Abstract
Objectives
This practice-based study evaluated the clinical performance and risk factors for biological and technical complications with conventionally luted zirconia crowns.
Materials and methods
Sixty-eight patients (39 female) with a total of 323 restorations placed on 219 vital teeth, 69 endodontically treated teeth (ETT), and 41 implants (incisors, 96; premolars, 89; molars, 138; observational period, 79.7 ± 14.2 months) underwent a clinical follow-up examination and were included in the study. Time-dependent survival (in situ), success (event free), and veneering ceramic fracture (VCF) rates were calculated and analyzed relative to the following risk factors: smoking status, location of the crown, and type of abutment.
Results
Fifty-three complete failures were recorded. A significant influence of the abutment type on survival could be detected (p = 0.033): ETT demonstrated a significantly (p = 0.029) lower 7-year survival rate (73.8 %, 95 % confidence interval [95 % CI] 0.600–0.876) than crowns placed on implants (90.0 %, 95 % CI 0.814–0.990). The success rate of the crowns was significantly influenced by the location of the restoration (p = 0.0058). A total of 75.6 % (95 % CI 0.648–0.864) of the anterior crowns remained event free, compared to 50.4 % (95 % CI 0.388–0.621) of the molar crowns. Furthermore, the location of the crowns affected the VCF rate (p = 0.018, event-free anterior teeth 95.2 % (95 % CI 0.880–1), event-free molars 80.9 % (95 % CI 0.706–0.913)).
Conclusions
Survival and success rates were significantly influenced by the type of abutment and the location of the restoration.
Clinical relevance
More complete failures should be expected for crowns placed on ETT, while crowns on molars demonstrated more biological and technical complications than anterior zirconia crowns.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past decade, zirconia (yttrium-containing tetragonal zirconia polycrystalline = Y-TZP) has been introduced to the dental field, along with new computer-aided design/computer-aided manufacturing (CAD/CAM) processing technologies for the fabrication of fixed dental prostheses (FDPs) and crowns [1]. The majority of early stage clinical studies were focused on the evaluation of tooth-supported Y-TZP-based FPDs [2]. Although these studies reported framework survival rates exceeding 90 % for observational periods of up to 10 years, a high incidence of veneering ceramic fractures (VCFs), ranging from 0 to 54 %, within the first 3 years of clinical service was documented, thus presenting a serious complication for this type of restoration [1–3]. More recently published clinical trials [4–10] have also evaluated the clinical performance of tooth- and implant-supported single Y-TZP crowns. In a systematic review of 16 studies, including 830 tooth-supported and 301 implant-supported Y-TZP-based crowns, cumulative survival rates of 95.9 % for tooth-supported crowns and 97.1 % for implant-supported crowns were determined [11] which is comparable with the survival rates published for metal-ceramic crowns [12]. In another systematic review [13], the survival rates of Y-TZP crowns ranged from 92.7 to 100 % for observational periods of 24 to 39 months. Nevertheless, VCFs were reported as frequent technical complications in both systematic reviews [11, 13], with incidences of at least 13.2 % for observational periods of 2–3 years [4, 6, 14–16]. Various reasons related to both, the material and its processing, have been suggested to cause fractures of the veneering material: mismatching of the coefficient of thermal expansion between the veneering porcelain and the zirconia substructure, aging, the veneering method, missing anatomical design of the framework, residual stress due to the low thermal conductivity of zirconia, and user-related effects (e.g., occlusal adjustments) [1, 17–21]. Apart from factors related to the material and its processing, the rate of technical complications can be influenced by patient- and restoration-related risk factors. Patient-specific factors, such as occlusal relationship, parafunctional habits, and the use of a night guard, have been identified as relevant risk factors that can significantly affect the veneering ceramic fracture rate of Y-TZP restorations [22, 23]. Restoration-specific risk factors, such as the type of abutment (i.e., a vital tooth, an endodontically treated tooth, or an implant-based restoration) and its location (anterior, premolar, or molar), have been demonstrated to influence the survival (restoration remaining in function) and success (intervention-free survival) of metal-ceramic and all-ceramic crowns [12, 24–28]. To the authors’ best knowledge, there is no information in the literature regarding the associations of these types of risk factors with the survival, success, and technical complication rates of Y-TZP crowns for extended observational periods of more than 5 years.
