Abstract
Objective
To assess whether lesion sterilization and tissue repair (LSTR) technique resulted in similar clinical and radiographic success outcomes as compared with pulpectomy in primary teeth.
Materials and methods
Randomized clinical trials comparing LSTR with pulpectomy by means of clinical and radiographic parameters were included. Risk of bias was assessed using Cochrane methodology and the certainty of evidence was determined by GRADE.
Results
Six articles were included. Conventional pulpectomy was favored with respect to radiographic success frequency in the systematic review. Four studies were included in meta-analyses. Based on the clinical results at 6 months (RR = 0.99, 95% CI, 0.94–1.04, p = 0.67; I2 = 0%), 12 months (RR = 0.97, 95% CI, 0.90–1.04, p = 0.34; I2 = 0%), and 18 months (RR = 0.89, 95% CI, 0.77–1.04, p = 0.14; I2 = 0%) and radiographic findings at 6 months (RR = 0.91, 95% CI, 0.78–1.06, p = 0.23; I2 = 9%), 12 months (RR = 0.87, 95% CI, 0.65–1.18, p = 0.38; I2 = 64%), and 18 months (RR = 0.84, 95% CI, 0.69–1.02, p = 0.08; I2 = 0%), there was no difference observed regarding success between the two treatments. The quality of evidence ranged from moderate to very low.
Conclusions
No difference between the LSTR and pulpectomy approaches could be confirmed by meta-analyses. The quality of evidence according to the GRADE scheme ranged from moderate to very low.
Clinical relevance
The present meta-analyses could not demonstrate the superiority of one treatment over the other.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The early loss of primary molars may lead to undesirable consequences in the developing dentition [1]. Pulpectomy has been the gold-standard treatment for addressing primary teeth with pulp necrosis or irreversible pulp inflammation and is based on the debridement and modeling of the root canals with manual or rotary instruments together with the use of antimicrobial irrigation solutions aimed at decontaminating the root canal system for posterior filling with resorbable materials [2]. However, the inherent characteristics of the root canal system in primary teeth make this procedure an endodontic challenge, especially in molars. The presence of lateral branches as well as accessory channels at the apex and furcation regions; the anomalous root canal anatomy; and, finally, the fact that the roots of the primary teeth are located close to the germ of the permanent successor and are physiologically programmed to exfoliate [1, 3] all contribute to increase the level of difficulty.
Given that root canal infection was a common problem in the primary dentition [4] in the 1990s, a new technique called lesion sterilization and tissue repair (LSTR) was proposed as an alternative biologic approach that sought to facilitate the disinfection of dentinal carious lesions, pulp, and periapical lesions in primary teeth [5,6,7] with the advantages of being simpler and faster [4, 8]. LSTR has been proposed as one option to potentially replace pulpectomy as it is simpler and quicker to perform and does not necessitate multiple visits be completed, even for teeth with periapical lesions [4]. LSTR is also known as noninstrumental endodontic treatment (NIET) and consists of the nonmechanical instrumentation of the root canals and placement of a paste made of a mixture of antibiotics at the entrance of the root canals [9].
Given the above, the present systematic review sought to answer whether there is adequate scientific evidence to favor the use of LSTR therapy in primary teeth as compared with conventional pulpectomy treatment.
Materials and methods
This systematic review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines [10] and the protocol was registered in the International Prospective Register of Systematic Reviews database under the number CRD42018107312.
Eligibility criteria
Based on the PICO strategy, randomized clinical trials (RCTs) involving primary teeth (P) submitted to noninstrumental endodontic treatment (I) in comparison with conventional pulpectomy (C) with respect to their clinical and radiographic success (O) were identified. Those studies that compared the clinical and radiographic outcomes of LSTR therapy and conventional pulpectomy in primary teeth with at least 6 months of clinical and radiographic follow-up were included. Review articles, case reports, editorials, letters to editors, in vitro or in situ studies, and clinical studies in which, in the LSTR group, the pulp tissue was extirpated or manipulated using files were excluded. Duplicated studies were also removed.
Information sources and search strategy
The PubMed, Web of Science, Scopus, Cochrane, BVS (LILACS and BBO), ClinicalTrials.gov databases, and the gray literature (Google Scholar and Trip Database) up to December 2019 without language or publication year restrictions were reviewed.
