Abstract
Objectives
Facial asymmetry is one of the main concerns in patients with a dentofacial deformity. The aims of the study were to (1) evaluate the changes in facial asymmetry after bimaxillary surgery for asymmetric skeletal class II deformity and (2) compare preoperative and postoperative facial asymmetry of class II patients with normal controls.
Materials and methods
The facial asymmetry was assessed for 30 adults (21 women and 9 men, mean age: 29.3 years) who consecutively underwent bimaxillary surgery for asymmetric skeletal class II deformity using cone-beam computed tomography before and at least 6 months after surgery. Thirty soft tissue and two dental landmarks were identified on each three-dimensional facial image, and the asymmetry index of each landmark was calculated. Results were compared with those of 30 normal control subjects (21 women and 9 men, mean age: 26.2 years) with skeletal class I structure.
Results
Six months after surgery, the asymmetric index of the lower face and total face decreased significantly (17.8 ± 29.4 and 16.6 ± 29.5 mm, respectively, both p < 0.01), whereas the asymmetric index of the middle face increased significantly (1.2 ± 2.2 mm, p < 0.01). Postoperatively, 53% of the class II patients had residual chin asymmetry. The postoperative total face asymmetric index was positively correlated with the preoperative asymmetric index (r = 0.37, p < 0.05).
Conclusions
Bimaxillary surgery for patients with asymmetric class II deformity resulted in a significant improvement in lower face asymmetry. However, approximately 50% of the patients still had residual chin asymmetry. The total face postoperative asymmetry was moderately related to the initial severity of asymmetry.
Clinical relevance
These findings could help clinicians better understand orthognathic outcomes on different facial regions for patients with asymmetric class II deformity.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Facial symmetry is generally recognized as one of the features of attractive faces [1, 2]. Although some amounts of facial asymmetry are acceptable and are present on what are considered to be beautiful and attractive faces [3, 4], significant facial asymmetry might severely influence facial appearance and induce psychosocial distress to patients.
The causes of facial asymmetry include skeletal asymmetry, soft tissue asymmetry, and functional asymmetry or a combination [5, 6]. Of these, skeletal asymmetry involving the maxillofacial region is predominant. Orthognathic surgery (OGS) is the only procedure for correcting jaw asymmetry in adult patients. Although several studies have reported the outcome after bimaxillary OGS for facial asymmetry, the lack of normal controls in these studies prevents an objective assessment of whether the outcome is ideal [7,8,9,10,11,12]. Moreover, types of malocclusion in most of these studies were heterogenous; therefore, the outcome of class II asymmetry was unclear [7, 9,10,11]. Although Hajeer et al. reported the outcome of 12 patients with class II deformity, only two of them presented with facial asymmetry before surgery [8]. Furthermore, asymmetric class II patients undergoing bimaxillary OGS have never been systematically studied for outcomes on the areas (e.g., nose, cheek, lip, chin, contour, incisor), parts (midline, paramedian, contour), or zones (middle, lower) of the face. A better understanding of the OGS outcomes on facial areas, parts, or zones may have important clinical implications, including the development of more comprehensive surgical designs that consider facial asymmetry as well as improvements in consultations with patients for this surgical modality.
One of the best methods for assessing the three-dimensional structure of the face is cone-beam computed tomography (CBCT), which has been demonstrated to be a powerful research tool [12, 13]. Although CBCT provides untextured soft tissue data, it can also provide information regarding dental and hard tissue components. Incisors are directly visualized; therefore, they are important for development of a treatment plan and evaluation of the treatment outcome. In addition, because of their higher stability and reproducibility of landmark identification compared to soft tissues, hard tissues are essential for head orientation, registration of CBCT at different timings, and construction of a 3D coordinate system for each subject. Therefore, this CBCT study aimed to (1) evaluate the outcome of bimaxillary OGS in patients with asymmetric skeletal class II deformity and (2) compare the preoperative and postoperative facial asymmetry of class II patients with control subjects. The null hypotheses to be tested were (1) facial asymmetry after bimaxillary OGS is not different from pre-surgery, and (2) the facial asymmetry after bimaxillary OGS is not significantly different from that of normal controls.