The present practice-based, retrospective study aimed to evaluate patient- (smoking status) and restoration-specific (abutment type, location) risk factors for the survival and technical, as well as biological, complication rates with Y-TZP single crowns placed in a private practice.
Materials and methods
Patient selection
Eighty-seven patients who were treated in a private practice from February 2003 to December 2006 and who received conventionally luted zirconia crowns fabricated with a single type of CAM system (Cercon Smart Ceramics, DeguDent, Germany) and attended a maintenance program (prophylaxis or supportive periodontal therapy) on a regular basis were identified. A total of 395 restorations were placed using either zinc phosphate or glass ionomer cements of different brands. These patients were approached during their annual maintenance appointments and were asked to participate in this retrospective study after having received information about the aims and the course of the study and the methods of data collection. Patients who met the following criteria were included:
-
Participation in at least annual (±2 months) clinical examinations;
-
Antagonistic natural teeth or fixed prosthetic restorations;
-
Complete medical information, including smoking status; and
-
Complete documentation of crown-related complications or failures.
Patients with one or more of the following diagnoses were excluded from participation:
-
Clinical symptoms of bruxism (severe occlusal parafunction with wear facets and facial pain, both self-reported); or
-
Aggressive periodontitis or untreated chronic periodontitis.
The Ethics Committee of the University of Göttingen approved this study (application no. 4/8/12), and all of the subjects provided informed consent. The recommendations for strengthening the reporting of observational studies in epidemiology (STROBE) were followed.
Clinical approach
All of the clinical treatments were performed by an experienced clinician (S.R.) in a private practice in Germany. All of the patients received oral hygiene instructions and professional tooth cleaning or systematic periodontal treatment prior to prosthetic treatment. All vital abutments received an adhesively placed composite buildup. Non-vital teeth were restored with a direct composite buildup to ensure the long-term retention of the restorations and, in cases of insufficient natural tooth structure, with a prefabricated titanium or fiberglass root post. The abutment teeth were prepared with a 0.8- to 1.0-mm heavy chamfer and an axial taper of 4° to 6°. The occlusal reduction was approximately 1.5 mm. Single-tooth implants were restored using prefabricated titanium abutments. All impressions were obtained with polyvinylsiloxane or polyether materials. Clinical fit of the veneered crowns was checked prior to cementation using a dental probe (86-157-001, Ustomed, Tuttlingen, Germany). Six crowns had to be remade due to insufficient fitting quality. The acceptable restorations were finally luted with zinc phosphate or glass ionomer cements of different brands. The preferred occlusal concepts were a canine-protected articulation or a group functioning on the canines and premolars.
Laboratory techniques
All of the zirconia frameworks were produced by a CAM system (Cercon Smart Ceramics, DeguDent GmbH, Germany), which was introduced to the German market in 2001. During the production process, a manually fabricated wax pattern of the framework was laser scanned to acquire the necessary data for a three-dimensional virtual model. Prior to milling the frameworks from presintered zirconia (Cercon Base, DeguDent Hanau, Germany), the acquired data were increased by ~30 % to compensate for shrinkage during sintering. Finally, the frameworks were sintered to full density at a temperature of 1350 °C for 6 h.
The minimum framework thickness was 0.4 mm. The sintered frameworks were adapted until the best possible fit was achieved. Adaptation was performed by an experienced technician under ×4 magnification according to the literature [29]. All of the Y-TZP restorations were veneered with a manual layering technique, using a ceramic material (Cercon Ceram S or Cercon Ceram-Kiss, DeguDent GmbH, Germany) with a TEC (thermal expansion coefficient) adapted for the veneering of zirconia frameworks (9.5 μm/m*K).
