Abstract
Objectives
This systematic review (SR) aimed to investigate the influence of obturation extent on the final outcome of root canal treatment (RCT), by answering the question “among patients requiring RCT on fully formed permanent teeth, is there an association between obturation extent and the final treatment outcome?”
Materials and methods
Five electronic databases and three gray literature searches were performed. Observational studies investigating the association between obturation extent and RCT outcome in fully formed permanent teeth with a minimum follow-up of 12 months were included. We evaluated the risk of bias (RoB) in with MAStARI for cohort studies. The overall quality of the evidence was assessed with the GRADE-tool.
Results
Twenty-two studies were included, 2 had high RoB, 7 moderate RoB, and 13 low RoB. Underextended obturation demonstrated increased odds of an unfavorable outcome in seven studies, in which the odds varied between 6.94 (95%CI 2.20–21.87) and 1.73 (95%CI 1.02–2.95). Overextended obturation also demonstrated this association in four studies, with odds varying from 1.90 (95%CI 1.23–2.94) to 23.00 (95%CI 5.58–94.75). Due to heterogeneity and the very low level of evidence found in the GRADE analysis, the results from this SR should be interpreted with caution.
Conclusions
Obturation extent seems to influence RCT outcome; overextended and underextended obturations showed higher chance of association with less favorable outcomes than adequate obturation; however, this association was not categorically supported.
Clinical relevance
This SR provides information about obturation extent influence on RCT outcome and guides clinicians to make evidence-based decisions during endodontic practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Root canal treatment (RCT) outcome can only be assessed through case follow-up [1]. According to the European Society of Endodontology (2006), follow-up should be regularly performed for at least 1 year after RCT conclusion, aiming to monitor apical health progress [1].
Several studies have suggested that the quality of RCT may influence its outcome, and RCT quality is frequently assessed through periapical radiographs (PA) [2,3,4]. The criteria mostly used include the incidence of procedural errors and obturation characteristics, such as length and density [5, 6].
Working length, as well as obturation extent, is traditionally defined by PA [4, 6, 7], and currently, the use of electronic apex locators has made those measurements more objective and reliable [8]. As reported by the American Association of Endodontists, underextended obturation is considered an incomplete obturation of the root canal space, and overextended obturation is described as material extending beyond the radiographic apex [9]. However, there is no consensus among researchers regarding the ideal obturation extent [3, 4, 6]. On the other hand, other investigators suggested that acceptable obturation extent should end less than 2 mm away from the radiographic apex [7].
A previous systematic review published in 2008 used the terminology of short, flush, and over-filling to categorize the characteristics of root canal obturation; however, the precise obturation extent (mm) was not reported or considered by the authors [4]. Nonetheless, according to the authors, short and flush obturations were related to higher odds of favorable outcome than over-filling. Conversely, when only teeth with preoperative periapical lesions were considered, the odds of a favorable outcome for short and over-filling obturations were not significantly different [4].
Because that study was published more than 10 years ago from this publication and new data on RCT outcomes have been published, a further systematic review with more recent data is proposed. Therefore, this systematic review aims to assess the influence of obturation extent in RCT outcome by answering the following question “among patients requiring RCT on fully formed permanent teeth, is there an association between obturation extent and final treatment outcome?”
Methods
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Checklist [10].
Protocol and registration
A systematic review protocol based on the PRISMA Protocols (PRISMA-P) [11] was registered at the International Prospective Register of Systematic Reviews (PROSPERO) under the number CRD42017079444 [12].
Eligibility criteria
The question of this systematic review was formulated using the acronym PECOS (Population, Exposition, Comparison, Outcomes, Studies), of which (P) human permanent teeth with complete root formation; (E) primary root canal treatment (with the root canal obturation apical extent reported); (C) none or studies comparing different apical extent groups; (O) endodontic therapy outcome (odds ratio, success rate, post-operative symptomatology, signs of infection, periodontal ligament status, or periodontal bone status); and (S) clinical trials and observational studies. It is important to emphasize that only primary RCT data were considered in this systematic review, and therefore, articles on root canal retreatment were excluded. No time restrictions for publications were applied.
The following exclusion criteria were applied: (1) Studies in primary teeth; (2) studies in open apex teeth; (3) studies in which the RCT outcome was not described or correlated with obturation extent; (4) studies with less than 12 months of clinical follow-up; (5) studies with mixed treatment and retreatment data; (6) studies in which data were not clearly reported; (7) reviews, case reports, protocols, short communications, personal opinions, letters, posters, conference abstracts, and laboratory research; (8) studies not in Latin (Roman) alphabet; (9) full copy not available.