Materials and methods
Patients with asymmetric class II deformity
Thirty Taiwanese adults (age ≥ 18 years) with class II deformity (A point–nasion–B point angle > 4°) and significant facial asymmetry (skeletal menton deviation ≥ 2 mm or lip cant ≥ 2 mm) were selected consecutively based on the following criteria: (1) Le Fort I osteotomy and bilateral sagittal split osteotomy (BSSO) advancement surgery by the attending surgeons supervised by one senior surgeon with more than 40 years of experience at the Chang Gung Craniofacial Center between 2010 and 2015, (2) no progressive or chronic temporomandibular joint disorder, (3) no history of craniofacial surgery, (4) no craniofacial deformity or genetic syndromes, and (5) CBCT evaluation at two time points: before surgery and at least 6 months after surgery (i.e., at orthodontic debonding). The hospital’s institutional review board approved the study.
Control subjects
Control subjects were 30 Taiwanese adults with skeletal class I (0 < A point–nasion–B point angle < 4°) and dental class I occlusion. Control subjects were selected consecutively from patients who had undergone CBCT at the Chang Gung Dental Department between 2010 and 2014 for other dental indications (e.g., implant, third molars, dental crowding, or spacing). Controls were excluded based on the following criteria: (1) craniofacial anomaly, (2) anterior open bite, (3) severe dental crowding or spacing, (4) significant facial asymmetry, or (5) history of craniofacial surgery. These subjects were used to generate 3D norms.
Surgical technique
The BSSO was modified from Hunsuck [14] by extending the anterior cut of the osteotomy to the first molar [15, 16]. The Le Fort I osteotomy was performed with a technique similar to that popularized by Bell [17]. No additional surgical intervention other than genioplasty was performed. Rigid fixation was performed with bone plates or screws.
CBCT
CBCT of the head and neck was performed during wakefulness using an i-CAT 3D Dental Imaging System (Imaging Sciences International, Hatfield, PA) with the following parameters: 120 kVp, 0.4 mm × 0.4 mm × 0.4 mm voxel size, 40 s scan time, and 16 cm × 16 cm field of view. The patient’s head was positioned with the Frankfort horizontal (FH) plane parallel to the ground. Throughout the scan, patients were asked not to swallow.
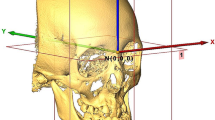
Images were stored in the Digital Imaging and Communications in Medicine (DICOM) format and then transferred to a workstation (Avizo v7.0.0 software, VSG, Bordeaux, France) where they were rendered into volumetric images, segmented, and analyzed by one single investigator (CYF) blinded to subjects’ treatment histories. Before analysis, six skeletal landmarks were selected for registration of the 3D images in a 3D coordinate system (x, y, z) with nasion (N) as the zero point: N, bilateral porion (Po), bilateral orbitale (Or), and basion (Ba). The definition of skeletal landmarks [18] and reference planes are provided in Table 1. A positive coordinate value indicates the left, posterior, and superior side of the face, and a negative value indicates the opposite (Fig. 1). Cranial structures not affected by the surgery were selected to superimpose the CBCT images taken before and after surgery in order to register them in the same 3D coordinate system.
After registration of the 3D images, 30 soft tissue and 2 dental landmarks [13, 18] (Table 2 and Fig. 2) were located on the 3D surface model with coordinates (x, y, z) by the same investigator (CYF) in random order. Multiplanar reconstruction views were also used to identify the landmark when necessary.