Data collection
Using patient records, the patients were evaluated according to the following parameters: age (at crown placement), sex, smoking status, crown location (according to the FDI scheme), abutment type (vital tooth, endodontically treated tooth, implant), date of crown placement, and observation period.
All of the included patients attended at least an annual clinical examination that was completed during prophylaxis or SPT. The clinical examinations were performed by a skilled dentist (not the clinician who placed the restorations), who was trained to use the criteria for survival and success. The following parameters were assessed for all of the restorations and were documented in the patients’ records: restoration in situ, decementation (mobility), fracture of the framework, and chipping of the ceramic veneer. Tooth-based restorations were evaluated for loss of vitality, secondary caries, need for periodontal treatment, and endodontic failures. Implant-based restorations were assessed for technical complications of the implant components (implant or abutment fracture, screw loosening) and for peri-implantitis.
Statistical analysis
Information regarding the survival and success of the reconstructions was used for the statistical evaluation. Survival was defined as the reconstruction remaining in situ at the follow-up examination visit, without presenting an absolute failure (i.e., the in situ criterion) [3, 12]. Absolute failure was defined as a clinically unacceptable fracture of the restoration or a biological event (caries, tooth fracture, periodontal reason) that required replacement of the entire restoration or extraction of the tooth [3]. The survival time of a restoration was defined as the period between the day of cementation and either the final follow-up appointment or, in the case of a failure, the appointment scheduled to address the failure, as documented in the patient’s file. Success was defined as a reconstruction that remained unchanged and that did not require any intervention to maintain function during the entire observational period [3, 12]. Necessary interventions to maintain function were divided into technical complications (minor chipping of the ceramic, recementation of a debonded but intact restoration) and biological complications (caries, endodontic treatments, periodontal interventions). The survival (in situ criterion) and success (intervention-free) rates of the restorations and the ceramic veneers (no defects) were calculated using Kaplan-Meier plots. The location of the restoration (anterior/premolar/molar), the type of abutment (vital tooth, endodontically treated tooth, implant), and smoking status were included as factors when analyzing the time-dependent survival and success rates by Cox regression analysis. Different observations within a single patient (several crowns per patient) were dependent. This dependence was allowed for by adjusted variance estimation in the Cox regression model. Thus, for the data analysis, a marginal model was applied [30]. Multiple Cox regression analysis was performed to analyze the influence of the different factors on the success and survival rates. In cases of significance, post hoc tests were performed to compare the different factor levels with a pairwise procedure. A level of significance of <5 % was accepted to determine a statistically significant influence; due to the closed testing procedure, an adjustment for multiple comparisons was not necessary in the post hoc tests. Statistical analyses were performed using the R programming environment (version 2.14.1, www.r-project.org).
Results
Patients
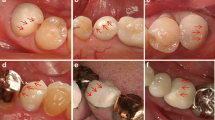
Nineteen patients with 72 restorations did not fulfill the inclusion criteria, met the exclusion criteria, or declined to participate in the study. Their data were excluded from further statistical evaluation (Table 1). Sixty-eight patients (39 female/29 male) with a total of 323 restorations (anterior crowns, 96; premolar crowns, 89; molar crowns, 138), placed on 221 vital and 63 endodontically treated teeth and 41 implants, attended clinical follow-ups between January 2011 and April 2012, and were included in the study. The age of the subjects ranged from 25 to 74 years old (mean age 51.0 ± 9.2 years old). The patients received up to 10 restorations. The mean observational period was 79.7 ± 12.2 months. The minimum observational period was 48.9 months (maximum 116.3 months). During this period, 52 of the 323 crowns failed and had to be replaced. The most frequent reason for crown failure was extensive fracturing of the veneering ceramics (n = 28) (Fig. 1), followed by endodontic reasons (n = 15) (Table 2). No fracture of a zirconia framework was detected over the entire observational period.
