Abstract
Objectives
The aim of this study was to examine levels of salivary mucins in children with deciduous and mixed dentition and to determine correlations between salivary mucins and dental caries status in two dentition stages.
Materials and methods
Saliva samples were collected from preschool children with deciduous dentition aged between 4 and 6 years (n = 60) and school children with mixed dentition aged between 9 and 11 years (n = 60). In each age group, the subjects were divided into two categories: high and low caries risk (n = 30 each). Salivary mucins (MUC5B and MUC7) were measured by enzyme-linked immunosorbent assay (ELISA).
Results
There were no significant differences in MUC5B and MUC7 levels between high and low caries-risk groups in preschool children. Significantly increased MUC5B (p = 0.01) and decreased MUC7 (p = 0.04) levels in a low caries-risk group were demonstrated in school children. No significant correlations were observed between salivary mucins and dental caries in preschool children, whereas a significantly negative correlation (r = −0.29, p = 0.03) between MUC5B and the number of decayed teeth was observed in school children.
Conclusion
Patterns of salivary mucin expression in relation to dental caries were different between preschool and school children. The present findings suggest that changes in oral environment from deciduous to mixed dentition may affect the secretion of salivary mucins in response to dental caries.
Clinical relevance
The present study provides additional information that changes in oral environment from deciduous to mixed dentition stage possibly affect the secretion of salivary mucins in response to dental caries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dental caries is a major public health problem in many developing countries including Thailand. Data from the seventh national oral health survey in 2012 indicated that dental caries was as high as 78.5 % in Thai children aged 5 years and 52.3 % in those aged 12 years [1]. Caries is a unique multifactorial infectious disease which is associated with internal defense factors and external factors [2]. Saliva plays an important role in maintenance of oral health. Saliva contains a large number of proteins including mucins, proline-rich glycoprotein, immunoglobulins, agglutinin, lactoferrin, cystatins, and lysozyme [3]. Saliva is involved in several protective functions of dental structure such as promotion of remineralization, retardation of demineralization, neutralization of acids, and prevention of microbial adherence and their growth [3]. It has been reported that changes in salivary protein compositions involve in dental caries etiology [4–6]. These findings suggest the potential use of salivary proteins as biological indicators of dental caries.
Salivary mucins are glycoproteins and mainly synthesized by the mucus acinar cells of the paired submandibular and sublingual gland as well as minor salivary glands [7, 8]. There are two major types of genetically different salivary mucins, including high molecular weight mucin (MG1 or MUC5B) and low molecular weight mucin (MG2 or MUC7) [4, 7–9]. MUC5B plays an important role in barrier function, lubrication, and protection of the dental surfaces, whereas MUC7 plays a major role in binding of microorganisms and oral clearance of bacteria [3–5, 7–13]. Moreover, salivary mucins are major constituents of the biofilm that covers and protects the oral mucosa and tooth surface [14]. Several studies reported different patterns of salivary mucin secretion in various age groups [14–17]. One previous study demonstrated an association between dental caries index and reduced levels of salivary MUC5B and MUC7 in young adults [6].
To our knowledge, no studies have investigated the levels of salivary mucins in children with different dentition stages. We hypothesized that the alteration of salivary mucin secretion in response to dental caries might be associated with changes in oral environment from deciduous to mixed dentition. The objective of this study was to measure the levels of salivary MUC5B and MUC7 in preschool children with deciduous dentition and school children with mixed dentition and to determine the correlations between levels of salivary mucins and dental caries status in two dentition stages.
Materials and methods
Study participants
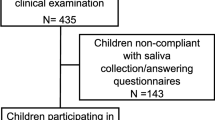
During October 2006 and April 2008, 120 children in preschool level (aged 4–6 years; n = 60) and school level (aged 9–11 years; n = 60) from Khon Kaen University’s Demonstration School were recruited in the study. Criteria for selecting children with tooth decay conditions were adapted from the criteria set by the American Academy of Pediatric Dentistry [18]. In each school level, 30 participants were selected for a high caries-risk group and the other 30 participants were selected for a low caries-risk group. The criteria for a high caries-risk group consisted of the presence of at least one carious tooth, visible plaque on anterior teeth, and having greater than or equal to three between-meal sugary foods per day. Children who did not match these criteria were classified as having low caries risk. Exclusion criteria included history of significant medical conditions, taking any medication known to reduce salivary flow rate, and using fixed or removable prostheses. A self-administered questionnaire was used to collect information on demographic characteristics, frequency of tooth brushing, and use of fluoride supplement. The study protocol was approved by the Khon Kaen University Ethics Committee in Human Research (HE480238). All parents signed informed consent forms, while the school children provided assent.