Information sources and search strategy
Individual search strategies were developed for the following databases: Latin American and Caribbean Health Sciences (LILACS), LIVIVO, PubMed, Scopus, and Web of Science. A search in gray literature was performed, including Google Scholar, Open Grey, and ProQuest. All searches were conducted from the earliest date available until October 10th, 2017 (Appendix 1). All references were managed in a reference software (EndNote X7®, Thomson Reuters, Philadelphia, PA), in which collection of references and duplicate removal were conducted.
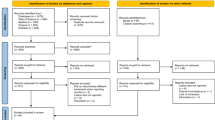
Study selection
Selection of studies was conducted in two phases. Phase 1 was performed in a systematic review web application (Rayyan®, Qatar Computing Research Institute), in which two authors reviewed the identified references’ titles and abstracts. In phase 2, the same reviewers applied the eligibility criteria for full-text studies. In addition, the reviewers screened the reference list of selected studies individually aiming to identify potentially relevant articles. Any disagreement was resolved between the two authors and, if there was not a consensus, a third author was consulted to make a final decision.
Data collection process and data items
Two authors collected key data from selected references; any disagreement was solved between the authors. Data collection consisted of study characteristics (author, year of publication, country, and study design), sample characteristics (size, obturation extent, RCT technique, and follow-up period), outcome assessment (clinical and radiographic criteria), and studies’ main results. If the required data were not complete or the data presented could not be extrapolated, attempts were made to contact the authors by e-mail to retrieve the missing information. No further information was obtained through these contact attempts.
Risk of bias in individual studies
The Meta-Analysis of Statistics Assessment and Review Instrument (MAStARI) for cohort studies was utilized to evaluate included studies [13]. Two reviewers assessed the risk of bias (RoB) for each study and crosschecked the information. RoB was categorized as “high” when the study reached up to 49% score “yes”; “moderate” when the study reached 50% to 69% score “yes”; and “low” when the study reached more than 70% score “yes.” The figures were generated with Review Manager 5.3 (RevMan 5.3, The Nordic Cochrane Centre, Copenhagen, Denmark).
Summary measures
The association between RCT outcome and obturation extent was the main outcome evaluated. RCT outcome was reported or calculated as odds ratio (95%CI), success rates, and healing rates (reported or calculated as percentage). For the purposes of synthesis, “favorable” outcome was defined according to the report of the included studies, based on the success and healing parameters. Studies were grouped based on the ideal endpoint reported for the obturation.
Synthesis of results
A qualitative analysis based on RCT outcome was performed. A meta-analysis was planned if sufficient data were available and whenever the studies were considered homogeneous regarding study design, interventions, and outcomes. A qualitative analysis of results based on the influence of obturation extent on RCT outcome was performed. In order to decrease heterogeneity among studies, results were separated according to the ideal endpoint reported.
Risk of bias across studies
The quality of evidence, as well as the strength of the recommendations, was assessed and a summary was presented using “Grading of Recommendations Assessment, Development and Evaluation” (GRADE) Summary of Findings (SoF) tables, from GRADEpro software (McMaster University, Hamilton, Canada) [14].
Additional analyses
Sensitivity analysis with regard to RoB subgroups (low, moderate, and high RoB) was conducted to verify whether the results of the systematic review were altered.
Results
Study selection
The search strategy resulted in 2170 references once the duplicates were removed. After phase 1, 61 articles were included for full-text assessment. In phase 2, 39 articles were excluded due to different reasons (Appendix 2). Finally, 22 cohort studies were included for final evaluation [3, 15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35] (Fig. 1).
Studies characteristics
The follow-up period ranged from 1 [15, 21, 24, 28, 31, 35] to 19 years [29]. The examined parameter varied, including teeth, roots, canals, and more than one of these parameters. Furthermore, the studies’ sample size varied from 85 [27] to 1139 teeth [20]; from 143 [26] to 551 roots [19]; and from 236 [35] to 1369 canals [30].
Obturation extent assessment
The obturation extent assessment varied between studies; variable endpoints were suggested as ideal. One study considered an adequate obturation within 3 mm from the radiographic apex [29], ten studies within 2 mm [3, 17, 21, 23, 25, 26, 28, 31, 33, 35], three within 1 mm [20, 22, 24], and three at the apex (0 mm) [15, 19, 30]. One study not stated an endpoint and considered an adequate obturation the range of 0.5 to 1.5 mm from the apex [32]. Two studies measured the obturation extent in mm from the radiographic apex and reported the results in means [16, 34]. Finally, one study classified as over-filling or underfilling, which was assorted in three categories: 0 to 0.4 mm, 0.5 to 1.0 mm, and 1.1 to 2.0 mm [27].
