Abstract
Objective
To evaluate the survival of atraumatic restorative treatment (ART) restorations using high viscosity glass ionomer cement (GIC), compomer (COM), and glass carbomer (CAR) for occlusal and occlusoproximal cavitated dentin caries lesions in primary molars.
Methods
A total of 568 4–7-year-old children (287 occlusoproximal and 281 occlusal cavities) were selected in Barueri, Brazil. The patients were randomly allocated in three groups: GIC, COM, and CAR. All treatments were performed on school setting following ART premises. Evaluations were performed after 2, 6, 12, 18, 24, and 36 months. Restoration survival was evaluated using Kaplan-Meier survival analysis and log-rank test, while Cox regression analysis was used for testing association with clinical factors (α = 5%).
Results
The overall survival rate after 3 years of occlusal ART restorations was 73% (GIC = 83%; COM = 78%; CAR = 62%) and 49% for occlusoproximal ART restorations (GIC = 56%; COM = 56%; CAR = 36%). CAR restorations were less successful than GIC and COM for both occlusal and occlusoproximal restorations (p < 0.05). No difference was found between GIC and COM (p > 0.05).
Conclusions
GIC and compomer are clinically more successful than CAR for occlusal and occlusoproximal restorations in primary molars.
Clinical significance
Both compomer and high viscosity glass ionomer cement are suitable materials for ART in primary molars. However, glass carbomer cement should not be used for ART (#NCT02217098).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The atraumatic restorative treatment (ART) uses only hand instruments to remove the necrotic dentin and an adhesive restorative material to fill the cavities [1]. Therefore, the ART technique rarely requires local anesthesia and it is less anxiety- and pain-inducing when compared to conventional treatment [2]. Although ART was originally created to provide dental treatment for underprivileged populations and lacking electricity, nowadays, it is one of the most used treatments among children and anxious patients [3, 4].
The high viscosity glass ionomer cement (GIC) is the material of choice for ART, since it presents good biocompatibility, favorable setting time, fluoride ion release, and the ability to bond chemically to enamel and dentin [5]. On the other hand, it is known that low viscosity GICs have lower longevity than high viscosity ones, and therefore, high viscosity GICs should be chosen as ART filling material [6, 7]. However, the mechanical properties of GICs are blamed to be the reason for “less then excellent” performance of these materials, mainly in occlusoproximal cavities, when the material is submitted mainly to flexural tension. Other materials could be used for ART restorations but little is known about their performance when used in field conditions, under relative isolation and after dentinal hand excavation [8].
Besides GIC, another restorative material commonly used in pediatric dentistry is called compomer (COM) [9]. It is a polyacid-modified resin that was developed to match properties of composite resins and GICs [10]. Although COM is claimed to offer better esthetics, more strength and better wear resistance than GIC [11] showing good results in conventional restorations [9], little is known about its survival in combination with ART philosophy [8]. More recently, aiming to improve the physical-mechanical GIC properties, a new material called glass carbomer cement (CAR) was developed. CAR consists of a carbomized nano particles containing GIC added with fluorapatite and hydroxyapatite particles [12]. According to the manufacturer, CAR presents low solubility, high compressive and flexural strengths, and high wear resistance. Additionally, this material is claimed to present excellent chemical bonding to dentin and enamel with the advantage of accelerating the remineralization process [13].
This material had already been tested in laboratorial studies and the findings were controversial [14, 15, 16] but little is known on the clinical performance of this material. To the present time, only clinical trials reporting CAR behavior as sealant are reported [17, 18], while no clinical trial had been conducted to analyze the clinical performance as a restorative material.
Thus, the aim of this study was to evaluate the survival of atraumatic restorative treatment (ART) restorations using high viscosity glass ionomer cement (GIC), compomer (COM), and glass carbomer (CAR) for the management of occlusal and occlusoproximal dentin caries lesions in primary molars.
