity disorder in a population isolate: linkage to loci at 4q13.2, 5q33.3, 11q22, and 17p11. Am J Hum Genet 75:998–1014
Aronson M, Hagberg B, Gillberg C (1997) Attention deficits and autistic spectrum problems in children exposed to alcohol during gestation: a follow-up study. Dev Med Child Neurol 39:583–587
Asherson PJ, Curran S (2001) Approaches to gene mapping in complex disorders and their application in child psychiatry and psychology. Br J Psychiatry 179:122–128
Biederman J, et al. (2002) Influence of gender on attention deficit hyperactivity disorder in children referred to a psychiatric clinic. Am J Psychiatry 159:36–42
Biederman J (2005) Attention-deficit/hyperactivity disorder: a selective overview. Biol Psychiatry 57:1215–1220
Biederman J, Faraone SV, Monuteaux MC (2002) Differential effect of environmental adversity by gender: Rutter’s index of adversity in a group of boys and girls with and without ADHD. Am J Psychiatry 159:1556–1562
Biederman J, Faraone SV, Monuteaux MC (2002) Impact of exposure to parental attention-deficit hyperactivity disorder on clinical features and dysfunction in the offspring. Psychol Med 32:817–827
Biederman J, Newcorn J, Sprich S (1991) Comorbidity of attention deficit hyperactivity disorder with conduct, depressive, anxiety, and other disorders. Am J Psychiatry 148:564–577
Bloom DR, et al. (2001) Lifetime and novel psychiatric disorders after pediatric traumatic brain injury. J Am Acad Child Adolesc Psychiatry 40:572–579
Castellanos FX, Tannock R (2002) Neuroscience of attention-deficit/hyperactivity disorder: the search for endophenotypes. Nat Rev Neurosci 3:617–628
Chang YC, Guo NW, Huang CC, Wang ST, Tsai JJ (2000) Neurocognitive attention and behavior outcome of school-age children with a history of febrile convulsions: a population study. Epilepsia 41:412–420
Dalsgaard S, Mortensen PB, Frydenberg M, Thomsen PH (2002) Conduct problems, gender and adult psychiatric outcome of children with attention-deficit hyperactivity disorder. Br J Psychiatry 181:416–421
Dierker LC, Canino G, Merikangas KR (2006) Association between parental and individual psychiatric/substance use disorders and smoking stages among Puerto Rican adolescents. Drug Alcohol Depend 84:144–153
Domizio S, Verrotti A, Ramenghi LA, Sabatino G, Morgese G (1993) Anti-epileptic therapy and behaviour disturbances in children. Childs Nerv Syst 9:272–274
Eaves L, et al. (1993) Genes, personality, and psychopathology: a latent class analysis of liability to symptoms of attention-deficit hyperactivity disorder in twins. In: Plomin R, McClearn GE (eds) Nature, nurture, and psychology. American Psychological Association, Washington, DC, pp 285–303
Faraone SV, et al. (1992) Segregation analysis of attention deficit hyperactivity disorder. Psychiatr Genet 2:257–275
Faraone SV, et al. (2001) A family study of psychiatric comorbidity in girls and boys with attention-deficit/hyperactivity disorder. Biol Psychiatry 50:586–592
Faraone SV, Biederman J (2000) Nature, nurture, and attention deficit hyperactivity disorder. Dev Rev 20:568–581
Faraone SV, Biederman J, Monuteaux MC (2000) Toward guidelines for pedigree selection in genetic studies of attention deficit hyperactivity disorder. Genet Epidemiol 18:1–16
Faraone SV, Doyle AE (2000) Genetic influences on attention deficit hyperactivity disorder. Curr Psychiatry Rep 2:143–146
Gerring J, et al. (2000) Neuroimaging variables related to development of secondary attention deficit hyperactivity disorder after closed head injury in children and adolescents. Brain Inj 14:205–218
Gillis JJ, Gilger JW, Pennington BF, DeFries JC (1992) Attention deficit disorder in reading-disabled twins: evidence for a genetic etiology. J Abnorm Child Psychol 20:303–314
Herskovits EH, et al. (1999) Is the spatial distribution of brain lesions associated with closed-head injury predictive of subsequent development of attention-deficit/hyperactivity disorder? Analysis with brain-image database. Radiology 213:389–394
Hill SY, Lowers L, Locke-Wellman J, Shen SA (2000) Maternal smoking and drinking during pregnancy and the risk for child and adolescent psychiatric disorders. J Stud Alcohol 61:661–668