For pooled data analysis purposes, included studies were grouped based on the ideal endpoint reported. For studies that stated an endpoint (in mm) as adequate obturation extent, the underextended obturation was considered when that endpoint extent was not reached, and incomplete obturation was radiographically observed. In contrast, for all included studies, an overextended obturation was described as obturation material extending beyond the radiographic apex.
RCT outcome
RCT outcome evaluation was performed mainly by PA assessment. Only one study compared cone beam computed tomography (CBCT) and PA assessments [26]. Additionally, five studies classified the apical healing according to the Periapical Index (PAI) [17, 18, 23, 29, 31]. Three of them executed a dichotomized analysis grouping PAI 1 and 2 for normal periapical status, and PAI 3, 4, and 5 representing the presence of apical periodontitis [17, 29, 31].
Risk of bias within studies
Two studies were classified as high RoB [15, 24], seven as moderate RoB [20,21,22, 27, 28, 34, 35], and thirteen as low RoB [3, 16,17,18,19, 23, 25, 26, 29,30,31,32,33] (Appendix 3). For most studies, the questions “are confounding factors identified and strategies to deal with them stated?”, and “are outcomes assessed using objective criteria?” were scored as “high RoB”, since data were not presented separately for vital and non-vital teeth nor PAI criteria or other validated criteria were utilized for periapical healing assessment. The question “has bias been minimized in relation to selection of cases and of controls?” was considered as “not applicable” for all included studies as none of them presented data in regard to controls (Fig. 2).
Risk of bias graph. Q1 Is sample representative of patients in the population as a whole?; Q2 Are the patients at a similar point in the course of their condition/illness?; Q3 Has bias been minimized in relation to selection of cases and of controls?; Q4 Are confounding factors identified and strategies to deal with them states?; Q5 Are outcomes assessed using objective criteria?; Q6 Was follow-up carried out over a sufficient time period?; Q7 Where the outcomes of people who withdrew described and included in the analysis?; Q8 Were outcomes measured in a reliable way?; Q9 Was appropriate statistical analysis used?
Results of individual studies
Since most included studies considered that adequate obturation was within 2 mm from the radiographic apex, this endpoint was considered as “adequate” for the purpose of this section, unless otherwise stated. Detailed information about included studies’ results are available in Table 1.
Adequate obturation presented higher “healed” rates than inadequate obturations (which included both over and underextended) in the study of Chugal et al. (2003) [16], while both adequate (within 3 mm from the radiographic apex) and overextended obturations showed higher “healed” rates compared to underextended obturations in the study of Pirani et al. (2015) [29]. Moreover, Lee et al. (2012) suggested that adequate obturations presented higher rates of periapical healing than overextended obturations, although no differences in periapical healing were observed between underextended and overextended obturations [25].
Four studies found that the success rates were lower in under and overextended than in adequate obturations (at the apex [15], within 1 mm [20, 24], and within 2.5 mm from the radiographic apex [30]), from which one [20] found no statistical difference between under and overextended obturations. In addition, Helling et al. (2001) found no differences in the success rates between adequate, under, and overextended obturations [21], while Tamarut et al. (2006) suggested that teeth with unsuccessful outcomes presented on average with underextended obturations [34].
Ilgüy et al. (2012) showed that PAI of adequate obturations (within 1 mm from the radiographic apex) was lower than under and overextended obturations [23]. In addition, Ridell et al. (2006) reported that teeth with apical periodontitis in the follow-up period were more likely to have under or overextended obturations [31].
Halse and Molven (1987) reported that overextended obturations had lower rates of success than obturations ending at the radiographic apex [19]. Similarly, Matsumoto et al. (1987) concluded that overextended obturations presented lower repair rates than obturations within 0.5 and 1 mm from the radiographic apex [27]. In addition, two studies reported that the extrusion of endodontic cement was not significantly associated with lower healing rates [17, 18].
Liang et al. (2011) compared the influence of obturation extent in the presence of post-treatment periapical lesions using PA and CBCT [26]. As a result, in PA, the presence of under or overextended obturation presented higher rates of post-treatment apical lesions when compared to adequate obturations, while in CBCT analysis, obturation extent did not affect the presence/absence of post-treatment apical lesions (p > 0.05).
Regarding the influence of obturation extent on periapical repair, ten studies investigated teeth with preoperative normal/diseased apical tissues separately [3, 16, 18, 19, 22, 28, 30, 32, 33, 35]. Three of them reported that teeth with preoperative vital pulp or absence of radiolucency have higher rates of a favorable outcome related to underextended obturation [16, 22, 28], and Tani-Ishii and Teranaka (2003) reported that all teeth with normal preoperative apical conditions remained unchanged during the follow-up appointments [35].