Materials and methods
This is a three-arm parallel randomized clinical trial. This manuscript was written following the guidelines of CONSORT (Consolidated Standards of Reporting Trials) and registered in the website www.clinicaltrials.gov (#NCT02217098). The CONSORT checklist is available on Supplementary files.
Sample calculation
The sample size calculation was performed using the website sealedenvelope.com. The hypothesis of this study is that no difference between the tested materials (non-inferiority trial). The calculation was based on a previous published systematic review [19] that reported a survival rate of 66% for occlusal and 31% for occlusoproximal ART restorations using GIC after 3 years. We considered a value of 15%, a significance level of 5%, and a power of 80% as a non-inferiority limit. Adding up more 10% to predict possible loss to follow-up, the required sample size was a total of 272 occlusal and 260 occlusoproximal restorations. The experimental unit was the tooth and only one tooth per patient was included in the study.
Sample selection
Two dentists evaluated approximately 3000 children in 23 public schools at the city of Barueri/SP/Brazil from which 568 children were included in this study. All the children took part in an oral health prevention program where they were particularly instructed about to perform good oral hygiene and reduce sugar consumption.
As inclusion criteria, only children aged between 4 and 7 years, with good behavior and good health conditions, with possibility of following-up were screened.
The children were included in the study if they had at least one primary molar with occlusal or occlusoproximal dentin caries lesion accessible to hand instruments. All the other treatment needs from the included children that could not be performed inside the schools, such as endodontic treatment and extractions, were referred to public health centers and performed by the municipality dentists from Barueri.
As exclusion criteria, deep cavities where there was any doubt regarding pulp involvement by clinical diagnosis or teeth with fistula or abscess, history of pain, pulp exposure, and mobility were not included in the study.
Operators
The operators were four final-year undergraduate dental students who received the same training. First, they followed a theoretical lecture regarding the ART concepts. After that, they participated in hands on laboratory-based workshop for practicing ART-restorations on extracted molars. Additionally, the operators underwent 2-week training making ART with all three materials in the selected children, but restoring teeth that were not included in this research.
The operators were assisted by a local dentist and one dental assistant who were previously trained on how to handle the materials according to the manufacturers’ protocol.
Blinding (masking)
The children were randomly assigned into three groups: GIC—high viscosity glass ionomer cement (Equia Fil, GC Europe, Leuven, BE); COM—compomer (Dyract Extra, Dentsply International, York, USA); and CAR—glass carbomer (Glass Carbomer Cement, GCP, Leiden, NL). The materials’ composition is provided in Table 1.
The randomization process was designed in blocks of different sizes generated by the website randomization.com, stratified by occlusal and occlusoproximal cavities. As the materials used in this study had different application forms, it was not possible to completely blind operators and patients. To reduce the allocation bias, the randomization was done by an external dentist who was responsible for handling the materials, after the cavity preparation was completed and the material needed to be inserted.
Treatment procedure
Treatments were performed on school setting, in empty classrooms at schools and without any dental facility.
Cavity preparation followed the ART guidelines [1], and no local anesthesia was used during treatment. In all groups, cavity opening/entrance enlarging was done with a dental hatchet and enamel cutters when necessary. The soft and completely demineralized dentin removal was done with hand excavators, while enamel-dentin junction was left caries free. The restorations were done following the manufactures’ instructions and the details are described in Table 2.
The smear layer removal was only done in the GIC group, as the Equia Fil system contains the cavity conditioner. Although the GIC adhesion is not hampered with smear layer on; it is believed that the removal of such debris with a polyacrylic acid results in better bonding of the material to enamel and dentin [20]. Both glass carbomer and compomer do not require cavity conditioning, so, no smear layer removal was done in these groups. The restorations using compomer were done after applying the adhesive system Prime&Bond (Dentsply).
After cavity preparation, the cavity size was measured using a periodontal probe, in order to determine whether cavity size plays a role in restoration failure. Regarding the volume of the cavity, we classified in three categories: 0–9.9, 10–19.9, and > 20 mm3 (occlusal-cervical; buccal-lingual; mesial-distal measurements) according to the cavity size.