The search strategies, presented in Table 1, were adapted according to the syntax rules of each database, using the combination of MeSH terms, synonyms, and free terms. A librarian experienced in systematic searches (DMF) guided the process. Following article selection, an additional hand search was performed among the reference lists of each selected article in order to elucidate publications that might not have been found otherwise during the database investigations.
Selection of studies
Two of the authors (MLD and AVBP) conducted the search independently and selected the articles for inclusion. Consensus meetings with an expert in systematic reviews (LCM) were held whenever there were any disagreements between these two authors. Articles present in more than one electronic database were considered duplicated and, thus, only included once. The remaining titles and abstracts were evaluated, and all potentially eligible studies were read in full. Moreover, studies with insufficient data in the title and abstract were read in full to facilitate the making of a clear decision regarding their inclusion.
Data extraction
The same authors (MLD and AVBP) carried out the data extraction process independently. The data extracted from each included study included (1) authors, year of publication, and geographic location; (2) study design; (3) age range and mean age of the participants; (4) tooth type; (5) intervention group(s) and sample size; (6) follow-up time and evaluation criteria of the treatment; (7) treatment outcomes; and (8) main conclusions.
Risk of bias in individual studies
The methodological quality and risk of bias of each selected study were evaluated in accordance with the Cochrane Collaboration Tool by the same authors (MLD and AVBP), who conducted their evaluations independently and then compared the results. Disagreements were resolved during consensus meetings with a senior reviewer (LCM).
The following key domains were analyzed: selection bias (random sequence generation and allocation concealment), performance bias (blinding of participants and professionals), detection bias (blinding of outcomes assessment), attrition bias (incomplete outcome data), and reporting bias (selective reporting). Each key domain was classified as presenting either a “low,” “unclear,” or “high risk” of bias. When one key domain was judged as having “unclear” bias, up to five attempts to contact the authors of the study for additional information and then a posterior final risk of bias judgment was conducted. If one or more key domain was classified as showing “high” bias, the study was considered to have a high risk of bias.
Meta-analyses
Extracted data were inserted into the RevMan software (Review Manager v. 5.3; The Nordic Cochrane Centre, Copenhagen, Denmark) to be analyzed. Analyses were performed for the clinical and radiographic results achieved at 6, 12, and 18 months of follow-up. Success and failure frequencies were used to calculate the risk difference with a 95% confidence interval (CI). Heterogeneity was evaluated using the I2 index.
Certainty of the evidence
The quality of the evidence of estimates obtained from the meta-analyses was evaluated through the application of the Grading Recommendations, Assessments, Development, and Evaluations approach (GRADE) criteria using the software GRADEpro GDT (available at https://gradepro.org/; McMaster University, Hamilton, On, Canada and Evidence Prime, Inc., Hamilton, On, Canada). The quality of the evidence was categorized as recommended as either “high,” “moderate,” “low,” or “very low” [11]. The evaluations were carried out by two researchers independently (MLD and AVBP) and then compared.
Results
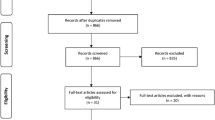
The PRISMA flow diagram presenting the search process and results is presented in Fig. 1. Initially, a total of 3984 studies were identified and 2811 records remained after the removal of duplicates using the reference manager EndNote. Another 2797 studies were removed after the retrieved studies were scanned based on their titles and abstracts because they did not meet the inclusion criteria. Fourteen full texts were read and eight were excluded due to not fulfilling the inclusion criteria. The reasons for the exclusions are described in Fig. 1. Finally, six studies were included in the systematic review, four were included in the 6 and 12 months clinical and radiographic follow-up meta-analyses, and from these, two studies were included in the 18 months meta-analyses.
Study characteristics
Table 2 presents the characteristics of the six studies selected for the systematic review. All six studies were RCTs. Three studies had been conducted in India [12,13,14], one was performed in Thailand [9], one was from Brazil [15], and one was from Argentina [16]. A total of 263 primary molars were treated (specifically, 119 in the control group and 144 in the intervention group). Four studies included teeth with necrotic pulps [9, 13, 14, 16] and two included teeth with both irreversible pulp inflammation and teeth with necrosis [12, 15]. The evaluation period ranged from 1 to 18 months.