Considering teeth with preoperative periapical lesions, Chugal et al. (2003) showed that obturation extent was closer to the radiographic apex in cases with favorable than with unfavorable outcomes [16]. Similarly, two other studies concluded that failure rates were higher on underextended or overextended than in adequate obturations [3, 33]. Additionally, Halse and Molven (1987) reported that overextend obturations have higher rates of an unfavorable outcome in teeth with preoperative periapical lesions [19]. Interestingly, Santos et al. (2010) found no association between obturation extent and maintenance of apical lesion [32].
Synthesis of results
Among all included studies, eleven studies described an endpoint (in mm) considered as adequate obturation extent and reported enough data to calculate the odds ratio of unfavorable outcome related to underextended and overextended obturations [3, 15, 20,21,22, 24, 26, 28, 29, 33, 35]. These studies were grouped by their ideal endpoint stated. Forest plots were constructed for the odds ratio measured (Figs. 3 and 4). High clinical and methodological heterogeneity across studies was found, reflecting differences in RCT techniques, outcome assessments, obturation extent assessments, and follow-up periods. Thus, a pooled quantitative synthesis was not recommended.
Underextended obturation
One study considered the adequate obturation extent within 3 mm from the radiographic apex, and showed that underextended obturation (less than 3 mm) presented increased odds (4.26; 95%CI = 2.1–8.7) of unfavorable outcome when compared to adequate obturation extent. For studies (n = 6) that considered the adequate obturation extent within 2 mm from the radiographic apex, odds of unfavorable outcome for underextended obturations (less than 2 mm) varied between 0.93 (95%CI = 0.5–1.6) and 6.94 (95%CI = 2.2–21.9) when compared to adequate obturation extent.
For studies (n = 3) that considered the adequate obturation extent within 1 mm from the radiographic apex, odds of unfavorable outcome for underextended obturations (less than 1 mm) varied between 1.73 (95%CI = 1.0–2.9) and 7.67 (95%CI = 0.9–60.2) when compared to adequate obturation extent. One study considered the adequate obturation extent at the apex (0 mm), in which the underextended obturation (shorter than 0 mm) presented increased odds (5.67; 95%CI = 2.1–15.5) of unfavorable outcome when compared to adequate obturation extent.
Overextended obturation
Odds of unfavorable outcome for overextended obturations (n = 11) varied between 0.72 (95%CI = 0.3–1.7) and 23.00 (95%CI = 5.6–94.7) when compared to adequate obturation extent.
Risk of bias across studies
The quality of evidence of this systematic review was classified as very low for all outcome measures (Table 2). The high and moderate RoB of some included studies and the high inconsistency between them influenced these results. Inconsistency was rated according to the heterogeneity of studies.
Additional analyses
Among the eleven studies that enabled calculation of odds ratio of unfavorable outcomes related to under and overextended obturations, the odds of unfavorable outcomes for underextended obturations in studies classified as low RoB (n = 4) varied between 1.45 (95%CI = 0.2–8.3) and 6.94 (95%CI = 2.2–21.9), and for overextended obturation varied between 0.96 (95%CI = 0.4–2.5) and 4.60 (95%CI = 1.8–11.9) when compared to adequate obturation. Odds of unfavorable outcome for underextended obturations in studies classified as moderate RoB (n = 5) varied between 0.93 (95%CI = 0.5–1.6) and 7.67 (95%CI = 0.9–60.2), and for overextended obturation varying between 0.72 (95%CI = 0.3–1.7) and 23.00 (95%CI = 5.6–94.7). Only two studies were classified as high RoB; therefore, sensitivity analysis was not justifiable.
Discussion
Summary of evidence
This systematic review aimed to investigate the association between obturation extent and RCT outcome including studies with a minimum 1-year follow-up. The selected sample consisted of 22 studies, with a total of 1139 endodontic treated teeth. Among the included studies, various obturation extents were suggested as adequate. Thus, studies were grouped based on the endpoint (in mm) stated as adequate. Since these subgroups reflected differences in under and overextended parameters that differently interfer RCT outcome, and considering the high heterogeneity of the included studies, a meta-analysis was not executed.
The adequate obturation extent reported in the included studies ranged from 3 to 0 mm from the radiographic apex. Among them, only eleven studies reported enough data to enable calculation of the odds ratio, and were separated in the following subgroups according to the distance of the obturation from the radiographic apex: 3 mm [29], 2 mm [3, 17, 21, 23, 25, 26, 28, 31, 33, 35], 1 mm [20, 22, 24], and at the apex (0 mm) [15]. Underextended obturation was considered when obturation extent did not reach the ideal endpoint stated, and an incomplete obturation was radiographically observed, whereas, for all included studies, an overextended obturation was defined as obturation material extending beyond the apex.
