Abstract
Introduction
Absorption of iodine through skin and an increased incidence of thyroid disorders due to iodophor exposure are reported. However, the risk of oral transmucosal absorption of povidone-iodine after intraoral preparation is not clear.
Objective
To investigate the possibility of oral transmucosal absorption of povidone-iodine after intraoral preparation and its effect on thyroxine level in blood.
Patients and methods
A randomized controlled study was carried out in the department of oral and maxillofacial surgery. Twenty- to 40-year-old healthy male adults planning to receive oral surgery under general anesthesia were enrolled. The study group received povidone-iodine irrigation of oral cavity for 3 min as intraoral preparation before operation. The control group received chlorhexidine gluconate irrigation of oral cavity for 3 min as intraoral preparation before operation. Iodine levels in blood and urine, and thyroxine levels in blood were tested and compared, before and after operation.
Result(s)
In total, 24 patients were included and analyzed finally. We found that after intraoral preparation with povidone-iodine, serum iodine level increased significantly to 2–3 times the pre-operation level in 15–30 min, and the urinary iodine level increased to 5 times the pre-operation level on the first day after operation. Iodine levels in blood and urine decreased significantly on the third day after operation but still significantly greater than the pre-operation levels. However, thyroxine levels were not altered accordingly.
Conclusion(s)
Oral transmucosal absorption of iodine is observed when povidone-iodine is used for intraoral preparation in healthy male adults, though the free thyroxine in blood is not affected accordingly.
Clinical relevance
Povidone-iodine is commonly used as an antiseptic in oral surgery and dental clinics. Based on our findings that iodine levels in blood and urine may elevate significantly after intraoral preparation with povidone-iodine prior to oral surgeries, care must be taken for individuals when excess iodine intakes can endanger the safety of the patient.
Registration information
Name of the trial registry: The Chinese Clinical Trial Registry (http://www.chictr.org.cn/). Registration number: ChiCTR2100042028
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Iodine which is essential for the production of thyroid hormones plays an important role in human metabolism. Iodine deficiency has a lot of adverse effects on growth and development [1], but high iodine intakes can be well tolerated by most healthy individuals [2]. However, in some people, excess iodine intakes can endanger the function of thyroid gland as well [2].
Besides of its important role in metabolism as a nutrient essential for thyroid hormone synthesis, iodine is also a highly effective topical antiseptic which has been used clinically for more than 100 years. Iodine has broad spectrum of antimicrobial activity against bacteria, mycobacteria, fungi, protozoa, and viruses [3], and is relatively inexpensive and easy to use in the meantime. Since iodophors were introduced in 1950s with the advantage of being much safer and less painful but just as effective as element iodine [3, 4], it has been widely used by surgeons and theatre staff as skin cleaner and antiseptic. Povidone-iodine is now the most widely used antiseptic for skin and intraoral preparation in oral and maxillofacial surgeries.
Though extensive evidence has been published to support the safety of povidone-iodine being used as an antiseptic agent in clinical practice, there is not without controversy considering the perceived issues with toxicity and systemic absorption. Substantial elevations of serum free iodide are found after intrapleural lavage with povidone-iodine [5], topically application of povidone-iodine in burn patients [6,7,8,9], vaginal mucosa preparation [10], and skin preparation in adults [11] and infants [12, 13]. An increased incidence of thyroid disorders in female medical personnel as a result of long-term iodine exposure has been reported according to a survey in a Chinese hospital [14].
To our knowledge, however, there is no study which has been carried out to investigate the risk of iodine absorption through oral mucosa, while intraoral preparation with povidone-iodine is so widely used in dental clinic and hospital worldwide. So, the aim of our study was to investigate the risk of oral transmucosal absorption of iodine after povidone-iodine is used for intraoral preparation prior to oral and maxillofacial surgery and its effect on thyroxine levels in blood.