Several distinct root canal filling pastes were used during conventional pulpectomy among the selected studies, including Vitapex® (Neo Dental International, Federal Way, WA, USA) [9, 13] and Maisto-Capurro [16], pastes based on iodoform and calcium hydroxide; Endoflas® (Sanlor Laboratories, Miami, FL, USA), an iodoform, calcium hydroxide, and zinc oxide powder added with propolis instead of eugenol [14]; zinc oxide and eugenol paste (ZOE) [12]; zinc oxide-ozonated oil-based paste [13]; and calcium hydroxide and zinc oxide paste [15]. For the LSTR technique, four studies [9, 12, 14, 16] used 3-Mix antibiotic paste composed of ciprofloxacin, metronidazole, and minocycline in different proportions and distinct vehicles, while Doneria et al. [13] used a mixture of ornidazole, ciprofloxacin, and cefaclor. CTZ, a combination of chloramphenicol, tetracycline, zinc oxide, and eugenol were also investigated in another study [15].
Regarding the final tooth restoration protocol, stainless steel crowns were used in five studies [9, 12,13,14, 16] and composite resin was used in one [15]. In the latter, the visible failures of coronary restoration were evaluated and classified as treatment failures. Among 53 teeth followed in this study, seven showed restoration failure with marginal leakage, including six in the intervention group and one in the control group.
In the respective control groups, the reported independent rate of clinical success at 6 months was 100% [9, 13, 14] and 89.4% [16], while at 12 months, it ranged from 88.8% [16] to 100% [13, 14] and at 18 months, from 88.8% [16] to 100% [13]. Meanwhile, the rate of radiographic success ranged from 40.0% [14] to 100% [13] at 6 months, from 56.0% [9] to 100% [13, 14] at 12 months, and from 83.3% [16] to 94.4% [13] at 18 months.
Among the intervention groups, the rate of clinical success ranged from 90.0% [16] to 100% [9] at 6 months, from 83.3% [16] to 96.0% [9] at 12 months, and from 82.3% [16] to 89.5% [13] at 18 months. Furthermore, the rate of radiographic success at 6 months ranged from 20.0% [14] to 84.0% [9], while at 12 months, it ranged from 60.0% [14] to 79.2% [13] and at 18 months from 76.4% [16] to 80.9% [13].
No difference between the success rates of the groups at any experimental time was disclosed in two studies [9, 16]. On the contrary, Agarwal et al. [12] disclosed statistical differences in overall success considering the clinical and radiographic performance at both 6 (p = 0.003) and 12 months (p = 0.016), with better outcomes achieved in the conventional pulpectomy group. Likewise, Divya et al. [14] and Doneria et al. [13] also observed better radiographic outcomes (p < 0.05) for the conventional pulpectomy treatment (Table 2).
Examples of reported treatment failures included gingival abscess [9, 13], new fistula [15], pathological mobility [13], increased radiolucency in the furcation area [13, 15], extensive external root resorption [15], internal radicular reabsorption [9, 13,14,15], and deviation in the eruption path of the successor [14]. Two studies [12, 16] did not report on the reasons for treatment failures.
Staining of the dental crown on 12 teeth after LSTR therapy and statistically significant lower survival rates for teeth treated with LSTR therapy (p = 0.024) were also reported [15].
Assessment of risk bias
Among the six included studies, Agarwal et al. [12] did not report enough information for random sequence generation and allocation concealment, thus being considered having an “unclear risk of bias”. Still considering selection bias, one study [16] was classified as of “high risk of bias” for inadequate random sequence generation and allocation concealment. Due to differences between the treatments and radiographic final images, participants, operators, and radiographic assessors could not be blinded. On the other hand, blinded clinical evaluations were feasible and reported by Agarwal et al. [12], Doneria et al. [13], and Nakornchai et al. [9], which were then classified as having a “low risk of bias” for the detection bias domain. The studies that did not perform blinded clinical evaluations [14,15,16] were classified as “high risk.” In one of them [14], only the statistical assessor was blinded. Doneria et al. [13] excluded overfilled teeth from the sample; the study was classified as having a “high risk” in the domain attrition bias. Similarly, Zacharczuk et al. [16] were considered “high risk” due to missing data was not properly reported.
In summary, one study was classified as showing an “unclear risk” of bias per the authors’ judgment even after contacting the authors via email, one was classified as having a “low risk,” and four were deemed to show a “high” degree of risk. Figure 2 presents the bias descriptions of the six selected studies.