Hudziak JJ (2001) The role of phenotypes (diagnoses) in genetic studies of attention-deficit/hyperactivity disorder and related child psychopathology. Child Adolesc Psychiatr Clin N Am 10:279–297, viii
Jain M, et al. (2006) Attention-deficit/hyperactivity disorder and comorbid disruptive behavior disorders: evidence of pleiotropy and new susceptibility loci. Biol Psychiatry
Kamphaus RW, et al. (1999) A typology of parent rated child behavior for a national U.S. sample. J Child Psychol Psychiatry 40:607–616
Kamphaus RW, Huberty CJ, DiStefano C, Petoskey MD (1997) A typology of teacher-rated child behavior for a national U.S. sample. J Abnorm Child Psychol 25:453–463
Kaplan BJ, Dewey DM, Crawford SG, Wilson BN (2001) The term comorbidity is of questionable value in reference to developmental disorders: data and theory. J Learn Disabil 34:555–565
Knopik VS, et al. (2005) Contributions of parental alcoholism, prenatal substance exposure, and genetic transmission to child ADHD risk: a female twin study. Psychol Med 35:625–635
Knopik VS, et al. (2006) Maternal alcohol use disorder and offspring ADHD: disentangling genetic and environmental effects using a children-of-twins design. Psychol Med 36:1461–1471
Langley K, Rice F, van den Bree MB, Thapar A (2005) Maternal smoking during pregnancy as an environmental risk factor for attention deficit hyperactivity disorder behaviour. A review. Minerva Pediatr 57:359–371
Lopera F, et al. (1999) Genetic and environmental factors discrimination in attention deficit hyperactivity disorder. Rev Neurol 28:660–664
Maher BS, Marazita ML, Moss HB, Vanyukov MM (1999) Segregation analysis of attention deficit hyperactivity disorder. Am J Med Genet 88:71–78
Max JE, et al. (1998) Child and adolescent traumatic brain injury: correlates of disruptive behaviour disorders. Brain Inj 12:41–52
Max JE, et al. (1998) Attention-deficit hyperactivity symptomatology after traumatic brain injury: a prospective study. J Am Acad Child Adolesc Psychiatry 37:841–847
Max JE, et al. (2004) Attention deficit hyperactivity disorder in children and adolescents following traumatic brain injury. Dev Neuropsychol 25:159–177
Max JE, et al. (2005) Predictors of secondary attention-deficit/hyperactivity disorder in children and adolescents 6 to 24 months after traumatic brain injury. J Am Acad Child Adolesc Psychiatry 44:1041–1049
Mick E, Biederman J, Faraone SV (1996) Is season of birth a risk factor for attention-deficit hyperactivity disorder? J Am Acad Child Adolesc Psychiatry 35:1470–1476
Mick E, Biederman J, Faraone SV, Sayer J, Kleinman S (2002) Case-control study of attention-deficit hyperactivity disorder and maternal smoking, alcohol use, and drug use during pregnancy. J Am Acad Child Adolesc Psychiatry 41:378–385
Mick E, Biederman J, Prince J, Fischer MJ, Faraone SV (2002) Impact of low birth weight on attention-deficit hyperactivity disorder. J Dev Behav Pediatr 23:16–22
Noland JS, et al. (2005) Prenatal drug exposure and selective attention in preschoolers. Neurotoxicol Teratol 27:429–438
Palacio JD, et al. (2004) Attention-deficit/hyperactivity disorder and comorbidities in 18 Paisa Colombian multigenerational families. J Am Acad Child Adolesc Psychiatry 43:1506–1515
Pineda D, et al. (1999) Prevalence of attention-deficit/hyperactivity disorder symptoms in 4- to 17-year-old children in the general population. J Abnorm Child Psychol 27:455–462
Pineda DA, et al. (1999) Use of multidimensional scale for parents of children aged 6 to 11 for the diagnosis of attention deficit with hyperactivity. Rev Neurol 28:952–959
Pineda DA, et al. (1999) A system of multidimensional behavior assessment. A scale for parents of children from 6 to 11 years of age. Colombian version. Rev Neurol 28:672–681
Pineda DA, et al. (2005) Validation of two rating scales for attention-deficit hyperactivity disorder diagnosis in Colombian children. Pediatr Neurol 33:15–25
Pineda DA, et al. (2006) Screening for conduct disorder in an adolescent male sample from Colombia. Transcult Psychiatry 43:362–382