Patients and methods
Population
The research protocol was approved by the institutional review board and was submitted to the Chinese Clinical Trial Registry (www.chictr.org.cn). Registration number ChiCTR2100042028 was recorded on January 14, 2021. From January 2021 through March 2021, we evaluated 60 patients who planned to undergo oral surgery under general anesthesia in our department. A total of 45 of 60 patients were eligible for the study. The inclusion criteria included as follows: (1) patients who were 20–40-year-old health males, (2) patients who were planned to receive jaw cyst curettages or surgical extractions of buried teeth under general anesthesia, (3) patients should have lived or worked in Chongqing for at least 2 years, and (4) patients who signed written informed consent before they were assigned. Exclusion criteria were as follows: (1) patients with a thyroid disorder history or iodine-containing drug using history within 6 months, (2) patients who had used drugs which have effects on the free thyroxine (FT4) levels in blood within 6 months, (3) patients with other medical conditions, (4) patients with known or suspected iodine sensitivity, (5) patients whose oral mucosa was unhealth or not intact, and (6) patients who were unable to comply with the diet instructions.
Design
Patients were first consecutively assigned to blocks according to their admission time. The randomization process was then carried out using the block randomization method with a block size of 4, and finally 24 patients were randomly assigned to study group (group A) or control group (group B) in a 1:1 ratio. Povidone-iodine and chlorhexidine gluconate irrigation of oral cavity for 3 min were applied as intraoral preparation for study group and control group, respectively. Patients were informed and signed consents were obtained from all participants before surgery. All subjects were kept on an iodine-restricted diet after admission until the fourth day after surgery.
Procedure
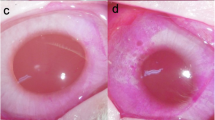
Perioral skin was prepared with 2% chlorhexidine gluconate (Lierkang, Shandong, China) for all the patients. 500 mg/L povidone-iodine (Lierkang, Shandong, China) and 0.12% chlorhexidine gluconate (Lierkang, Shandong, China) irrigation of oral cavity for 3 min were applied for intraoral preparation for study group and control group, respectively. The concentrations of povidone-iodine and chlorhexidine gluconate used in the study were determined according to the manufacturer’s recommendations. Then the oral cavity was dried with gauze sponge, and blood samples were collected. Venous access is established in all participants before they were sent to the theatre and antibiotic prophylaxis is given as a single intravenous dose 0.5 h before the operation. The operation time ranged from 2 to 2.5 h. Total amount of fluid administered during operation ranged from 500 to 1000 ml. A throat pack, made by suturing a surgical gauze roll together, leaving a long thread tail outside the mouth for emergency removal, was routinely used in all patients in order to prevent antiseptic agent, saliva, and blood to enter the oropharynx during the whole anesthesia period. When it appeared to be saturated with antiseptic agents (immediately after antisepsis), the throat pack was replaced by an unused one, and it would also be replaced several times if needed during the operation once the throat pack was completely wetted.
Outcome measures
The primary measures were the iodine levels in urine and blood and free thyroxine levels in blood, before and after intraoral preparation. Urine samples were collected from each subject on the day before the surgery, the first day after surgery, and the third day after surgery, respectively. Venous blood samples were collected from each subject on the day before the surgery, 15 and 30 min after the oral cavity was dried with gauze sponge, and on the third day after surgery, respectively. Iodine levels were tested in all urine and blood samples. FT4 levels were tested in blood samples collected before surgery and on the third day after surgery. Serum and urinary iodine levels were measured using arsenic-cerium catalytic spectrophotometry. All samples were test by an independent employee from department of clinical laboratory who was blinded to the patient assignment and interventions.
Statistical analysis
We assumed that an average of 0% iodine level increase would be achieved in the control group, and that the average iodine level in the study group would not be lower than that in the control group. To detect an absolute increase of 50% in the iodine levels for the study group, we needed at least 22 subjects (11 per group for two groups) for a power of 80% at a significance of 0.05. Results were analyzed by Wilcoxon signed-rank test. A p value less than 0.05 was considered statistically significant.