Clinical examination and collection of saliva
Clinical examinations for dental caries and oral hygiene were performed by one calibrated dentist. Dental caries was determined according to the modified World Health Organization (WHO) diagnostic criteria [19]. Oral hygiene was assessed using the Simplified Oral Hygiene Index (OHI-S) by Greene and Vermillion [20]. Unstimulated whole saliva samples were collected between 9 a.m. and 11 a.m. Saliva from each individual was collected every 1 min by spitting into a disposable polypropylene sterile tube with an adapted disposable cup. Salivary flow rates were determined gravimetrically and expressed in milliliters per minute (mL/min). All saliva samples were immediately placed on ice for transportation. Samples were centrifuged at 4000 rpm for 10 min. Supernatants were aliquoted and stored at −80 °C until the assays were performed.
Assays for measurement of salivary MUC5B and MUC7
Enzyme-linked immunosorbent assay (ELISA) protocols were developed for measurement of MUC5B and MUC7 in human whole saliva. One hundred microliters of diluted saliva (1:200 for MUC5B and 1:10 for MUC7) in coating buffer, carbonate-bicarbonate buffer (pH 9.6), was added to each well. Microtiter plates were kept at 4 °C overnight and then washed three times with 0.05 % Tween 20 in normal saline (NS). Two hundred microliters of 3 % bovine serum albumin (BSA) in phosphate buffer saline (PBS) (pH 7.2) was added to each well for 1 h at 37 °C for blocking nonspecific binding, followed by washing three times with NS. For the determination of salivary MUC5B, 100 μl of diluted mouse antihuman MUC5B antibodies (1:100) [21] in incubation buffer with 2 % skimmed milk was added to each well, followed by washing three times with NS. One hundred microliters of biotin-conjugated goat anti-mouse IgG antibody (1:5000; Zymed Laboratories Inc., San Francisco, CA) in incubation buffer with 2 % skimmed milk was added to each well, followed by incubation for 1 h at 37 °C. After washing three times with NS, 100 μl of streptavidin-conjugated peroxidase (1:10,000; Zymed Laboratories Inc.) in incubation buffer was added to each well, followed by incubation for 1 h at 37 °C. To estimate salivary MUC7, 100 μl of diluted rabbit antihuman MUC7 antibodies (1:100) [22] in incubation buffer with 2 % skimmed milk was added to each well, followed by washing three times with NS. One hundred microliters of biotin-conjugated goat anti-rabbit IgG antibody (1:5000; Zymed Laboratories Inc.) in incubation buffer with 2 % skimmed milk was added to each well, followed by incubation for 1 h at 37 °C. After washing three times with NS, 100 μl of streptavidin-conjugated peroxidase (1:10,000; Zymed Laboratories Inc.) in incubation buffer was added to each well, followed by incubation for 1 h at 37 °C.
After washing three times with NS, 100 μl of freshly prepared substrate solution containing one O-phenylenediamine dihydrochloride (OPD) tablet (Sigma Chemical Co.), 14 μl of 30 % H2O2, and 20 ml of 0.05 M citrate buffer (pH 5.0) was added to each well. Incubation was approximately 20 min to observe for the development of color in the wells. The reaction was stopped by adding 100 μl/well of 2 N H2SO4, and the absorbances were measure on a microtiter plate reader (Sunrise microtiter plate reader; Tecan, Austria) at 492 nm. All saliva samples in the procedures of ELISA were done in triplicate, and the data were calculated from the mean optical density (OD) values of three tests for each sample. Triplicate determinations of each sample were estimated for coefficient of variation (CV). Substrate and H2O2 was used as a blank control, and incubation buffer in place of saliva sample was used as a negative control. An inter-plate saliva sample from one participant was used to compare plate-to-plate absorbance variation, thereby calibrating plate-to-plate discrepancy, accordingly.