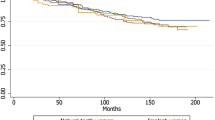
Crown survival rates
The overall 7-year survival rate was 82.4 % (95 % confidence interval [95 % CI] 0.760, 0.888). A statistically significant influence of type of abutment (vital tooth, endodontic tooth, implant) on the survival rate was detected (multivariate analysis, p = 0.033). Crowns placed on endodontically treated teeth demonstrated a significantly lower 7-year survival rate (73.8 % [95 % CI 0.600–0.876]) than crowns placed on implants (7-year survival rate 90.0 % [95 % CI 0.814–0.990]) (pairwise comparison, p = 0.029) (Table 3). Crowns placed on vital teeth demonstrated a survival rate of 83.5 % (95 % CI 0.759–0.911) after an observational period of 7 years (Fig. 2). Neither the location of the restoration (anterior, premolar, molar) (p = 0.270) nor smoking status (p = 0.260) significantly affected the survival rate.
Crown success rates
Sixty-four restorations required clinical interventions to maintain their function over the entire observational period (Table 4). The most frequent technical complication (n = 31) was loss of retention of a conventionally luted zirconia crown. All of the restorations could be recemented using an adhesive protocol, with a self-etching primer and bonding agent and an auto-curing composite (Panavia 21, Kuraray Europa GmbH, Hattersheim, Germany). Veneering ceramic fractures requiring a clinical intervention to maintain function were observed in 12 restorations. Nine events were considered minor chippings, with an affected surface area of <2 mm2. These defects were polished intraorally. Three chippings that exposed the zirconia core required repair with a composite material. Endodontic treatment was necessary for 19 abutment teeth. The access cavity was sealed with a composite restoration, and all of the crowns could remain in function. The overall 7-year success rate (event-free restoration) was 62.5 % (95 % CI 0.545–0.7042). Multivariate analysis revealed a significant effect of the independent variable location of the restoration on the success rate (p = 0.0058). The success rate of anterior crowns (75.6 % [95 % CI 0.648–0.864]) was significantly higher than the success rate of molar crowns (50.4 % [95 % CI 0.388–0.621]) (pairwise comparison, p = 0.013) (Table 5). Of the crowns placed on premolars, 68.3 % (95 % CI 0.564–0.803) remained event free over the 7-year observational period and did not demonstrate significant differences from the success rates of anterior or molar crowns.
Ceramic fracture rates
During the entire observational period, 40 veneering ceramic fractures were observed, resulting in a 7-year incidence of 12.4 %. Twenty eight of these fractures required replacement of the restoration, while the function of 12 restorations could be maintained by intraoral polishing or repair with a composite restoration.
A separate time to event analysis regarding ceramic fractures revealed that 95.2 % (95 % CI 0.88–1) of the ceramic veneers of anterior crowns were intact, whereas a lower success rate of 80.9 % (95 % CI 0.706–0.913) was calculated for the ceramic veneers of molar crowns (Fig. 3) A statistically significant difference between these two groups could be detected (pairwise comparison, p = 0.034) (Table 6).
Discussion
The 7-year results of this retrospective study revealed survival rates ranging from 73.85 % for crowns placed on endodontically treated teeth to 90 % for implant-based crowns. These results were not in agreement with the findings of two systematic reviews, which estimated 3-year cumulative survival rates of 100 % for anterior and 95.5 % for posterior crowns [13], as well as calculated 5-year survival rates of 95.9 % for tooth-based zirconia crowns and 97.1 % for implant-based restorations [11]. This finding might be explained as follows. The reported estimated 5-year survival rates were calculated from clinical trials with mean observational periods ranging from 2 to 5 years. The calculation was based on a constant annual failure rate. If the failure rate increased, this calculation resulted in overestimation of the survival rate. The increase in the annual failure rate with prolonged observational periods has already been demonstrated for zirconia FPDs [31], thus emphasizing the need for clinical studies with prolonged observational periods to draw reliable conclusions regarding clinical performance [11, 13]. In the present study, none of the Y-TZP frameworks fractured during the entire observational period. This result is in good accordance with the findings of a systematic review that included 16 clinical studies with 1131 Y-TZP crowns, in which only three events of core fractures were reported [11]. As in other clinical studies, extended veneering ceramic fractures represented the most frequent reason for failure, confirming the importance of these findings for clinical long-term success [11, 13] in the early stages of Y-TZP processing. In addition, knowledge regarding the prevention of ceramic material fractures, by using either a pressable veneering ceramic [21] or a more pronounced core design and applying prolonged cooling periods to decrease internal stresses, has increased and is now clinically applied. However, this information was not available during the study period, which might explain the higher survival rates reported in clinical trials that have been published more recently [6, 7, 9, 20]. The type of abutment (vital tooth/endodontically treated tooth/implant) showed a significant effect on the survival rate. Endodontic failures represented the most frequent biological complications in the present study, resulting in a reduced survival rate of 73.85 % after a mean observational period of 7 years. This finding agrees with the findings of other clinical trials reporting on all-ceramic and metal-ceramic crowns [12, 27], which have also reported reduced survival rates for crowns on endodontically treated teeth.