Pineda D, Ardila A, Rosselli M (1999) Neuropsychological and behavioral assessment of ADHD in seven- to twelve-year-old children: A discriminant analysis. J Learn Disabil 32:159–173
Pineda DA, Lopera F, Henao GC, Palacio JD, Castellanos FX (2001) Confirmation of the high prevalence of attention deficit disorder in a Colombian community. Rev Neurol 32:217–222
Pineda DA, Lopera F, Palacio JD, Ramirez D, Henao GC (2003) Prevalence estimations of attention-deficit/hyperactivity disorder: differential diagnoses and comorbidities in a Colombian sample. Int J Neurosci 113:49–71
Pineda DA, Merchan V (2003) Executive function in young Colombian adults. Int J Neurosci 113:397–410
Pineda DA, Rosselli M, Henao GC, Mejia SE (2000) Neurobehavioral assessment of attention deficit hyperactivity disorder in a Colombian sample. Appl Neuropsychol 7:40–46
Reich W (2000) Diagnostic interview for children and adolescents (DICA). J Am Acad Child Adolesc Psychiatry 39:59–66
Reich W (2000) More on the DICA [letter]. J Am Acad Child Adolesc Psychiatry 39:14–15
Reynolds CR, Kamphaus RW (1992) Behavior Assessment System for Children (BASC). American Guidance Service, Cicle Pines, MN
Rietveld MJ, Hudziak JJ, Bartels M, van Beijsterveldt CE, Boomsma DI (2003) Heritability of attention problems in children: I. cross-sectional results from a study of twins, age 3–12 years. Am J Med Genet 117B:102–113
Rowland AS, et al. (2001) Studying the epidemiology of attention-deficit hyperactivity disorder: screening method and pilot results. Can J Psychiatry 46:931–940
Rowland AS, Lesesne CA, Abramowitz AJ (2002) The epidemiology of attention-deficit/hyperactivity disorder (ADHD): a public health view. Ment Retard Dev Disabil Res Rev 8:162–170
Scahill L, Schwab-Stone M (2000) Epidemiology of ADHD in school-age children. Child Adolesc Psychiatr Clin N Am 9:541–555
Schubert R (2005) Attention deficit disorder and epilepsy. Pediatr Neurol 32:1–10
Shan’ko GG, Korol’ EA, Shal’kevich VB (1985) Neurologic disturbances and EEG characteristics in children who had hyperthermic convulsions in infancy. Neurosci Behav Physiol 15:48–53
Thapar A, et al. (2003) Maternal smoking during pregnancy and attention deficit hyperactivity disorder symptoms in offspring. Am J Psychiatry 160:1985–1989
Thapar A, Langley K, O’Donovan M, Owen M (2006) Refining the attention deficit hyperactivity disorder phenotype for molecular genetic studies. Mol Psychiatry 11:714–720
Verdoux H (2002) Long-term psychiatric and behavioural consequences of prenatal exposure to psychoactive drugs. Therapie 57:181–185
Verdoux H, Sutter AL (2002) Perinatal risk factors for schizophrenia: diagnostic specificity and relationships with maternal psychopathology. Am J Med Genet 114:898–905
Waldman ID, Rhee SH, Hay DA, Levy F (1999) Are genetic and environmental influences on ADHD the same throughout the range of symptoms as at the disordered extreme? Behav Genet 29(5):373
Wechsler D (1999) Wechsler Abbreviated Scale of Intelligence (WASI). The Psychological Corporation, San Antonio, TX
Zappitelli M, Pinto T, Grizenko N (2001) Pre-, peri-, and postnatal trauma in subjects with attention-deficit hyperactivity disorder. Can J Psychiatry 46:542–548
Acknowledgments
We would like to thank the Instituto Colombiano para el Desarrollo de la Ciencia y Tecnología (COLCIENCIAS) for funding the project: Factores de Riesgo para la Aparición del trastorno de Deficiencia de Atención en Niños de 6 A 11 Años del Valle de Aburrá [Risk factors for attention deficit diagnosis in 6- to 11-year-old children from Aburra Valley], code 1255-04-10169, grant #155-2000. The data presented in this paper were obtained from this project. We acknowledge assistant researchers Máryoris Zapata, Paula Montoya Angela Builes, Bibiana Velásquez, Jormaris Marínez, and Edith Oleiva Salazar.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pineda, D.A., Palacio, L.G., Puerta, I.C. et al. Environmental influences that affect attention deficit/hyperactivity disorder. Eur Child Adolesc Psychiatry 16, 337–346 (2007). https://doi.org/10.1007/s00787-007-0605-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-007-0605-4