As a result, seven studies reported a positive association between underextended obturation and increased odds of failure in RCT [3, 15, 20, 24, 28, 29, 33]. In these studies, underextended obturation was associated with higher odds of failure when compared with adequate obturations, with reported odds ranging between 1.73 (95%CI = 1.02–2.95) and 6.94 (95%CI = 2.2–21.9). The presence of underextended obturation may represent the presence of contaminated tissue in the final extension of the root canal system, which can contribute to the maintenance of apical bacterial biofilms, and therefore influence the outcome of RCT [36, 37]. However, due to the lack of standardized criteria for obturation extent assessment, future studies evaluating these criteria are required to reach safe conclusions.
Regarding overextended obturations, four studies reported increased odds of failure in overextended obturations compared to adequate obturation, with odds ranging between 1.90 (95%CI = 1.23–2.94) and 23.00 (95%CI = 5.58–94.75). The presence of overextended obturation represents the existence of foreign bodies in the periapical region, which may not be biocompatible, and therefore can increase inflammation and influence the healing rates in cases of RCT [38]. Two of the studies included [16, 34] provided data as the mean distance from the radiographic apex, which can facilitate comparisons with other studies and provide more reliable data.
Considering the data collected by the present study, obturation extent seems to influence the RCT outcome in function of the pulp tissue condition. Teeth with irreversible pulpitis (vital teeth) exhibiting bacterial colonization usually do not show colonies in the apical third of the roots [39]. Therefore, instrumentation and obturation at the foramen level is not necessary [3, 40]. In contrast, non-vital teeth show bacterial infection extending throughout the entire root canal system, with common formation of biofilms in the apical portion and beyond the apical foramen [41, 42]. Instrumentation at the apex level is highly recommended in teeth with periapical lesions, followed by apical enlargement attempting to reduce the microbial content and to facilitate periapical healing [43, 44]. In the present study, teeth without apical lesion demonstrated higher chances of favorable outcomes when obturation was placed shorter from the apex.
The authors of the present study understand that, for an effective decrease in the toxic content of the root canal system, not only instrumentation and obturation at a level close to the apical foramen are necessary to reach a favorable outcome in non-vital teeth [45]. Other factors, such as foraminal patency [43, 46], the use of intracanal medication prior to obturation [47], and the use of irrigation techniques with solutions that optimize sanification of the root canal system [48, 49], in addition to the advent of engine-driven instruments [50, 51], newer warm gutta-percha obturation techniques [52] and more tapered preparation [53], are also fundamental.
The findings of this study demonstrated that an obturation extent as close as possible to the apical foramen presented a positive correlation with treatment success in non-vital teeth. A retrospective study regarding 2000 clinical cases with proper samples and adequate exclusion and inclusion criteria reported high success rates when root canal instrumentation and obturation limits were established close to apical constriction [54]. Thus, it can be presumed that a root canal obturation close to the apical limit, in spite of other factors that may affect the success of the treatment, is indicative of a favorable prognosis.
The extrusion of endodontic sealers (cement) did not influence RCT outcome in the two studies [17, 18] that evaluated this association. Additionally, one study [19] investigated the influence of overextended obturation (both gutta-percha and sealer) on the rates of favorable outcomes and found that it did not influence the healing rates as most extruded material had been reabsorbed at the follow-up appointment. However, these findings are not consistent with the results of several studies, which demonstrated that the extrusion of obturation materials beyond the apical foramen is responsible for RCT complications [55,56,57,58]. Flare-ups and foreign body type reaction are the most common occurrences and are positively correlated with RCT complications [55]. Thus, due to the limited number of studies assessed in this systematic review, further prospective cohort studies are required to reach a definitive conclusion.
Most included studies used PA for RCT outcome assessment, which is limited by its bi-dimensional nature. However, a consensus regarding RCT outcome assessment is lacking. The PAI scoring system has been proposed for assessing periapical status through PA, and consequently addressing the apical healing status after RCT in teeth with apical lesions [59]. This system grades the apical lesions from 1 to 5, from which scores 4 and 5 at the follow-up are considered as an ultimate failure, and 1 or 2 as an absolute success. Score 3 is controversial, and some studies considered it as a success [59]. From the included studies, only five evaluated apical healing through the PAI [17, 18, 23, 29, 31], which emphasizes the need for standardized criteria for assessing RCT outcome. Moreover, the obturation extent assessment through PA is limited by the anatomical variation of the anatomic foramen [60]. Usually, the anatomical foramen does not coincide with the radiographic apex [61,62,63]. Thus, obturation distance from radiographic apex must be analyzed with caution. One included study [26] compared the periapical healing of vital teeth treated endodontically between PA and CBCT. CBCT detected periapical lesions in 25.9% of cases and PA in 12.6%; obturation extent did not influence RCT outcome in the CBCT analysis. Although CBCT provides useful information, it has been recommended for selected cases according to ALARA (As Low As Reasonably Achievable) where the radiation dose should follow safety principles [64,65,66].