Nevertheless, it must be stated that the low survival rate of Y-TZP crowns in the present study was mainly attributable to technical complications (veneering ceramic fractures). This rate represents a clear difference from the data published for porcelain-fused-to-metal (PFM) crowns. For PFM crowns, a cumulative survival rate of 95.6 % (CI 92.4–97.5) after 5 years was estimated by systematically reviewing six studies including a total of 1765 restorations; therefore, the clinical performance of Y-TZP crowns fabricated in the early stages of Y-TZP processing did reach the level of PFM crowns [12].
The success rate of the crowns (intervention-free survival) was significantly influenced by the location of the restoration, with molar crowns having more biological and technical complications (success rate 50.4 %) than crowns placed on anterior teeth (success rate 75.6 % [95 % CI 0.648–0.864]). This result is in accordance with the findings of systematic reviews [12, 24, 28] reporting high complication rates for all-ceramic crowns placed in posterior areas. Therefore, it should be stated that zirconia crowns fabricated in the early stages of Y-TZP processing did not overcome the limitations of other dental ceramics regarding their usage in posterior areas. The most frequent reason for a clinical intervention (31 of 64 cases) was the need for recementation of a crown, resulting in a 7-year incidence of 9.6 %. Based on the findings of a systematic review, loss of retention is a rare technical complication with PFM crowns; an annual rate of 0.13 % resulted in a cumulative complication rate of 0.7 % after 5 years [12]. The high complication rate observed in the present study might be explained by the following specific aspects. The present study used an early stage CAM-processing technique that was introduced in 2001. An in vitro study compared the internal fit of porcelain-fused-to-metal and zirconia-based FPDs, made with the same system as that used in the present study. The results revealed reduced internal fit and therefore a thicker cement layer among the zirconia FPDs, compared to the cast metal frameworks [32]. This is supported by another in vitro study comparing the fitting quality of the early stage CAM system (Cercon) used in this study with other CAD/CAM systems. Compared to other CAD/CAM systems, restorations produced with the CAM system demonstrated a reduced internal and marginal fitting quality compared to other marginal and internal fits of zirconia restorations [29]. The high rate of retention loss could be explained by the reduced internal fitting accuracy of the zirconia framework. In addition, improved CAD/CAM techniques have improved the quality of zirconia restorations with regard to internal and marginal fitting accuracy [1].
A second possible explanation can be observed in the luting agents used in the present study. A loss of retention has been reported in clinical studies of the performance of zirconia FPDs, particularly when zinc phosphate cements have been used as luting agents [14, 31]. Zinc phosphate and glass ionomer cements as luting agents have demonstrated reduced retentive strength under in vitro conditions, while resin-modified glass ionomer cements and composite cements have demonstrated improved retentive characteristics [33]. In a prospective clinical trial using an improved CAD/CAM technology and a resin-modified glass ionomer cement, none of the evaluated Y-TZP molar crowns showed loss of retention [20]. These findings might result in the conclusion that with improved manufacturing technology and the use of luting agents with improved retentive capacity, the high complication rate of the present study would be substantially reduced.