Soft tissue and dental landmarks for calculation of asymmetry index. (Left) Soft tissue landmarks: 1, pronasale (Pn); 2, subnasale (Sn); 3, labiale superius (Ls); 4, stomion (Sto); 5, labiale inferius (Li); 6, soft tissue B point (B′); 7, soft tissue pogonion (Pg′); 8, soft tissue menton (Me′); 9, alare right (AlaR); 10, alare left (AlaL); 11, cheek right (ChkR); 12, cheek left (ChkL); 13, cupid’s bow right (CuR); 14, cupid’s bow left (CuL); 15, cheilion right (ChR); 16, cheilion left (ChL); 17, soft tissue lateral chin point right (lC′R); 18, soft tissue lateral chin point left (lC′L); 19, contour Sn point right (cSnR); 20, contour Sn point left (cSnL); 21, contour Ls point right (cLsR); 22, contour Ls point left (cLsL); 23, contour Sto point right (cStoR); 24, contour Sto point left (cStoL); 25, contour Li point right (cLiR); 26, contour Li point left (cLiL); 27, contour B′ point right (cB′R); 28, contour B′ point left (cB′L); 29, contour Pg′ point right (cPg′R); 30, contour Pg′ point left (cPg′L). (Right) dental landmarks: 1, upper incisal embrasure (UIE); 2, lower incisor embrasure (LIE)
Asymmetry index (AI)
To evaluate facial asymmetry, the distances of each landmark to three reference planes were measured as dx, dy, and dz in millimeters [19]. The values of dx, dy, and dz of the nasion were zero. For each paired bilateral landmark, the differences in dx, dy, and dz between the right side and left side indicated the discrepancy of the paired landmarks in three dimensions. For perfect symmetrical paired bilateral landmarks located in the paramedian part, the discrepancy in dx, dy, and dz must approach zero. For perfect symmetrical paired bilateral landmarks located in the contour part, the discrepancy in dx must approach zero because symmetry of facial contour is always perceived from the frontal view. In other words, it is not necessary to take the dy into account. Therefore, the perfect contour symmetry should fulfill the following criteria: no discrepancy in the distance of the bilateral most lateral points of the face from the facial midline on the same horizontal level.
Thus, an AI for each landmark was calculated and designated as follows:
-
AI of facial midline landmarks = dx;
-
AI of facial paramedian landmarks = √ (Ldx − Rdx)2 + (Ldy − Rdy)2 + (Ldz − Rdz)2, where L = left and R = right;
-
AI of facial contour landmarks = √ (Ldx − Rdx)2, where L = left and R = right.
To evaluate facial asymmetry, a total face AI was created, which is the sum of each landmark AI. In addition, every region AI was created, which is the sum of each landmark AI in that region (Table 3). For perfect symmetry, the AI must approach zero.
To define residual asymmetry in class II patients, a cutoff value derived from the normal controls (i.e., mean plus 2 standard deviations [SD]) was calculated [20, 21]. If the postoperative AI was higher than the cutoff value, the asymmetry was more severe than that of approximately 97.72% of the control subjects, which was considered as residual asymmetry (i.e., abnormal asymmetry).
Reliability
To assess intra-examiner reliability, all CBCT measurements were repeated by the same investigator for ten randomly chosen patients 1 month after the measurements. Intra-examiner reliability, analyzed by the intraclass correlation coefficient (ICC), was excellent (mean ICC, 0.954; 95% confidence interval, 0.928 to 0.969).
Statistical analysis
Statistical analyses were performed using the statistical software package SPSS version 17.0 for Windows (SPSS Inc., Chicago, USA). Patient clinical characteristics and CBCT-measured variables were compared before and after surgery using paired t, independent t, or chi-square test when indicated. Pearson correlation analysis was used to assess correlation between postoperative AI and preoperative AI. Probabilities of 0.05 or less were accepted as significant.
Results
Subject characteristics
We studied 30 patients with asymmetric class II deformity (mean age, 29.3 ± 5.6 years; range, 19.0–47.0) and 30 control subjects (mean age, 26.2 ± 4.5 years; range, 18.1–35.5). Patients with class II deformity were not significantly different from control subjects at baseline with respect to sex and overbite. The mean time after surgery was 20.6 ± 7.2 months (range 8.2 to 34.6 months) (Table 4).
Postsurgical changes in class II patients
The surgery was highly effective for class II deformity with significant improvement in the ANB angle (from 7.2 ± 2.0 to 3.7 ± 1.5°, p < 0.001) and overjet (from 4.8 ± 3.0 to 2.7 ± 0.6 mm, p < 0.01). After surgery, the AI of the lower face and total face decreased significantly, whereas the AI of the middle face increased significantly (all p < 0.01). The AI of the chin, lower contour, and lower incisor decreased significantly (p < 0.001, p < 0.05, and p < 0.01, respectively); however, the AI of the nose and upper incisor increased significantly (p < 0.001 and p = 0.05, respectively). The AI of the midline and paramedian parts decreased significantly (both p < 0.01) (Table 5).