Limitations
The 22 included studies were considerably heterogeneous, especially regarding study design, sample size, RCT technique, follow-up period, obturation extent, and outcome assessment criteria. Therefore, meta-analysis was not possible. Overextended and underextended obturation had a higher chance of association with a less favorable outcome than adequate obturation, as reported in the majority of the included articles. However, the methods used for investigating RCT outcome were usually poorly described and not validated. It is worth mentioning that most of included articles did not reported data on confounding factors such as preoperative pulpal status, coronal leakage, or carious involvement. As previous mentioned, several confounding factors can influence RCT outcome [2, 3], and therefore, they should be considered in future studies assessing RCT outcome characteristics. For these reasons, this systematic review’s conclusions must be interpreted with caution, and further studies with standardized and validated methods should be conducted. Future studies on this topic are required, aiming to reduce methodological heterogeneity in this topic. The authors suggest that these studies utilize the PAI method for the assessment of the endodontic outcome, and obturation extent should be measured in millimeter and present as mean values.
Conclusion
Obturation extent seems to influence the RCT outcome. Overextended and underextended obturation showed a higher chance of association with less favorable outcome than adequate obturation. However, this influence could not be categorically supported due to other factors which are crucial and may affect proper shaping and cleaning of the root canal system. Due to the limitations of this systematic review, this conclusion must be interpreted with caution.
References
European Society of Endodontology (2006) Quality guidelines for endodontic treatment: consensus report of the European Society of Endodontology. Int Endod J 39:921–930
Stoll R, Betke K, Stachniss V (2005) The influence of different factors on the survival of root canal fillings: a 10-year retrospective study. J Endod 31:783–790
Sjögren U, Hägglund B, Sundqvist G, Wing K (1990) Factors affecting the long-term results of endodontic treatment. J Endod 16:498–504
Ng YL, Mann V, Rahbaran S, Lewsey J, Gulabivala K (2008) Outcome of primary root canal treatment: systematic review of the literature—part 2. Influence of clinical factors. Int Endod J 41:6–31
Eliyas S, Briggs PFA, Harris IR, Newton JT, Gallagher JE (2017) Development of quality measurement instruments for root canal treatment. Int Endod J 50:652–666
Ribeiro DM, Reus JC, Felippe WT et al (2017) Technical quality of root canal treatment performed by undergraduate students using hand instrumentation: a meta-analysis. Int Endod J 53:269–283
Eleftheriadis GI, Lambrianidis TP (2005) Technical quality of root canal treatment and detection of iatrogenic errors in an undergraduate dental clinic. Int Endod J 38:725–734
Martins JN, Marques D, Mata A, Carames J (2014) Clinical efficacy of electronic apex locators: systematic review. J Endod 40:759–777
American Association of Endodontists (2015) Glossary of endodontic terms. American Association of Endodontists, Chicago
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62:1006–1012
Shamseer L, Moher D, Clarke M et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 350:g7647
Booth A, Clarke M, Ghersi D, Moher D, Petticrew M, Stewart L (2011) An international registry of systematic-review protocols. Lancet 377:108–109
Joanna Briggs Institute (2014) The meta-analysis of statistics assessment and review instrument. Joanna Briggs Institute, Adelaide
McMaster University,2015 (developed by Evidence Prime I. GRADEpro GDT: GRADEpro Guideline Development Tool [Software]
Barbakow FH, Cleaton-Jones P, Friedman D (1980) An evaluation of 566 cases of root canal therapy in general dental practice 2. Postoperative observations. J Endod 6:485–489
Chugal NM, Clive JM, Spångberg LSW (2003) Endodontic infection: some biologic and treatment factors associated with outcome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 96:81–90
Farzaneh M, Abitbol S, Lawrence HP, Friedman S (2004) Treatment outcome in endodontics—the Toronto study. Phase II: initial treatment. J Endod 30:302–309
Friedman S, Abitbol S, Lawrence HP (2003) Treatment outcome in endodontics: the Toronto study. Phase 1: initial treatment. J Endod 29:787–793