Nineteen of the 219 reevaluated restorations placed on vital teeth required endodontic treatment during the entire observational period, resulting in a 7-year incidence of 8.6 %. This finding agrees with those of Ortrop et al. (2012) [14], who reported an incidence of 6 % for endodontic treatments after 3 years for zirconia-based single crowns, with all of the endodontic problems occurring in posterior teeth. Both results conflict with the findings of other studies. In a systematic review, the incidence of loss of vitality after placement of an all-ceramic crown was calculated to be 2.1 % within a 5-year period [12]. This observation is also supported by the findings of a retrospective, long-term evaluation of 1335 adhesively luted all-ceramic restorations. In that study, the incidence of endodontic treatment was 2.5 % after a mean observational period of 8.5 years [27]. A possible explanation for the increased rate of biological complications can be observed in the preparation guidelines provided during the early phase of the clinical usage of Y-TZP. To ensure complete data acquisition for the entire preparation, a more conical design with a preparation angle of 4° to 6° was recommended, which is greater than the standard preparation angle of 2° to 3° recommended for metal-ceramic crowns. This more conical design led to increased substance loss and a more aggressive preparation design, thus possibly increasing the risk of biological complications. In addition, because of improved scanning technology, manufacturers have modified the preparation guidelines, allowing for preparations with less conical designs. This aspect might be important in decreasing the risk of biological complications. As in other clinical studies evaluating Y-TZP crowns, secondary caries was a rare complication in the present study [11, 13].
The annual chipping rate for metal-ceramic crowns, based on the findings of a systematic review [12], was 1.17 % including anterior and posterior crowns, which translated to a 5-year rate of ceramic chipping of 5.7 %. In the present study, crowns placed on anterior teeth or implants showed an annual ceramic fracture rate of 0.69 %, while molar crowns demonstrated a significantly higher (p = 0.034) annual ceramic failure rate of 2.73 %. This finding demonstrated that in the early stages of Y-TZP processing and clinical application, fractures of the veneering ceramic were highly relevant for crowns placed on molars, while for anterior restorations, a ceramic fracture complication rate comparable to that of PFM restorations was observed [12].
The present study was limited by all of the restorations having been placed by a single operator. This fact limits the potential generalization of the results because operator-related effects on clinical performance could not be evaluated. Furthermore, no control group with conventionally cemented PFM crowns was included.
When interpreting the results of the present study, the inherent limitations of a retrospective study should be considered; a prospective, randomized clinical trial would have more power. A typical problem encountered in retrospective studies is the availability of analyzable, consistent data; however, this limitation did not apply to the present retrospective study, because the clinical findings have been recorded in the same dental practice since the beginning of 2001, according to a standardized procedure. It can therefore be assumed that the recorded data were representative and comparable.
Moreover, it is worth mentioning that, in the present study, probable bruxists (severe occlusal parafunction with wear facets and facial pain, both self-reported) were excluded. However, it must be stated that identification of bruxists is challenging because a definitive diagnosis requires polysomnography [23]. Thus, it remains unclear how many bruxists were included in the present study. Patients with undetected bruxism might have influenced the results of the present study, resulting in lower survival and success rates than those demonstrated in other clinical studies [22, 27].
Despite these limitations, this study can contribute to the further evaluation of all-ceramic restorations because of its prolonged mean observational period of more than 5 years and because the data were collected under the typical conditions of a private practice. Moreover, the associations between the potential risk factors type of abutment and location of the restoration and the survival and success of Y-TZP crowns have not yet been concisely presented. This information can be helpful for a detailed evaluation of the long-term prognoses of all-ceramic restorations and for the planning of the necessary future long-term, prospective clinical trials.
Conclusion
Within the limitations of this study, the following conclusions can be drawn.
-
The 7-year survival rate of Y-TZP crowns, produced with an early stage CAM system, demonstrated inferior survival and success rates, compared to the survival and success rates published for PFM crowns. The clinical performance was compromised by increased technical (VCFs and loss of retention) and biological (loss of vitality) complication rates.