Results
Study population
From January 2021 through March 2021, we screened 60 patients for eligibility, and 45 patients were eligible for this study, of which 21 patients were not included due to various reasons. Finally, 24 male patients, aged from 21 to 35 years old with an average age of 28 years old and a median age of 28.5 years old, were enrolled and completed the study (Fig. 1).
Outcomes
The postoperative courses were uneventful for all subjects, and all patients were discharged from hospital to home on the fourth day after surgery. Serial changes of serum iodine (SI) and urinary iodine (UI) levels of each participant in groups A and B are shown in Figs. 2 and 3 respectively. Tables 1 and 2 represent the median iodine levels of SI and UI of each group at indicated time points, respectively.
As shown in Fig. 4a, the SI levels of participants after povidone-iodine preparation were significantly greater than that before preparation. The average SI level increased significantly to twofold 15 min after preparation and to nearly threefold 30 min after preparation. SI levels decreased significantly on the third day after surgery, but still greater than that before povidone-iodine preparation. However, SI levels of participants in group B decreased significantly 15 min and 30 min after intraoral preparation with chlorhexidine gluconate, which may be due to fluid administration started before entering the theatre. SI levels further decreased significantly on the third day after surgery in group B compared with the pre-surgery levels, which may because of the iodine-restricted diet.
Distribution of serum iodine (a) and urinary iodine (b) in experiment group and control group at indicated time point. The p value was calculated by the Wilcoxon signed-rank test and is displayed on the plot. Bef., before operation; 15 min/30 min aft., 15 min/30 min after intraoral preparation; 1st/3rd aft., the first/third day after operation
The median UI level on the first day after surgery in group A was found increased significantly to 5 times the pre-surgery level as shown in Fig. 4b and was found to decrease on the third day after surgery, which were still significantly higher than the pre-surgery level. However, UI levels in group B were found significantly decreased on the first day after surgery compared with the pre-surgery levels, and even greater decrease was observed on the third day, which may be the results of the iodine-restricted diet. Serum T4 levels were found not significantly altered in all subjects before and after surgery (Fig. 5).
Discussion
SI or UI levels were found substantially elevated in patients undergoing skin preparation with povidone-iodine in infants [12], neonates [15], and adults [11]. Similar results were found in vaginal mucosa preparation [10] and intrapleural lavage [5] using povidone-iodine. Povidone-iodine is now the most widely used antiseptic in the department of oral and maxillofacial surgery for skin and intraoral preparation. Considering the short time of application, the oral transmucosal absorption of povidone-iodine seems negligible. However, on the contrary, in this study, we found that, after intraoral preparation with povidone-iodine for 3 min, SI level increased significantly to 2–3-folds in 15–30 min, and the UI level increased significantly to 5 times the pre-operation level on the first day after operation. Considering the fact that oral transmucosal absorption of drugs is generally rapid due to the rich vascular supply to the oral mucosa and a lack of a stratum corneum epidermis [16], these findings should be actually expected rather than surprising.
Iodine is a nutrient most closely related with thyroid hormone synthesis. Thyroid disorders due to single absorption of iodine in infants after skin preparation with povidone-iodine [12] and in elderly patients after nonionic contrast radiography [17] are reported. Cases of hypothyroidism and hyperthyroidism caused by long-term improper use of povidone-iodine were also reported [18,19,20]. However, the effect of single absorption of iodine through oral mucosa on the function of thyroid gland is not clear. As almost all of the tetraiodothyronine (thyroxine, T4) is excreted directly by thyroid gland, while only a smaller amount of triiodothyronine (T3) is excreted by thyroid gland and more than 80% of the triiodothyronine (T3) present in target tissues is derived from T4 through the action of deiodinase enzymes, FT4 levels were mostly used to reflect the short-term function changes of thyroid gland [21, 22]. We found that single transmucosal absorption of iodine after intraoral preparation with povidone-iodine did not alter the blood FT4 levels in participants who were healthy male adults, which may be explained by that high iodine intakes can be well tolerated by most healthy individuals [2].