Halse A, Molven O (1987) Overextended gutta-percha and Kloroperka N-O root canal fillings. Radiographic findings after 10-17 years. Acta Odontol Scand 45:171–177
Harty FJ, Parkins BJ, Wengraf AM (1970) Success rate in root canal therapy. A retrospective study of conventional cases. Brit Dent J 128:65–70
Heling I, Bialla-Shenkman S, Turetzky A, Horwitz J, Sela J (2001) The outcome of teeth with periapical periodontitis treated with nonsurgical endodontic treatment: a computerized morphometric study. Quintessence Int 32:397–400
Hellwig E, Klimek J, Ahrens G (1982) 3-year follow-up of the success of root canal treatments done in student demonstrations. Dtsch Zahnarztl Z 37:949–953
İlgüy D, İlgüy M, Fişekçioğlu E, Ersan N, Tanalp J, Dölekoğlu S (2013) Assessment of root canal treatment outcomes performed by Turkish dental students: results after two years. J Dent Educ 77:502–509
Kane AW, Sarr M, Faye B, Wadji N (1998) Long term evaluation of results of endodontic treatments of dental pulp necrosis (74 cases obturated by the monoconal technique). Dakar Med 43:216–219
Lee AHC, Cheung GSP, Wong MCM (2012) Long-term outcome of primary non-surgical root canal treatment. Clin Oral Investig 16:1607–1617
Liang YH, Li G, Wesselink PR, Wu MK (2011) Endodontic outcome predictors identified with periapical radiographs and cone-beam computed tomography scans. J Endod 37:326–331
Matsumoto T, Nagai T, Ida K, Ito M, Kawai Y, Horiba N, Sato R, Nakamura H (1987) Factors affecting successful prognosis of root canal treatment. J Endod 13:239–242
Peak JD, Hayes SJ, Bryant ST, Dummer PMH (2001) The outcome of root canal treatment. A retrospective study within the armed forces (Royal Air Force). Brit Dent J 190:140–144
Pirani C, Chersoni S, Montebugnoli L, Prati C (2015) Long-term outcome of non-surgical root canal treatment: a retrospective analysis. Odontology 103:185–193
Ricucci D, Russo J, Rutberg M, Burleson JA, Spngberg LSW (2011) A prospective cohort study of endodontic treatments of 1,369 root canals: results after 5 years. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 112:825–842
Ridell K, Petersson A, Matsson L, Mejàre I (2006) Periapical status and technical quality of root-filled teeth in Swedish adolescents and young adults: a retrospective study. Acta Odontol Scand 64:104–110
Santos SMC, Soares JA, Costa GM, Brito-Júnior M, Moreira AN, de Magalhães CS (2010) Radiographic parameters of quality of root canal fillings and periapical status: a retrospective cohort study. J Endod 36:1932–1937
Smith CS, Setchell DJ, Harty FJ (1993) Factors influencing the success of conventional root canal therapy—a five-year retrospective study. Int Endod J 26:321–333
Tamarut T, Kovacevic M, Glavičič S (2006) Influence of the length of instrumentation and canal obturation on the success of endodontic therapy. A 10-year clinical follow-up. Am J Dent 19:211–216
Tani-Ishii N, Teranaka T (2003) Clinical and radiographic evaluation of root-canal obturation with obtura II. J Endod 29:739–742
Chavez de Paz LE (2007) Redefining the persistent infection in root canals: possible role of biofilm communities. J Endod 33:652–662
Noiri Y, Ehara A, Kawahara T, Takemura N, Ebisu S (2002) Participation of bacterial biofilms in refractory and chronic periapical periodontitis. J Endod 28:679–683
Willershausen I, Callaway A, Briseno B, Willershausen B (2011) In vitro analysis of the cytotoxicity and the antimicrobial effect of four endodontic sealers. Head Face Med 7:15
Ricucci D, Langeland K (1998) Apical limit of root canal instrumentation and obturation, part 2. A histological study. Int Endod J 31:394–409
Wu MK, Wesselink PR, Walton RE (2000) Apical terminus location of root canal treatment procedures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 89:99–103
Ricucci D, Siqueira JF (2010) Biofilms and apical periodontitis: study of prevalence and association with clinical and histopathologic findings. J Endod 36:1277–1288
Subramanian K, Mickel AK (2009) Molecular analysis of persistent periradicular lesions and root ends reveals a diverse microbial profile. J Endod 35:950–957
Borlina SC, de Souza V, Holland R, Murata SS, Gomes-Filho JE, Dezan Junior E, Marion JJC, Neto DA (2010) Influence of apical foramen widening and sealer on the healing of chronic periapical lesions induced in dogs’ teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109:932–940
de Souza Filho FJ, Benatti O, de Almeida OP (1987) Influence of the enlargement of the apical foramen in periapical repair of contaminated teeth of dog. Oral Surg Oral Med Oral Pathol 64:480–484