-
The type of abutment demonstrated a significant influence on the survival rates of Y-TZP crowns, with crowns placed on endodontically treated teeth being at significantly greater risk for complete failure than implant-based restorations.
-
The success rate (intervention-free survival) was significantly influenced by the location, with crowns placed in the molar area showing more biological and technical complications than anterior crowns.
Ceramic material fractures were also significantly influenced by location, with molar crowns demonstrating significantly greater risk for these fractures than anterior crowns.
References
Miyazaki T, Nakamura T, Matsumura H, Ban S, Kobayashi T (2009) Current status of zirconia restoration. J Prosthodont Res 57(4):236–261
Raigrodski AJ, Hillstead MB, Meng GK, Chung KH (2012) Survival and complications of zirconia-based fixed dental prostheses: a systematic review. J Prosthet Dent 107(3):170–177
Anusavice KJ (2012) Standardizing failure, success, and survival decisions in clinical studies of ceramic and metal-ceramic fixed dental prostheses. Dent Mater 28(1):102–111
Groten M, Huttig F (2010) The performance of zirconium dioxide crowns: a clinical follow-up. Int J Prosthodont 23:429–431
Schmitt J, Wichmann M, Holst S, Reich S (2010) Restoring severely compromised anterior teeth with zirconia crowns and feather-edged margin preparations: a 3-year follow-up of a prospective clinical trial. Int J Prosthodont 23(2):107–109
Tartaglia GM, Sidoti E, Sforza C (2011) A 3-year follow-up study of all-ceramic single and multiple crowns performed in a private practice: a prospective case series. Clinics (Sao Paulo) 66:2063–2070
Poggio CE, Dosoli R, Ercoli C (2012) A retrospective analysis of 102 zirconia single crowns with knife-edge margins. J Prosthet Dent 107(5):316–321
Hosseini M, Worsaae N, Schiødt M, Gotfredsen K (2013) A 3-year prospective study of implant-supported, single-tooth restorations of all-ceramic and metal-ceramic materials in patients with tooth agenesis. Clin Oral Implants Res 24(10):1078–1087
Monaco C, Caldari M, Scotti R, AIOP Clinical Research Group (2013) Clinical evaluation of 1,132 zirconia-based single crowns: a retrospective cohort study from the AIOP clinical research group. Int J Prosthodont 26(5):435–442
Ozer F, Mante FK, Chiche G, Saleh N, Takeichi T, Blatz MB (2014) A retrospective survey on long-term survival of posterior zirconia and porcelain-fused-to-metal crowns in private practice. Quintessence Int 45(1):31–38
Larsson C, Wennerberg A (2014) The clinical success of zirconia-based crowns: a systematic review. Int J Prosthodont 27(1):33–43
Pjetursson BE, Sailer I, Zwahlen M, Hämmerle CH (2007) A systematic review of the survival and complication rates of all-ceramic and metal-ceramic reconstructions after an observation period of at least 3 years. Part I: single crowns. Clin Oral Implants Res 18(Suppl 3):73–85
Takeichi T, Katsoulis J, Blatz MB (2013) Clinical outcome of single porcelain-fused-to-zirconium dioxide crowns: a systematic review. J Prosthet Dent 110(6):455–461
Ortorp A, Kihl ML, Carlsson GE (2012) A 5-year retrospective study of survival of zirconia single crowns fitted in a private clinical setting. J Dent 40:527–530
Schwarz S, Schröder C, Hassel A, Bömicke W, Rammelsberg P (2012) Survival and chipping of zirconia-based and metal-ceramic implant-supported single crowns. Clin Implant Dent Relat Res 14(Suppl 1):e119–e125
Kimmich M, Stappert CF (2013) Intraoral treatment of veneering porcelain chipping of fixed dental restorations: a review and clinical application. J Am Dent Assoc 144(1):31–44
Guess PC, Bonfante EA, Silva NR, Coelho PG, Thompson VP (2013) Effect of core design and veneering technique on damage and reliability of Y-TZP-supported crowns. Dent Mater 29(3):307–316