Frequency of residual asymmetry in class II patients
After surgery, 66.7% of the Class II patients had residual face asymmetry which was major on the lower face (60%), the midline (80%), and the paramedian (66.7%) parts, or the areas of the nose, upper lip, chin, upper and lower incisors from seven midline landmarks (Sn, Ls, B′, Pg′, Me′, UIE, and LIE), and the transverse differences of two paramedian landmarks (Cu and lC′) (Table 5 through Table 6). Figures 3 and 4 show a patient before and after treatment.
Preoperative and postoperative cone-beam computed tomography of the same patient as shown in Fig. 3. (Left) Before surgery, the total face asymmetric index (AI) and chin AI were 99.2 and 32.7 mm, respectively. (Right) After surgery, the total face AI and chin AI were 50.1 and 11.8 mm, respectively
Correlation between postoperative AI and preoperative AI
Postoperative AI was positively correlated with preoperative AI in five areas: nose, cheek, upper lip, chin, and lower incisor (r = 0.38–0.81, p < 0.05 for cheek, chin, and lower incisor and p < 0.001 for nose and upper lip), two parts: midline and paramedian (r = 0.54, p < 0.01 and r = 0.36, p < 0.05, respectively), middle face (r = 0.71, p < 0.001), and total face (r = 0.37, p < 0.05) (Table 7).
Discussion
To our knowledge, this is the first study to exclusively evaluate the treatment outcome of facial asymmetry after bimaxillary surgery for adult patients with asymmetric skeletal class II deformity. This study provided outcome details by dividing a face into several regions, which could be affected by OGS. The bimaxillary surgery significantly improved asymmetry in the lower face on the chin, lower contour, and lower incisor. However, 53.3% of the patients still had residual chin asymmetry, which was prominent in the transverse direction.
Facial asymmetry is a biological variation that commonly occurs in humans; therefore, it is crucial for clinicians to differentiate normal asymmetry from abnormal asymmetry. On the basis of AI measurements from the normal controls, we found that normal asymmetry was more severe in the lower face than the middle face, which is in agreement with previous studies [22,23,24]. In addition, normal asymmetry was severe in the contour part, moderate in the paramedian part, and mild in the midline part, suggesting a size difference between right and left faces in normal faces.
To identify patients with abnormal asymmetry, we derived a cutoff value, which we defined as the mean plus 2 SD from normal controls. Any asymmetry exceeding this value was considered greater than normal (i.e., abnormal). Similar to normal controls, the initial asymmetry in patients with class II asymmetry was significant in the lower face, which was major on the lower lip, chin, lower contour, and lower incisor (i.e., preoperative mean AI > threshold AI). After surgery, it is not surprising to find the greatest improvement in the chin area (AI improvement 11.9 mm, 49.8%) since chin asymmetry is often a chief complaint of facial asymmetry, and correction of chin asymmetry is an important treatment goal of OGS [10, 25].
Genioplasty is often the last step of OGS for refining the chin position. In this study, most class II patients (28/30) received genioplasty to further improve the facial profile, proportion, or symmetry, in addition to Le Fort I and BSSO procedures. Although the chin asymmetry was significantly improved after surgery, it still remained asymmetric (i.e., final mean AI > threshold AI). This finding is consistent with previous studies on different types of malocclusion [9, 10, 25], which indicates the difficulty in the recognition of facial midline intra-operatively or relapse post-operatively.
Although previous studies have focused on the correction of facial midline asymmetry with OGS, little is known regarding facial contour asymmetry. However, this problem is relevant in clinical practice as some patients seeking OGS do present significant contour asymmetry, especially in the lower contour. In this study, the second highest improvement of lower face asymmetry was in the lower contour (AI improvement 4.1 mm, 33.9%), confirming the ability of proximal segment displacement after BSSO to improve frontal ramal asymmetry [10, 26].