Peters OA, Paque F (2010) Current developments in rotary root canal instrument technology and clinical use: a review. Quintessence Int 41:479–488
Hülsmann M, Schäfer E (2009) Apical patency: fact and fiction—a myth or a must? A contribution to the discussion. Endod Pract Today 3
Pereira TC, da Silva Munhoz Vasconcelos LR, Graeff MSZ et al (2018) Intratubular decontamination ability and physicochemical properties of calcium hydroxide pastes. Clin Oral Investig https://doi.org/10.1007/s00784-018-2549-0
Guneser MB, Arslan D, Usumez A (2015) Tissue dissolution ability of sodium hypochlorite activated by photon-initiated photoacoustic streaming technique. J Endod 41:729–732
Hulsmann M, Hahn W (2000) Complications during root canal irrigation—literature review and case reports. Int Endod J 33:186–193
Mohammed N, Noushad MC, Balan B, Dhanesh N, Jayasheelan N, Revankar VD (2016) Apical extrusion of intracanal bacteria following use of two engine-driven instrumentation techniques: an in vitro study. J Contemp Dent Pract 17:939–942
Ounsi HF, Nassif W, Grandini S, Salameh Z, Neelakantan P, Anil S (2017) Evolution of nickel-titanium alloys in endodontics. J Contemp Dent Pract 18:1090–1096
Moinzadeh AT, Shemesh H, Neirynck NA, Aubert C, Wesselink PR (2013) Bisphosphonates and their clinical implications in endodontic therapy. Int Endod J 46:391–398
Capar ID, Arslan H (2016_ A review of instrumentation kinematics of engine-driven nickel-titanium instruments. Int Endod J 49:119–135, 2016
Imura N, Pinheiro ET, Gomes BP et al (2007) The outcome of endodontic treatment: a retrospective study of 2000 cases performed by a specialist. J Endod 33:1278–1282
Alves FR, Coutinho MS, Goncalves LS (2014) Endodontic-related facial paresthesia: systematic review. J Can Dent Assoc:80:e13
Gluskin AH (2005) Mishaps and serious complications in endodontic obturation. Endod Top 12:52–70
Gonzalez-Martin M, Torres-Lagares D, Gutierrez-Perez JL, Segura-Egea JJ (2010) Inferior alveolar nerve paresthesia after overfilling of endodontic sealer into the mandibular canal. J Endod 36:1419–1421
Koseoglu BG, Tanrikulu S, Subay RK, Sencer S (2006) Anesthesia following overfilling of a root canal sealer into the mandibular canal: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101:803–806
Orstavik D, Kerekes K, Eriksen HM (1986) The periapical index: a scoring system for radiographic assessment of apical periodontitis. Endod Dent Traumatol 2:20–34
Plascencia H, Cruz A, Palafox-Sanchez CA et al (2017) Micro-CT study of the root canal anatomy of maxillary canines. J Clin Exp Dent 9:e1230–e1236
Marceliano-Alves M, Alves FR, Mendes DM, Provenzano JC (2016) Micro-computed tomography analysis of the root canal morphology of palatal roots of maxillary first molars. J Endod 42:280–283
ElAyouti A, Hulber JM, Judenhofer MS et al (2014) Apical constriction: location and dimensions in molars—a micro-computed tomography study. J Endod 40:1095–1099
Tomaszewska IM, Leszczynski B, Wrobel A, Gladysz T, Duncan HF (2018) A micro-computed tomographic (micro-CT) analysis of the root canal morphology of maxillary third molar teeth. Ann Anat 215:83–92
Salineiro FCS, Kobayashi-Velasco S, Braga MM, Cavalcanti MGP (2017) Radiographic diagnosis of root fractures: a systematic review, meta-analyses and sources of heterogeneity. Dentomaxillofac Radiol 46:20170400. https://doi.org/10.1259/dmfr.20170400
Leonardi Dutra K, Haas L, Porporatti AL, Flores-Mir C, Nascimento Santos J, Mezzomo LA, Corrêa M, de Luca Canto G (2016) Diagnostic accuracy of cone-beam computed tomography and conventional radiography on apical periodontitis: a systematic review and meta-analysis. J Endod 42:356–364
SEDENTEXCT (2012) Radiation protection: cone beam ct for dental and maxillofacial radiology. Evidence based guidelines. http://www.sedentexct.eu/files/radiation_protection_172.pdf. Accessed 22 January 2018
Funding
This study was financed in part by the Coordenação deAperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001. FWM is supported by the Fundação de Amparo à Pesquisa e Invovação do Estado de Santa Catarina (FAPESC) [grant number 88887.200724/2018-00]
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This work does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mello, F.W., Miguel, A.F.P., Ribeiro, D.M. et al. The influence of apical extent of root canal obturation on endodontic therapy outcome: a systematic review. Clin Oral Invest 23, 2005–2019 (2019). https://doi.org/10.1007/s00784-019-02897-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-02897-x