Meta-analyses of the comparison of the clinical and radiographic performance
Six meta-analyses were performed; four analyses included four studies [9, 13, 14, 16] and two analyses included two studies [13, 16]. The quantitative grouping of these studies showed no differences between conventional treatment and LSTR. This conclusion was based on the clinical results at 6 (relative risk (RR) = 0.99, 95% CI, 0.94–1.04, p = 0.67; I2 = 0%), 12 (RR = 0.97, 95% CI, 0.90–1.04, p = 0.34; I2 = 0%), and 18 (RR = 0.89, 95% CI, 0.77–1.04, p = 0.14; I2 = 0%) months and radiographic findings at 6 (RR = 0.91, 95% CI, 0.78–1.06, p = 0.23; I2 = 9%), 12 (RR = 0.87, 95% CI, 0.65–1.18, p = 0.38; I2 = 64%), and 18 (RR = 0.84, 95% CI, 0.69–1.02, p = 0.08; I2 = 0%) months, respectively (Fig. 3).
Certainty of the evidence
The GRADE evidence summary is presented in Table 3. The quality of the evidence ranged from moderate to very low.
Discussion
The focused question of this systematic review was to address whether there is adequate scientific evidence to favor the use of LSTR therapy in primary teeth as compared with conventional pulpectomy treatment. Similar to conventional pulpectomy, distinct protocols have been proposed for the LSTR technique [9, 12,13,14,15,16,17,18]. In this sense, clinical diversity regarding the intervention protocols between the included studies was expected. However, such diversity was not observed considering the criteria applied for participants and outcomes, which were similar between the studies. Interestingly, distinct methodologies based on sound rationales either for the conventional or for the LSTR therapies and followed strictly or carried out properly result in elevated clinical and radiographical frequencies of success, as observed in the primary studies included as well as in the meta-analyses results [9, 12,13,14,15,16,17,18]. In addition, the heterogeneity between the studies was considered on the GRADE quality of evidence evaluation [11], which showed to range from moderate to very low. Therefore, these results suggest that although the differences could possibly affect the success of pulp treatment, the comparison between the included studies was not impaired.
In the LSTR technique, with respect to radicular pulp, some studies used files only to remove pulp tissue [17, 18]. Previous authors labeled this treatment as LSTR or NIET, given that the mechanical instrumentation of the root canal was not performed. Prabharkar et al. [19] demonstrated a statistically significant difference when comparing the application of nonmechanical instrumentation and mixed antibiotic paste in primary teeth with and without root pulp extirpation, favoring the group in whom radicular pulp tissue was extirpated. Our study did not consider works in which antibiotic paste was used when the radicular pulp was mechanically manipulated. As such, these studies were excluded from the systematic review, since we believe there existed differences between the procedures that may influence the outcome.
Considering the conventional treatment [20, 21], there was no consensus about the techniques and root canal filling materials. Zinc oxide and eugenol, iodoform-based paste (KRI), nonsetting calcium hydroxide paste, or a combination of iodoform paste and calcium hydroxide (e.g., Vitapex®, Endoflas®) were all employed [2, 22]. However, the clinical and radiographic performance evaluation criteria were usually similar between the studies. Specifically, the absence of pain, fistula, and abnormal mobility, and the absence of pain in percussion exam were used by Agarwal et al. [12] and Zacharczuk et al. [16], while visible restoration failure rating was employed by Daher et al. [15]. Any clinical signs and symptoms should resolve within a few weeks [2]. Meanwhile, radiographic signs should resolve within 6 months [2], as evidenced by bone deposition in the radiolucent pretreatment areas. Thus, the minimum period considered ideal for follow-up in such clinical studies would be 6 months. Here, the systematic review and meta-analyses evaluated studies with follow-up periods ranging from 6 to 18 months of follow-up.
Due to the broad antibacterial spectrum, especially against anaerobic microorganisms, metronidazole was the first drug tested in the disinfection of caries lesions [5]. Subsequently, drug combinations added to metronidazole were tested for disinfection in the context of caries, pulp, and periapical lesions [6, 23]. These studies concluded that several combinations of drugs are effective for the partial or total elimination of bacteria from samples of carious dentin, infected pulp tissue, dentin of the root canal walls, and dental plaque [6, 23]. These researches supported the development of the LSTR technique [4].