The nose, upper lip, and upper incisor became asymmetric after surgery (i.e., postoperative mean AI > threshold AI). More specifically, the asymmetry was in the transverse direction of subnasale (Sn), labiale superius (Ls), bilateral Cupid’s bow (Cu), and upper incisor embrasure (UIE). This could be explained by the sacrifice of the nasal and maxillary symmetry in order to achieve favorable overall facial symmetry, especially in the mandible. With maxillary osteotomy, nasal asymmetry could be noted due to nasal septal deviation [8, 27]. However, we do not consider this to be a factor, because, at our center, the bony collision during maxillary osteotomy is always avoided by additional resecting the inferior aspect of the septum or superior aspect of ANS or inferior turbinectomy during OGS. This explanation is also supported by the high correlation between the postoperative AI for nose and upper lip (r = 0.78, p < 0.001). Despite the asymmetry, the mean differences of Sn, Ls, Cu, and UIE from the cutoff value were only 0.3, 0.2, 0.4, and 0.2 mm respectively, which were of no clinical significance. In other words, the mean differences of Sn, Ls, Cu, and UIE from facial midline were too small (0.8, 1.0, 2.0, and 1.7 mm, respectively) to reach clinical significance [28, 29].
This study demonstrates that certain initial AI impact postoperative AI. Postoperative AI for nose, cheek, upper lip, chin, lower incisor, middle face, and total face were positively correlated with their initial AI. Postoperative AI for midline and paramedian parts of faces was positively correlated with their initial AI. These correlations have not been reported previously. The clinical implication of this finding is that it is possible to predict asymmetry outcome based on the initial severity of asymmetry, a consideration relevant to surgical design and consultation of patients for this surgery.
There are some limitations to this study. First, this was a retrospective study. However, this limitation was minimized by selecting consecutive patients. Second, the sample size was small. Increasing the power of the study with more patients might have yielded more robust conclusions. Third, 3D soft tissue asymmetry was evaluated via landmark-dependent method, which has been criticized for the questionable validity and reliability for assessing asymmetry [30]. However, the intra-rater reliability of the landmarks used in this study was excellent. Also, the advantage of the landmark method is the ease of interpreting and applying the results to clinical practice [7] compared to those using computer algorithms for assessing full surface asymmetry [11, 30]. Finally, further study is needed to evaluate the impact of facial asymmetry on the treatment outcome of bimaxillary surgery by using class II patients with no significant facial asymmetry as a control group.
Conclusions
In patients with asymmetric class II deformity after bimaxillary OGS, lower face asymmetry on the chin, lower contour, and lower incisor improved significantly. However, approximately 50% of the patients still had residual chin asymmetry. Middle face asymmetry on the nose deteriorated significantly. However, the deterioration was too small to reach clinical significance. The postoperative asymmetry of total face was moderately related to the initial severity of asymmetry.
References
Fink B, Neave N, Manning JT, Grammer K (2006) Facial symmetry and judgements of attractiveness, health and personality. Personal Individ Differ 41:491–499
Ostwald J, Berssenbrugge P, Dirksen D, Runte C, Wermker K, Kleinheinz J, Jung S (2015) Measured symmetry of facial 3D shape and perceived facial symmetry and attractiveness before and after orthognathic surgery. J Craniomaxillofac Surg 43:521–527
Peck S, Peck L, Kataja M (1991) Skeletal asymmetry in esthetically pleasing faces. Angle Orthod 61:43–48
Zaidel DW, Deblieck C (2007) Attractiveness of natural faces compared to computer constructed perfectly symmetrical faces. Int J Neurosci 117:423–431
Bishara SE, Burkey PS, Kharouf JG (1994) Dental and facial asymmetries: a review. Angle Orthod 64:89–98
Cheong YW, Lo LJ (2011) Facial asymmetry: etiology, evaluation, and management. Chang Gung Med J 34:341–351
Ferrario VF, Sforza C, Schmitz JH, Santoro F (1999) Three-dimensional facial morphometric assessment of soft tissue changes after orthognathic surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 88:549–556