Statistical analyses
Characteristics of the study groups were compared using chi-square and t tests. Salivary MUC5B and MUC7 data were analyzed as mean OD values. The Mann-Whitney U test was utilized to assess statistical differences in the levels of salivary mucins between high and low caries-risk groups. Spearman’s rank correlation coefficients were used to determine the correlations between salivary mucin levels and dental caries status. p values <0.05 were considered statistically significant.
Results
Characteristics of study population
Table 1 shows characteristics of the participants according to age groups and dental caries risk. The two investigated groups were similar in regard to demographic characteristics, oral care behaviors, fluoride supplement use, and salivary flow rate. School children with high caries risk had a significantly higher plaque index compared to those with low caries risk (p = 0.02).
Levels of MUC5B and MUC7 in saliva
In the preschool children with deciduous dentition, there were no statistically significant differences in the levels of MUC5B and MUC7 between the high and low caries-risk groups (Figs. 1 and 2). In the school children with mixed dentition, levels of salivary MUC5B were significantly higher in a low caries-risk group than those in a high caries-risk group (p = 0.01). In contrast, levels of salivary MUC7 were significantly lower in a low caries-risk group than those in a high caries-risk group (p = 0.04) (Figs. 1 and 2).
Levels of salivary MUC5B representing as OD values in preschool (aged 4–6 years) and school (aged 9–11 years) children with high and low dental caries risk. The boxes represent the inter-quartile range, with the lower edge and upper edge corresponding to the 25th and 75th percentiles, respectively. The horizontal line within each box represents the median expression level in each group. The circles indicate outliers, and the stars represent extreme outliers. In the school children, salivary MUC5B was significantly higher in a low caries-risk group than that in a high caries-risk group (p = 0.01)
Levels of salivary MUC7 representing as OD values in preschool (aged 4–6 years) and school (aged 9–11 years) children with high and low dental caries risk. The boxes represent the inter-quartile range, with the lower edge and upper edge corresponding to the 25th and 75th percentiles, respectively. The horizontal line within each box represents the median expression level in each group. The circles indicate outliers. In the school children, salivary MUC7 was significantly lower in a low caries-risk group than that in a high caries-risk group (S = 0.04)
Correlations between levels of salivary mucins and dental caries status
In the preschool children, no significant correlations were found between salivary mucins and dental caries status as measured by the numbers of decayed teeth (dt) and decayed surfaces (ds) in deciduous dentition (Table 2). In the school children with mixed dentition, salivary MUC5B levels were negatively correlated with the number of decayed deciduous and permanent teeth (DT + dt; r = −0.29; p = 0.03) and surfaces (r = −0.29; p = 0.03). No significant correlations between MUC7 and dental caries index were demonstrated in the school children (Table 2).
Discussion
In this study, we measured the levels of salivary mucins in preschool and school children with different dental caries status, using an ELISA technique. Preschool children aged between 4 and 6 years represented an oral environment with deciduous dentition, whereas school children aged between 9 and 11 years represented an oral environment with mixed dentition. According to our results, increased MUC5B and decreased MUC7 levels were observed in school children with low caries risk. No differences in salivary MUC5B and MUC7 levels were found between high and low caries-risk groups in preschool children. The present study extended previous observations in young adults with permanent dentition which found the higher salivary levels of MUC5B and MUC7 in a low dental caries-risk group [6]. Collectively, these findings suggested that secretion of salivary mucins in response to dental caries might be influenced by various oral conditions such as changes in oral environments during child growth and tooth development from deciduous to permanent dentition. It should be noted that, in our study, antihuman MUC5B antibody was directed against a Lewis blood group glycan moiety and antihuman MUC7 antibody was directed against a peptide moiety. Therefore, it would be hypothesized that degradation of mucin glycans by bacterial enzymes such as glycohydrolases in the oral environment could be another possible inducer of differences in salivary mucin levels assessed by ELISA.
Several studies reported different patterns of salivary mucin secretion in various age groups [14–17]. In addition, shifts in nutrition from fluids to solids and variations in exposure to pathogenic stimuli such as microorganisms may affect salivary secretions [14, 15]. One previous study demonstrated that decreased salivary MUC7 concentrations were significantly associated with elevated Streptococcus mutans titers in elderly subjects [11]. According to previous and present findings, one may hypothesize that several oral conditions such as aging and tooth development from deciduous to permanent dentition may affect salivary MUC5B and MUC7 secretion in response to dental caries. However, it remains unclear how the regulation of salivary mucin secretion at various oral conditions is affected by factors inducing dental caries such as cariogenic bacteria. Thus, to prove the aforementioned hypothesis, further studies are essential to validate which factors or mechanisms, at various oral conditions, play a major role in regulating salivary mucin expression in response to dental caries.