Distinct antibiotics and their combinations have been tested in clinical trials in relation to the LSTR technique to date [4, 9, 12,13,14,15,16,17,18, 24]. The mixture of ciprofloxacin, metronidazole, and minocycline has been that which is the most commonly used [4, 9, 12, 14, 16, 19, 24], with varying drug ratios ranging from 1:1:1 to 1:3:3 (triplicate portions of metronidazole and minocycline) under the name of 3Mix paste. In our results, four studies employed the combination of ciprofloxacin, metronidazole, and minocycline for treatment [9, 12, 14, 16], including two using the 1:3:3 formulation [12, 14]. The diversity of antibiotics, proportions, and vehicles that may possibly interfere in the LSTR clinical and radiographic outcomes should be addressed in the future during in vitro and in vivo studies.
Primary teeth with pulp necrosis, especially those with periapical lesions, may present a worse prognosis of treatment [9]. In such cases, it is justified to use a combination of irrigating solutions, aiming at achieving disinfection and smear layer removal in the root canal system [25, 26]. Despite this, the LSTR treatment that does not employ irrigation also ensured improvement in the clinical prognosis (i.e., regarding pain and sensitivity to percussion), especially in teeth in these situations [8]. Conversely, Daher et al. [15] observed that, regardless of whether the treatment used is pulpectomy or LSTR, the survival rates were significantly lower among teeth with initial pulp necrosis as compared with teeth with irreversible pulp inflammation, pointing to the need for smear layer removal [25, 26].
At the end of any endodontic therapy, the tooth must be restored to prevent microleakage at the restoration–tooth interface [2]. Among the six studies included in the systematic review, only one used glass ionomer cement followed by composite resin and classified the restoration having visible flaws during follow-up as an example of treatment failure [15]. This observation is relevant as it is known that restorative failure can influence the performance of endodontic treatments [27]. Also, previous studies involving primary teeth have reported that the type of material and the time between temporary and final restoration influence the success of pulpectomies [28, 29] and LSTR [28]. The other five studies employed stainless steel crowns as a final restorative material. However, the time between endodontic treatment and the final restoration ranged from the same appointment [9, 14], after 24 h [12], after a week [16], and even 15 days later [13]. The clinical success among those who employed stainless steel crowns was similar for those patients who underwent the restoration at the same appointment [9] and after 15 days [13]. Considering radiographic success, Nakornchai et al. [9] revealed that those who experienced restoration immediately obtained worse results as compared with the findings of Doneria et al. [13]. Despite the importance of the restoration to the prognosis of the treatment already demonstrated in the literature, the authors did not correlate the success of endodontic therapy with final restoration.
Considering the qualitative analysis of the clinical and radiographic results in this systematic review, there were lower radiographic success rates than clinical performance rates achieved with the LSTR technique. As observed in our results, most treatment failures were exclusively radiographic in nature [15] as revealed through the finding of a statistically significant difference when comparing the outcomes for radiographic success between the two techniques [13, 14].
This result corroborates with those of a previous retrospective study that describes failures in LSTR treatment as being mostly related to radiographic aspects [28]. Though Qadeer et al. [30] showed that a reduction in periapical radiolucency was statistically higher in teeth treated with LSTR when compared with pulpectomy, this result should be interpreted with caution, due to the short follow-up period of the study of only 6 months. In view of this, it should be emphasized that the radiographic follow-up of patients treated with LSTR should be judicious and imperative.
The results of this systematic review and meta-analyses suggest that there is a trend toward increased clinical and radiographic failures in primary teeth following both LSTR and conventional treatments after 6 months of follow-up [9, 12, 13, 16]. It was not possible to reveal differences between the treatments considering the clinical and radiographic results at 6, 12, and 18 months of follow-up in the meta-analyses since the certainty of the evidence was moderate for the clinical criteria and moderate to very low for the radiographic criteria. The performance of treatment is determined by the sum of the clinical and radiographic evaluations [26, 31]. Thus, our results should be interpreted with caution. Three studies demonstrated a statistically significant difference between the techniques [12,13,14], demonstrating the superiority of the conventional approach mainly regarding the radiographic outcome [13, 14]. We emphasize that only four studies could be included in the meta-analyses, which is a limitation of our study. Moreover, the number of RCTs comparing noninstrumental LSTR and pulpectomy is scarce. RCTs with good methodological quality and longer follow-up could possibly disclose differences between the treatments.