Preis V, Letsch C, Handel G, Behr M, Schneider-Feyrer S, Rosentritt M (2013) Influence of substructure design, veneer application technique, and firing regime on the in vitro performance of molar zirconia crowns. Dent Mater 29(7):e113–e121
Belli R, Frankenberger R, Appelt A, Schmitt J, Baratieri LN, Greil P, Lohbauer U (2013) Thermal-induced residual stresses affect the lifetime of zirconia-veneer crowns. Dent Mater 29(2):181–190
Rinke S, Schäfer S, Lange K, Gersdorff N, Roediger M (2013) Practice-based clinical evaluation of metal-ceramic and zirconia molar crowns: 3-year results. J Oral Rehabil 40(3):228–237
Beuer F, Edelhoff D, Gernet W, Sorensen JA (2009) Three-year clinical prospective evaluation of zirconia-based posterior fixed dental prostheses (FDPs). Clin Oral Investig 13(4):445–451
Koenig V, Vanheusden AJ, Le Goff SO, Mainjot AK (2013) Clinical risk factors related to failures with zirconia-based restorations: an up to 9-year retrospective study. J Dent 41(12):1164–1174
Schmitter M, Boemicke W, Stober T (2014) Bruxism in prospective studies of veneered zirconia restorations—a systematic review. Int J Prosthodont 27(2):127–133
Heintze SD, Rousson V (2010) Fracture rates of IPS Empress all-ceramic crowns—a systematic review. Int J Prosthodont 23(2):129–133
Land MF, Hopp CD (2010) Survival rates of all-ceramic systems differ by clinical indication and fabrication method. J Evid Based Dent Pract 10(1):37–38
Jung RE, Zembic A, Pjetursson BE, Zwahlen M, Thoma DS (2012) Systematic review of the survival rate and the incidence of biological, technical, and aesthetic complications of single crowns on implants reported in longitudinal studies with a mean follow-up of 5 years. Clin Oral Implants Res 23(Suppl 6):2–21
Beier US, Kapferer I, Dumfahrt H (2012) Clinical long-term evaluation and failure characteristics of 1,335 all-ceramic restorations. Int J Prosthodont 25(1):70–78
Wang X, Fan D, Swain MV, Zhao K (2012) A systematic review of all-ceramic crowns: clinical fracture rates in relation to restored tooth type. Int J Prosthodont 25(5):441–450
Beuer F, Aggstaller H, Edelhoff D, Gernet W, Sorensen J (2009) Marginal and internal fits of fixed dental prostheses zirconia retainers. Dent Mater 25(1):94–102
Gerds TA, Qvist V, Strub JR, Pipper CB, Scheike TH, Keiding N (2009) Failure time analysis. In: Lesaffre E, Feine J, LeRoux B (eds) Statistical and methodological aspects of oral health research. John Wiley and Sons, West Sussex, pp 259–277
Rinke S, Gersdorff N, Lange K, Roediger M (2013) Prospective evaluation of zirconia posterior fixed partial dentures: 7-year clinical results. Int J Prosthodont 26(2):164–171
Wettstein F, Sailer I, Roos M, Hämmerle CH (2008) Clinical study of the internal gaps of zirconia and metal frameworks for fixed partial dentures. Eur J Oral Sci 116(3):272–279
Ernst CP, Cohnen U, Stender E, Willershausen B (2005) In vitro retentive strength of zirconium oxide ceramic crowns using different luting agents. J Prosthet Dent 93(6):551–558
Acknowledgments
We thank Katrin Rinke for the critical reading and language editing of the manuscript. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
Sven Rinke has received lecture fees from DeguDent GmbH, Hanau, Germany. Katharina Lange, Matthias Roediger, and Nikolaus Gersdorff declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rinke, S., Lange, K., Roediger, M. et al. Risk factors for technical and biological complications with zirconia single crowns. Clin Oral Invest 19, 1999–2006 (2015). https://doi.org/10.1007/s00784-015-1410-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-015-1410-y