Based on the results of our study, it can be implied that povidone-iodine is a relatively safe antiseptic for intraoral preparation prior to oral and maxillofacial surgeries in most cases, or at least in healthy male adults. However, care must be taken for some individuals when excess iodine intakes can endanger the health of subjects as well, which may include patients with thyroid diseases, known or suspected iodine sensitivity, pregnant or breastfeeding women, neonates or infants, and patients about to receive diagnostic radioiodine therapy. And improper long-term use of povidone-iodine for gargling would not be a sensible recommendation according to our findings and previous reports.
However, one of the limitations of this study is that only male patients were included. As sex was found to have significant influence on FT4 and serum iodine levels [21, 23], similar conclusions may not be drawn for females. Further studies to investigate the risk of iodine absorption through oral mucosa and its effect on FT4 and SI/UI in females and infants are needed. A further limitation of the present study is that the sample size may be not large enough. In this study, we assumed that: (1) An average of 0% iodine levels increase would be achieved in the control group; (2) The average iodine level in study group would not be lower than that in the control group; (3) As high iodine intakes can be well tolerated by most healthy individuals, an increase of 50% in the iodine levels in the study group compared with the control group would be meaningful according to the experts’ opinion; and (4) We will accept a p < 0.05 as acceptable and a study with 80% power. Based on those assumes, the calculated sample size is 22 (11 subjects per group for two groups). However, since UI and SI values tend not to be normally distributed, a larger sample size would be more convincing. In addition, though a throat pack was used before antisepsis to prevent antiseptic agent to enter the larynx and trachea and was replaced by a bland one after it was saturated with antiseptic agents immediately after antisepsis, it was possible that some amount of iodine may be absorbed through oropharyngeal mucosa as the throat pack was placed anterior to or approximately at the level of the posterior edge of the soft palate for a patient in supine position. However, as a throat pack will be routinely used and placed at the back of oral cavity in almost all oral surgeries to prevent antiseptic agent, saliva, and blood to enter the upper respiratory tract and trachea of patient under general anesthesia, we do not think it would be meaningful to calculate the precise amount of iodine absorbed solely through the oral mucosa in the present and future studies of this kind, for the risk will not be reduced significantly by excluding the amount of iodine absorbed through oropharyngeal mucosa.
In spite of limitations discussed above, the current study had some merits of its own. To our best known, this is the first investigation of the risk of transoral absorption of iodine and its effect on FT4, which provides baseline data for future studies. Furthermore, our findings in this study would of reference value for a guidance for safer practices for clinical practitioners.
In summary, according to our study, oral transmucosal absorption of iodine is observed when povidone-iodine is used for intraoral preparation before oral and maxillofacial surgeries in male patients, though the free thyroxine levels are not altered accordingly. However, further studies are needed to investigate the risk of absorption of iodine and its long-term effect on the function of thyroid gland when povidone-iodine is used as skin and mucosa antiseptic prior to some major oral and maxillofacial surgeries for both male and female patients.