Conclusion
Considering the six studies included in the present systematic review, three demonstrated that conventional endodontic treatment for primary teeth was statistically more favorable based on the radiographic criteria. However, through the meta-analyses, it was not possible to disclose any difference between the treatments, regardless of follow-up (6, 12, or 18 months) and type of evaluation (clinical or radiographical). GRADE indicated the quality of evidence was from moderate to very low.
References
Ahmed HM (2014) Pulpectomy procedures in primary molar teeth. Eur J Gen Dent 3:3–10
AAPD. American Academy on Pediatric Dentistry Clinical Affairs Committee – Pulp Therapy Subcommittee (2019-2020) Pulp therapy for primary and immature permanent teeth. Pediatr Dent:353–361
Poornima P, Subba Reddy VV (2008) Comparison of digital radiography, decalcification, and histologic sectioning in the detection of accessory canals in furcation areas of human primary molars. J Indian Soc Pedod Prev Dent Jun 26(2):49–52
Takushige T, Cruz EV, Asgor Moral A, Hoshino E (2004) Endodontic treatment of primary teeth using a combination of antibacterial drugs. Int Endod J Feb 37(2):132–138
Hoshino E, Iwaku M, Sato M, Ando N, Kota K (1989) Bactericidal efficacy of metronidazole against bacteria of human carious dentin in vivo. Caries Res 23(2):78–80
Sato T, Hoshino E, Uematsu H, Noda T (1993) In vitro antimicrobial susceptibility to combinations of drugs of bacteria from carious and endodontic lesions of human deciduos teeth. Oral Microbiol Immunol Jun 8(3):172–176
Hoshino E, Kurihara-Ando N, Sato I, Uematsu H, Sato M, Kota K, Iwaku M (1996) In-vitro antibacterial susceptibility of bacteria taken from infected root dentine to a mixture of ciprofloxacin, metronidazole and minocycline. Int Endod J Mar 29(2):125–130
Ali M, Moral AA, Quader SMA (2017) Evaluation of pain and tenderness in endodontic treatment of deciduous teeth using (LSTR) 3-mix MP therapy. UpDCJ Oct 7(2):09–14
Nakornchai S, Banditsing P, Visetratana N (2010) Clinical evaluation of 3Mix and Vitapex® as treatment options for pulpally involved primary molars. Int J Paediatr Dent May 20(3):214–221
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med Jul 21;6(7):e1000097
Ryan R, Hill S (2019) How to GRADE the quality of the evidence. Cochrane Consumers and Communication Group http://cccrgcochraneorg/author-resources Version 30 March 2019. Accessed 26 July 2019
Agarwal M, Mohan UD, Vishwanath D (2011) A comparative evaluation of noninstrumentation endodontic techniques with conventional ZOE pulpectomy in deciduous molars: an in vivo study. WJD Jul-Sep 2(3):187–192
Daher A, Viana KA, Lees CR, Costa LR (2015) Ineffectiveness of antibiotic-based pulpotomy for primary molars: a survival analysis. Pesqui Bras Odontopediatria Clín Integr 15(1):205–215
Divya DV, Prasad MG, Radhakrishna AN, Sandeep RV, Reddy SP, Santosh Kumar KV (2019) Triple antibiotic paste versus propolis: a clinical quest for the reliable treatment of periapical lesions in primary molars. Saudi Endod J 9:34–39
Doneria D, Thakur S, Singhal P, Chauhan D, Keshav K, Uppal A (2017) In search of a novel substitute: clinical and radiological success of lesion sterilization and tissue repair with modified 3mix-mp antibiotic paste and conventional pulpectomy for primary molars with pulp involvement with 18 months follow-up. Contemp Clin Dent Oct-Dec 8(4):514–521
Zacharczuk GA, Toscano MA, López GE, Ortolani AM (2019) Evaluation of 3Mix-MP and pulpectomies in non-vital primary molars. Acta Odontol Latinoam 32(1):22–28
Grewal N, Sharma N, Chawla S (2018) Comparison of resorption rate of primary teeth treated with alternative lesion sterilization and tissue repair and conventional endodontic treatment: an in vivo randomized clinical trial. J Indian Soc Pedod Prev Dent 36:262–267