Regarding the correlations between salivary mucins and dental caries status, one study demonstrated negative correlations between salivary mucins (MUC5B and MUC7) and dental caries index in young adults aged 17–24 years with permanent dentition [6]. In addition, it was reported that changes in salivary proteins such as mucins and antimicrobial peptides during aging were significantly correlated with dental caries prevalence [23]. Our observations are in agreement with the previous studies by demonstrating a negative correlation between salivary MUC5B and the number of decayed teeth/surfaces in school children with mixed dentition. However, no significant correlations were observed between salivary mucin levels (MUC5B and MUC7) and dental caries in preschool children with deciduous dentition. The present data demonstrated that patterns of correlations between salivary mucins and dental caries status were different between deciduous and mixed dentition. Thus, previous and present findings imply that changes in tooth development from deciduous to permanent dentition may affect the association between salivary mucins and dental caries. However, we could not exclude the possibility that other factors such as criteria for establishing dental caries status and different methods for measuring levels of mucins in saliva may result in different outcomes. Therefore, standardization of methods for measurement of salivary mucins at various oral conditions would be of importance to validate MUC5B and MUC7 as caries risk indicators. In addition to salivary MUC5B and MUC7, other mucins such as MUC1 and MUC4 which were produced by minor salivary glands, parotid glands, and buccal epithelial cells [24, 25]. In addition, the expression of soluble forms of MUC1 and MUC4 was demonstrated in human-stimulated parotid secretion [25]. There has been evidence that MUC1 and MUC4 are involved in the physical protection [26, 27]. Therefore, it would be of interest to investigate whether there are any connections among the expression of soluble forms of MUC1 and MUC4 in whole saliva, dental plaque, and dental caries in association with tooth development of deciduous to permanent dentition.
In conclusion, the present study suggests that the patterns of salivary MUC5B and MUC7 expression and the patterns of correlations between dental caries status and salivary mucins were different between preschool children with deciduous dentition and school children with mixed dentition. Taken together, these findings suggest that changes in oral environment from deciduous to mixed dentition may have an effect on the secretion of salivary mucins in response to dental caries. Further studies to investigate whether each type of salivary mucins could have its own functional profile in response to dental caries would be important for validation of salivary mucins as caries risk indicators.
References
Dental Health Division, Department of Health, Ministry of Public health. The 7th national oral health survey in Thailand. [Online] Available from http://dental.anamai.moph.go.th/survey7.pdf. Accessed 19 Jan 2014
Lenander-Lumikari M, Loimaranta V (2000) Saliva and dental caries. Adv Dent Res 14:40–47
Amerongen AV, Veerman EC (2002) Saliva—the defender of the oral cavity. Oral Dis 8:12–22
Van Nieuw Amerongen A, Bolscher JG, Veerman EC (2004) Salivary proteins: protective and diagnostic value in cariology? Caries Res 38:247–253
Dowd FJ (1999) Saliva and dental caries. Dent Clin N Am 43:579–597
Banderas-Tarabay JA, Zacarias-D’Oleire IG, Garduno-Estrada R, Aceves-Luna E, Gonzalez-Begne M (2002) Electrophoretic analysis of whole saliva and prevalence of dental caries. A study in Mexican dental students. Arch Med Res 33:499–505
Tabak LA (1995) In defense of the oral cavity: structure, biosynthesis, and function of salivary mucins. Annu Rev Physiol 57:547–564
Tabak LA (2006) In defense of the oral cavity: the protective role of the salivary secretions. Pediatr Dent 28:110–117