During the treatment, data was collected per child and recorded in individual forms regarding the treated tooth (jaw and side) and child’s caries experience (dmft/DMFT). The cotton rolls were taken off after the materials (CAR and GIC groups) present a hard consistency. After the restoration procedure was finished, the children were instructed not to eat for at least 1 h.
Evaluation
The restorations were evaluated according to the criteria described by Roeleveld et al. [21] by one independent trained evaluator (who did not take part in restoration phase) after 2, 6, 12, 18, 24, and 36 months.
The evaluator’s training was performed with the aid of restored primary teeth images including all the scores of the evaluation criteria. After that, the inter-examiner calibration was performed clinically in 40 children with ART restorations with interval of 1 week between the evaluations, in order to calculate the weighted kappa value for intra-examiner reproducibility. A 0.5-mm diameter ball-shaped periodontal probe was used to measure the marginal defects. The evaluation criteria are described in Table 3.
A restoration was classified as ‘success’ when it was still present, or a slight defect was observed (scores 00 and 10). A ‘failure’ was considered when there was a defect in the filling greater than 0.5 mm, when secondary caries was observed, when the restoration was not present, or when the pulp was inflamed, or the tooth was extracted (scores 11–50). When the tooth was unavailable for evaluation (shedding or patient not present), it was censored (50–90).
Data monitoring
There is no external Data Monitoring Committee. The principal investigator (DPR) has overall responsibility for the study and is custodian of the data. The independent oversight of trial data collection, management, and analysis were undertaken by ICO.
Analysis
All data were processed with Stata 13.0 software (StataCorp, TX, USA). Restoration survival was evaluated using Kaplan-Meier survival analysis and Log-rank test, while Cox regression (univariate and adjusted) analyses were used for testing association with clinical factors. The significant level for the tests was considered as 5%.
Results
Recruitment took place in October/2013, while the treatment was performed from October/2013 to February/2014. The follow-up started in December/2013 and lasted until May/2017.
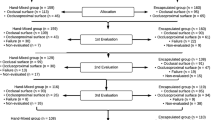
The weighted kappa value for intra-examiner reproducibility was 0.91. In total, 568 children aged 4–7 (average 5.4 years), of 21 different public schools, were treated. Among the participants, 292 (52.5%) were female and 264 (47.5%) were male. Figure 1 shows the flowchart containing all phases of the trial. After 36 months, 274 occlusal and 284 occlusoproximal restorations were evaluated and only 12 children could not be evaluated because they moved to another city (drop-out = 2.2%).
The overall survival rate after 3 years of occlusal ART restorations was 73% (GIC = 83%; COM = 78%; CAR = 62%) and 49% for occlusoproximal ART restorations (GIC = 56%; COM = 56%; CAR = 36%). A difference in survival rate between the materials was found, with a poorer performance of CAR in both occlusal (HR = 2.41; CI = 1.29 to 4.52; p = 0.006) and occlusoproximal restorations (HR = 1.70; CI = 1.13 to 2.55; p = 0.010) when compared to GIC. CAR showed lower survival when compared to COM, in both occlusal (HR = 1.83; IC = 1.05 to 3.21; p = 0.033) and occlusoproximal restorations (HR = 1.79; IC = 1.20 to 2.68; p = 0.004) while no difference was found between GIC and COM, as shown in Tables 4 and 5.
The survival curves, with censored data, are presented in Figs. 2 and 3. Log-rank test indicated significant difference between the materials, both for occlusal (p = 0.007) and for occlusoproximal restorations (p = 0.001).
The main reasons for failure of occlusal ART restorations were restoration missing or disappeared (almost) completely (n = 38), followed by gross marginal defect greater than 0.5 mm and secondary caries (n = 17), and pulp inflammation (n = 11). Regarding occlusoproximal restorations, the main failure reasons were that restoration was missing or disappeared (almost) completely (n = 76), pulp inflammation (n = 36) and gross marginal defect greater than 0.5 mm (n = 31).