Rewal N, Thakur AS, Sachdev V, Mahajan N (2014) Comparison of endoflas and zinc oxide eugenol as root canal filling materials in primary dentition. J Indian Soc Pedod Prev Dent 32:317–321
Prabhakar AR, Sridevi E, Raju OS, Satish V (2008) Endodontic treatment of primary teeth using combination of antibacterial drugs: an in vivo study. J Indian Soc Pedod Prev Dent Jan;26 Suppl 1:S5-10
Najjar RS, Alamoudi NM, El-Housseiny AA, Al Tuwirqi AA, Sabbagh HJ (2019) A comparison of calcium hydroxide/iodoform paste and zinc oxide eugenol as root filling materials for pulpectomy in primary teeth: a systematic review and meta-analysis. Clin Exp Dent Res Mar 4;5(3):294-310
Smaïl-Faugeron V, Glenny AM, Courson F, Durieux P, Muller-Bolla M, Fron Chabouis H (2018) Pulp treatment for extensive decay in primary teeth. Cochrane Database Syst Rev May 31;5:CD003220
Rodd HD, Waterhouse PJ, Fuks AB, Fayle SA, Moffat MA (2006) British Society of Paediatric Dentistry. Pulp therapy for primary molars. Int J Paediatr Dent Sep;16 Suppl 1:15-23
Sato T, Hoshino E, Uematsu H, Kota K, Iwaku M, Noda T (1992) Bactericidal efficacy of a mixture of ciprofloxacin, metronidazole, minocycline and rifampicin against bacteria of carious and endodontic lesions of human deciduous teeth in vitro. Microb Ecol Health Dis 5(4):171–177
Reddy GA, Sridevi E, Sai Sankar AJ, Pranitha K, Pratap Gowd MJS, Vinay C (2017) Endodontic treatment of chronically infected primary teeth using triple antibiotic paste: an in vivo study. J Conserv Dent Nov-Dec 20(6):405–410
Pintor AV, Dos Santos MR, Ferreira DM, Barcelos R, Primo LG, Maia LC (2016) Does smear layer removal influence root canal therapy outcome? A systematic review. J Clin Pediatr Dent Winter 40(1):1–7
Barcelos R, Tannure PN, Gleiser R, Luiz RR, Primo LG (2012) The influence of smear layer removal on primary tooth pulpectomy outcome: a 24-month, double-blind, randomized, and controlled clinical trial evaluation. Int J Paediatr Dent Sep 22(5):369–381
Gillen BM, Looney SW, Gu LS, Loushine BA, Weller RN, Loushine RJ, Pashley DH, Tay FR (2011) Impact of the quality of coronal restoration versus the quality of root canal fillings on success of root canal treatment: a systematic review and meta-analysis. J Endod 37(7):895–902
Duanduan A, Sirimaharaj V, Chompu-inwai P (2013) Retrospective study of pulpectomy with Vitapex® and LSTR with three antibiotics combination (3Mix) for non-vital pulp treatment in primary teeth. CMU J Nat Sci 12(2):131–139
Moskovitz M, Sammara E, Holan G (2005) Success rate of root canal treatment in primary molars. J Dent 33(1):41–47
Qadeer S, Munir B, Yousuf Dar S (2016) Comparison of effectiveness of triple antibiotic paste (3mix) and Vitapex for root canal treatment of pulpally involved primary molars. Pakistan Oral & Dental Journal Oct-Dec 36(4):654–657
Tannure PN, Azevedo CP, Barcelos R, Gleiser R, Primo LG (2011) Long-term outcomes of primary tooth pulpectomy with and without smear layer removal: a randomized split-mouth clinical trial. Pediatr Dent Jul-Aug 33(4):316–320
Funding
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior, Brasil (CAPES) (finance code 001) and Fundação Carlos Chagas Filho de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ) – APQ1 2010.352/2019 and E-26/202-399/2017.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Duarte, M.L., Pires, P.M., Ferreira, D.M. et al. Is there evidence for the use of lesion sterilization and tissue repair therapy in the endodontic treatment of primary teeth? A systematic review and meta-analyses. Clin Oral Invest 24, 2959–2972 (2020). https://doi.org/10.1007/s00784-020-03415-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03415-0