Zalewska A, Zwierz K, Zolkowski K, Gindzienski A (2000) Structure and biosynthesis of human salivary mucins. Acta Biochim Pol 47:1067–1079
Wei GX, Campagna AN, Bobek LA (2006) Effect of MUC7 peptides on the growth of bacteria and on Streptococcus mutans biofilm. J Antimicrob Chemother 57:1100–1109
Baughan LW, Robertello FJ, Sarrett DC, Denny PA, Denny PC (2000) Salivary mucin as related to oral Streptococcus mutans in elderly people. Oral Microbiol Immunol 15:10–14
Reddy MS, Levine MJ, Paranchych W (1993) Low-molecular-mass human salivary mucin, MG2: structure and binding of Pseudomonas aeruginosa. Crit Rev Oral Biol Med 4:315–323
Liu B, Rayment SA, Gyurko C, Oppenheim FG, Offner GD, Troxler RF (2000) The recombinant N-terminal region of human salivary mucin MG2 (MUC7) contains a binding domain for oral Streptococci and exhibits candidacidal activity. Biochem J 1:557–564
Sonesson M, Wickstrom C, Kinnby B, Ericson D, Matsson L (2008) Mucins MUC5B and MUC7 in minor salivary gland secretion of children and adults. Arch Oral Biol 53:523–527
Ruhl S, Rayment SA, Schmalz G, Hiller KA, Troxler RF (2005) Proteins in whole saliva during the first year of infancy. J Dent Res 84:29–34
Denny PC, Denny PA, Klauser DK, Hong SH, Navazesh M, Tabak LA (1991) Age-related changes in mucins from human whole saliva. J Dent Res 70:1320–1327
Navazesh M, Mulligan RA, Kipnis V, Denny PA, Denny PC (1992) Comparison of whole saliva flow rates and mucin concentrations in healthy Caucasian young and aged adults. J Dent Res 71:1275–1278
AAPD (2002) Policy on the use of a caries-risk assessment tool (CAT) for infants, children and adolescents. Pediatr Dent 24:15–17
World Health Organization (1997) Oral health surveys: basic methods. 4th edn. Geneva
Greene JC, Vermillion JR (1964) The simplified oral hygiene index. J Am Dent Assoc 68:7–13
Veerman EC, Bolscher JG, Appelmelk BJ, Bloemena E, van den Berg TK, Nieuw Amerongen AV (1997) A monoclonal antibody directed against high M(r) salivary mucins recognizes the SO3-3Gal beta 1-3GlcNAc moiety of sulfo-Lewis(a): a histochemical survey of human and rat tissue. Glycobiology 7:37–43
Bolscher JG, Groenink J, van der Kwaak JS, van den Keijbus PA, van’t Hof W, Veerman EC, Nieuw Amerongen AV (1999) Detection and quantification of MUC7 in submandibular, sublingual, palatine, and labial saliva by anti-peptide antiserum. J Dent Res 78:1362–1369
Mungia R, Cano SM, Johnson DA, Dang H, Brown JP (2008) Interaction of age and specific saliva component output on caries. Aging Clin Exp Res 20:503–508
Offner GD, Troxler RF (2000) Heterogeneity of high-molecular-weight human salivary mucins. Adv Dent Res 14:69–75
Liu B, Lague JR, Nunes DP, Toselli P, Oppenheim FG, Soares RV, Troxler RF, Offner GD (2002) Expression of membrane-associated mucins MUC1 and MUC4 in major human salivary glands. J Histochem Cytochem 50:811–820
Chang WI, Chang JY, Kim YY, Lee G, Kho HS (2011) MUC1 expression in the oral mucosal epithelial cells of the elderly. Arch Oral Biol 56:885–890
Chaturvedi P, Singh AP, Batra SK (2008) Structure, evolution, and biology of the MUC4 mucin. FASEB J 22:966–981
Acknowledgments
The authors would like to thank all children and their parents for participation in the study. We also thank teachers in Khon Kaen University’s Demonstration School for their assistance. We would like to thank Dr. Jan GM Bolscher and Dr. Enno CI Veerman for providing primary antibodies against MUC5B and MUC7. This work was supported by a research grant from Khon Kaen University, Thailand. JGMB and ECIV are supported by a grant from the University of Amsterdam for research into the focal point “Oral infections and inflammation.”
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Angwaravong, O., Pitiphat, W., Bolscher, J.G.M. et al. Evaluation of salivary mucins in children with deciduous and mixed dentition: comparative analysis between high and low caries-risk groups. Clin Oral Invest 19, 1931–1937 (2015). https://doi.org/10.1007/s00784-015-1428-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-015-1428-1