The Cox regression analysis showed an association between greater cavity size (> 20mm3) and lower failure rate only for occlusoproximal restorations when compared to smaller cavities (0–9.9 mm3) (Table 5). The other variables, such as operator, jaw, side, and sex, showed no association with the survival of both restoration types.
Discussion
Laboratorial tests are important to predict the clinical behavior as well as to ensure quality control, especially for new developed dental materials. However, it is known that those parameters do not always reflect materials’ clinical performance [22, 23]. In this way, clinical trials are still the most trustable way to insure the efficacy of dental materials [24]. Hence, this study investigated the 3-year survival rate of three different filling material used for occlusal and occlusoproximal ART restorations in primary molars.
Currently, GIC is the material of choice for ART restorations. Thus, the decision to conduct a non-inferiority trial was based on the principle that the experimental materials (CAR and COM) need to be at least as good as the control (GIC) to be indicated for those restorations. However, the results of the present study showed that CAR presents lower survival rate after 3 years compared to COM and GIC for both occlusal and occlusoproximal restorations while no difference was found between GIC and COM.
The main reason for CAR restoration failure was bulk fracture/restoration loss. One possible explanation could be the fact that during the setting reaction of CAR, the hydroxyapatite particles interact to the carboxylic groups, decreasing the amount of ions available to interact to the tooth structure, resulting in lower bond strength, as reported in previous in vitro studies [14, 25]. Another explanation is that during the setting of the material, internal cracks are created [26] and we hypothesize that those cracks could be disseminated leading to a low fracture resistance of the material, culminating on the restoration breakdown.
During the operative phase of this study, an interesting fact was observed by the operators. Even after light curing the material for 60 s, CAR still presented a soft consistency. In fact, the same was observed in a laboratory study [15], in which not all CAR restorations were fully hardened, some not even after 40 h. According to the authors, this phenomenon could result in a higher risk of restoration failure, as observed in our study.
Even with the lower survival rate of CAR, the overall survival rate of occlusal restorations was 74.1 and 50.7% for occlusoproximal. Even though the operators of the present study were undergraduate students, these values are higher than those reported in a meta-analysis [14], which showed a 3-year survival rate of 66% for occlusal surface and 31% for multiple surface ART restorations. When we look at the survival rate of GIC restorations separately, the survival is even higher (83% for occlusal and 58% for occlusoproximal). This finding may be justified by the same level of experience (no operator effect was identified) and by the fact that they followed a comprehensive laboratorial and clinical training prior to the start of the trial, as well as were supervised and assisted during all treatments by a dentist and by an auxiliary experts in ART.
The caries experience of the child was categorized in the analysis according to the Brazilian local average of DMFT/dmft in order to verify if there is any association with the restoration failures. However, both in occlusal and occlusoproximal restorations, no association was found between the caries experience and the restoration failure.
Regarding the classification of cavity volume used in this study, it was adapted from a previous research [27], but instead of using five categories of cavity volume, we used only tree (Tables 4 and 5). The main reason for that decision was that a small amount of restorations had volume higher than 30 mm3, since we avoided selecting deep caries for this study. As expressed in Table 4, the Cox regression analysis showed an association between cavities with a volume greater than 20 mm3 and lower failure rate of occlusoproximal restorations. A possible explanation is that small cavities can lead to poor visibility and difficulties during the material insertion, which could jeopardize the adaptation of the material and create fragility areas in the restoration [27, 28].
The COM is a restorative material often used in pediatric dentistry [29, 30]; however, its hydrophobic characteristic may compromise its use in field conditions [10]. Interestingly, although the treatments were carried out in a school setting, no difference was found between GIC and COM restorations. Thus, COM could be considered an alternative material for ART restorations, especially in cases when higher levels of esthetic are required.
As limitations of this study, we can mention that only the evaluator was blind to the materials. The operators could not be blinded because they have distinguished presentation forms. Yet, in order to control this variable, the information on which material would be used was only given by the assistant after the cavity preparation.