Hajeer MY, Ayoub AF, Millett DT (2004) Three-dimensional assessment of facial soft-tissue asymmetry before and after orthognathic surgery. Br J Oral Maxillofac Surg 42:396–404
Yu CC, Bergeron L, Lin CH, Chu YM, Chen YR (2009) Single-splint technique in orthognathic surgery: intraoperative checkpoints to control facial symmetry. Plast Reconstr Surg 124:879–886
Ko EW, Huang CS, Chen YR (2009) Characteristics and corrective outcome of face asymmetry by orthognathic surgery. J Oral Maxillofac Surg 67:2201–2209
Wermker K, Kleinheinz J, Jung S, Dirksen D (2014) Soft tissue response and facial symmetry after orthognathic surgery. J Craniomaxillofac Surg 42:e339–e345
Lee GC, Yoo JK, Kim SH, Moon CH (2016) Lip line changes in class III facial asymmetry patients after orthodontic camouflage treatment, one-jaw surgery, and two-jaw surgery: a preliminary study. Angle Orthod 87:239–245
Kim BR, Oh KM, Cevidanes LH, Park JE, Sim HS, Seo SK, Reyes M, Kim YJ, Park YH (2013) Analysis of 3D soft tissue changes after 1- and 2-jaw orthognathic surgery in mandibular prognathism patients. J Oral Maxillofac Surg 71:151–161
Hunsuck EE (1968) A modified intra- oral sagittal splitting technique for correction of mandibular prognathism, vol 26
Honda T, Lin CH, Yu CC, Heller F, Chen YR (2005) The medial surface of the mandible as an alternative source of bone grafts in orthognathic surgery. J Craniofac Surg 16:123–128
Chen YA, Ng LS, Ko EW, Chen YR (2017) Mandibular contouring during orthognathic surgery using the modified hunsuck technique. J Craniofac Surg 28:239–240
Bell WH (1992) Modern practice in orthognathic and reconstructive surgery. Saunders, Philadelphia
Swennen GRJ, Schutyser FAC, Hausamen JE (2005) Three-dimensional cephalometry: a color atlas and manual. Springer
Ras F, Habets LL, van Ginkel FC, Prahl-Andersen B (1995) Method for quantifying facial asymmetry in three dimensions using stereophotogrammetry. Angle Orthod 65:233–239
Farkas LG (1994) Anthropometry of the head and face. Raven Press
Kowner R (1997) The perception and attribution of facial asymmetry in normal adults. Psychol Rec 47:371–384
Ferrario VF, Sforza C, Miani A Jr, Serrao G (1995) A three-dimensional evaluation of human facial asymmetry. J Anat 186(Pt 1):103–110
Ferrario VF, Sforza C, Ciusa V, Dellavia C, Tartaglia GM (2001) The effect of sex and age on facial asymmetry in healthy subjects: a cross-sectional study from adolescence to mid-adulthood. J Oral Maxillofac Surg 59:382–388
Hwang HS, Yuan D, Jeong KH, Uhm GS, Cho JH, Yoon SJ (2012) Three-dimensional soft tissue analysis for the evaluation of facial asymmetry in normal occlusion individuals. Korean J Orthod 42:56–63
Verze L, Bianchi FA, Schellino E, Ramieri G (2012) Soft tissue changes after orthodontic surgical correction of jaws asymmetry evaluated by three-dimensional surface laser scanner. J Craniofac Surg 23:1448–1452
Ho CT, Lin HH, Liou EJ, Lo LJ (2017) Three-dimensional surgical simulation improves the planning for correction of facial prognathism and asymmetry: a qualitative and quantitative study. Sci Rep 7:40423
Shin YM, Lee ST, Kwon TG (2016) Surgical correction of septal deviation after Le Fort I osteotomy. Maxillofac Plast Reconstr Surg 38:21
Kokich VO Jr, Kiyak HA, Shapiro PA (1999) Comparing the perception of dentists and lay people to altered dental esthetics. J Esthet Dent 11:311–324
Williams RP, Rinchuse DJ, Zullo TG (2014) Perceptions of midline deviations among different facial types. Am J Orthod Dentofac Orthop 145:249–255
Blockhaus M, Kochel J, Hartmann J, Stellzig-Eisenhauer A, Meyer-Marcotty P (2014) Three-dimensional investigation of facial surface asymmetries in skeletal malocclusion patients before and after orthodontic treatment combined with orthognathic surgery. J Orofac Orthop 75:85–95
Funding
The work was supported by the Chang Gung Memorial Hospital, Taiwan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was approved by the Ethics Committee for Human Research, Chang Gung Memorial Hospital, Taoyuan, Taiwan.
Informed consent
Informed consent was not needed due to the retrospective design of the study.
Rights and permissions
About this article
Cite this article
Chen, YF., Liao, YF., Chen, YA. et al. Treatment outcome of bimaxillary surgery for asymmetric skeletal class II deformity. Clin Oral Invest 23, 623–632 (2019). https://doi.org/10.1007/s00784-018-2462-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2462-6