References
Zimmermann MB, Jooste PL, Pandav CS (2008) Iodine-deficiency disorders. Lancet 372:1251–1262
Farebrother J, Zimmermann MB, Andersson M (2019) Excess iodine intake: sources, assessment, and effects on thyroid function. Ann N Y Acad Sci 1446:44–65
Bigliardi PL, Alsagoff SAL, El-Kafrawi HY et al (2017) Povidone iodine in wound healing: a review of current concepts and practices. Int J Surg 44:260–268
Zinner DD, Jablon JM, Saslaw MS (1961) Bactericidal properties of povidone-iodine and its effectiveness as an oral antiseptic. Oral Surg Oral Med Oral Pathol 14:1377–1382
Findik G, Gezer S, Aydogdu K et al (2010) Effect of intrapleural povidone-iodine lavage on thyroid hormones in thoracic surgery. Thorac Cardiovasc Surg 58:225–228
Lavelle KJ, Doedens DJ, Kleit SA et al (1975) Iodine absorption in burn patients treated topically with povidone-iodine. Clin Pharmacol Ther 17:355–362
Rath T, Meissl G (1988) Induction of hyperthyroidism in burn patients treated topically with povidone-iodine. Burns Incl Therm Inj 14:320–322
Hunt JL, Sato R, Heck EL et al (1980) A critical evaluation of povidone-iodine absorption in thermally injured patients. J Trauma 20:127–129
Pietsch J, Meakins JL (1976) Complications of povidone-iodine absorption in topically treated burn patients. Lancet 1:280–282
Vorherr H, Vorherr UF, Mehta P et al (1980) Vaginal absorption of povidone-iodine. JAMA 244:2628–2629
Tomoda C, Kitano H, Uruno T et al (2005) Transcutaneous iodine absorption in adult patients with thyroid cancer disinfected with povidone-iodine at operation. Thyroid 15:600–603
Mitchell IM, Pollock JC, Jamieson MP et al (1991) Transcutaneous iodine absorption in infants undergoing cardiac operation. Ann Thorac Surg 52:1138–1140
Brown RS, Bloomfield S, Bednarek FJ et al (1997) Routine skin cleansing with povidone-iodine is not a common cause of transient neonatal hypothyroidism in North America: a prospective controlled study. Thyroid 7:395–400
Li CY, Guan HX, Li J et al (2003) Effects of iodophor on the thyroid glands of female medical workers. Zhonghua Yi Xue Za Zhi 83:647–649
Chabrolle JP, Rossier A (1978) Goitre and hypothyroidism in the newborn after cutaneous absorption of iodine. Arch Dis Child 53:495–498
Madhav NV, Shakya AK, Shakya P et al (2009) Orotransmucosal drug delivery systems: a review. J Control Release 140:2–11
Martin FI, Tress BW, Colman PG et al (1993) Iodine-induced hyperthyroidism due to nonionic contrast radiography in the elderly. Am J Med 95:78–82
Sato K, Ohmori T, Shiratori K et al (2007) Povidone iodine-induced overt hypothyroidism in a patient with prolonged habitual gargling: urinary excretion of iodine after gargling in normal subjects. Intern Med 46:391–395
Pagliaricci S, Lupattelli G, Mannarino E (1999) Hyperthyroidism due to the improper use of povidone-iodine. Ann Ital Med Int 14:124–126
Nobukuni K, Hayakawa N, Namba R et al (1997) The influence of long-term treatment with povidone-iodine on thyroid function. Dermatology 195 Suppl 2:69–72
Chaker L, Korevaar TIM, Medici M et al (2016) Thyroid function characteristics and determinants: the Rotterdam study. Thyroid 26:1195–1204
ooper DS, J Jonklaas (2019) Thyroid. In: L. Goldman and A. Schafer, editors (ed) Goldman-Cecil Medicine, 26th ed. Elsevier, Philadelphia
Fashena GJ (1938) A study of the blood iodine in childhood. J Clin Investig 17:179–188
Funding
This study was supported by the Chongqing Postdoctoral Science Foundation (Grant No. cstc2019jcyj-bshX0018 to LM Gou) and National Nature Science Foundation of China (Grant No. 31871464 to P Ji). The work was supported by the Department of Oral & Maxillofacial Surgery, Stomatological Hospital of Chongqing Medical University, China.
Author information
Authors and Affiliations
Contributions
LM Gou conceived the concept of the study, generated the random allocation sequence, and enrolled participants. XC Ren assigned participants to interventions. All authors contributed to the design of the research, data collection, and interpretation of data. LM Gou analyzed the data and drafted the manuscript. LM Gou and P Ji contributed equally to funding acquisition. All authors edited and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gou, L., Zhao, R., Ren, X. et al. Oral transmucosal absorption of iodine after intraoral preparation with povidone-iodine prior to oral surgeries: a randomized controlled study in 12 male patients. Clin Oral Invest 26, 705–711 (2022). https://doi.org/10.1007/s00784-021-04048-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-04048-7