One of the drawbacks of the materials used in this trial is that they cannot be used in a place where electricity is not available, because of the need of a mixer and photo curing light unit. However, although the ART technique was originally created to be performed under field conditions, when no electricity is available, nowadays the ART restorations are daily performed in private dental offices, as well as in public dental health centers [31].
In conclusion, this study shows similar survival between high viscosity GIC and COM for ART restorations on both occlusal and occlusoproximal surfaces. Thus, COM can be used as an alternative restorative material for ART in primary teeth. On the other hand, CAR shows worse survival when compared to the other two materials and should not be used as restorative material in primary teeth.
References
Frencken JE, Holmgren CJ (1999) How effective is ART in the management of dental caries? Community Dent Oral Epidemiol 27:423–430
Roshan NM, Sakeenabi B (2012) Anxiety in children during occlusal ART restorations in primary molars placed in school environment and hospital dental setup. J Clin Pediatr Dent 36:349–352
Smales RJ, Yip H-K (2002) The atraumatic restorative treatment (ART) approach for the management of dental caries. Quintessence Int 33:427–432
Frencken JE (2014) The state-of-the-ART of ART restorations. Dent Update 41:218–220 222–4
Yip HK, Smales RJ, Ngo HC, Tay FR, Chu FCS (2001) Selection of restorative materials for the atraumatic restorative treatment (ART) approach: a review. Spec Care Dent 21:216–221. https://doi.org/10.1111/j.1754-4505.2001.tb00257.x
Olegário IC, Pacheco AL de B, de Araújo MP et al (2017) Low-cost GICs reduce survival rate in occlusal ART restorations in primary molars after one year: a RCT. J Dent 57:45–50. https://doi.org/10.1016/j.jdent.2016.12.006
Frencken JE, Holmgren CJ (2004) ART: a minimal intervention approach to manage dental caries. Dent Update 31:295–8, 301
Louw AJ, Sarvan I, Chikte UME, Honkala E (2002) One-year evaluation of atraumatic restorative treatment and minimum intervention techniques on primary teeth. SADJ 57:366–371
Daou MH, Tavernier B, Meyer J-M (2009) Two-year clinical evaluation of three restorative materials in primary molars. J Clin Pediatr Dent 34:53–58
Gross LC, Griffen AL, Casamassimo PS (2001) Compomers as class II restorations in primary molars. Pediatr Dent 23:24–27
Qvist V, Laurberg L, Poulsen A, Teglers PT (2004) Class II restorations in primary teeth: 7-year study on three resin-modified glass ionomer cements and a compomer. Eur J Oral Sci 112:188–196. https://doi.org/10.1111/j.1600-0722.2004.00117.x
Kahvecioglu F, Tosun G, Ülker HE (2016) Intrapulpal thermal changes during setting reaction of glass Carbomer® using Thermocure lamp. Biomed Res Int 2016:5173805 . doi: https://doi.org/10.1155/2016/5173805, 7
GCP Dental (2011) GCP Dental biocompatible restorative Fill Cement based on Glass Carbomer™ Tech. http://gcp-dental.com/products/gcp-glass-fill/. Accessed 2 Aug 2017
Olegário IC, Malagrana APVFP, Kim SSH, Hesse D, Tedesco TK, Calvo AFB, Camargo LB, Raggio DP (2015) Mechanical properties of high-viscosity glass ionomer cement and nanoparticle glass carbomer. J Nanomater 2015:1–4
Koenraads H, Van der Kroon G, Frencken JE (2009) Compressive strength of two newly developed glassionomer materials for use with the Atraumatic Restorative Treatment (ART) approach in class II cavities. Dent Mater 25(4):551–556
Cehreli SB, Tirali RE, Yalcinkaya Z, Cehreli ZC (2013) Microleakage of newly developed glass carbomer cement in primary teeth. Eur J Dent 7:15–21
Chen X, Minquan D, Fan M, Mulder J, Huysmans M-C, Frencken JE (2012) Effectiveness of two new types of sealants: retention after 2Â years. Clin Oral Investig 16(5):1443–1450
Gorseta K, Glavina D, Borzabadi-Farahani A et al (2014) One-year clinical evaluation of a Glass Carbomer fissure sealant, a preliminary study. Eur J Prosthodont Restor Dent 22:67–71
de Amorim RG, Leal SC, Jo EF (2012) Survival of atraumatic restorative treatment (ART) sealants and restorations: a meta-analysis. Clin Oral Investig 16(2):429–441
Tay FR, Smales RJ, Ngo H et al (2001) Effect of different conditioning protocols on adhesion of a GIC to dentin. J Adhes Dent 3:153–167
Roeleveld AC, van Amerongen WE, Mandari G (2006) Influence of residual caries and cervical gaps on the survival rate of class II glass ionomer restorations. Eur Arch Paediatr Dent 1(2):85–90
Ferracane JL Resin-based composite performance: are there some things we can’t predict? Dent Mater 29:51–58
Sarrett D (2005) Clinical challenges and the relevance of materials testing for posterior composite restorations. Dent Mater 21(1):9–20
MJÖR IA (2007) Minimum requirements for new dental materials. J Oral Rehabil 34(12):907–912
Zainuddin N, Karpukhina N, Law RV, Hill RG (2012) Characterisation of a remineralising Glass Carbomer® ionomer cement by MAS-NMR spectroscopy. Dent Mater 28:1051–1058. https://doi.org/10.1016/j.dental.2012.06.011
Cehreli ZC, Akca T, Altay N (2003) Bond strengths of polyacid-modified resin composites and a resin-modified glass-ionomer cement to primary dentin. Am J Dent 16 Spec No:47A–50A
Kemoli AM, van Amerogen WE (2009) Influence of the cavity-size on the survival rate of proximal ART restorations in primary molars. Int J Paediatr Dent 19:423–430
Kemoli AM, Van Amerongen WE (2011) Effects of oral hygiene, residual caries and cervical Marginal-gaps on the survival of proximal atraumatic restorative treatment approach restorations. Contemp Clin Dent 2(4):318
Santamaria RM, Innes NPT, Machiulskiene V, Evans DJP, Splieth CH (2014) Caries management strategies for primary molars. J Dent Res 93(11):1062–1069
Ghaderi F, Mardani A (2015) Clinical success rate of compomer and amalgam class II restorations in first primary molars: a two-year study. J Dent Res Dent Clin Dent Prospects 9(2):92–95
Holmgren CJ, Frencken JE (1999) Painting the future for ART. Community Dent Oral Epidemiol 27(6):449–453
Acknowledgments
We would like to thank the children and their parents for taking part in this research, the schools staff for their kind aid and assistance. A special thanks to the operators of this trial: Lennaert Pruijn, Joran Aalders, Christine F. Tency and Khahn Do. Also, to the dentists of the Municipal Health Centre of Barueri: Andrea Rodrigues Simões, Rebeca Bergamini de Andrade Massaro, Fernanda Michelloti Cajado and Andrei Alvaro Barrichello Chaves. We would like to thank GC Europe, Dentsply International and GCP Leiden for materials supplying.
Funding
This study was supported by FAPESP-Fundação de Amparo à Pesquisa do Estado de São Paulo (grant numbers: 2015/00565-3 and 2013/11236-5). This study was partially supported by National Council for Scientific and Technological Development from the Brazilian Government (grant numbers: 309521/2015-7 and 306304/2015-5).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors (ICO, DH, FMM, CCB, and DPR) declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This research was approved by the Research Ethics Committee of the Faculty of Dentistry, University of São Paulo (protocol number 464.863).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Olegário, I.C., Hesse, D., Mendes, F.M. et al. Glass carbomer and compomer for ART restorations: 3-year results of a randomized clinical trial. Clin Oral Invest 23, 1761–1770 (2019). https://doi.org/10.1007/s00784-018-2593-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2593-9