Abstract
Objectives
The aims of the study were to use cone beam computed tomography (CBCT) images of nasopalatine duct cysts (NPDC) and to calculate the diameter, surface area, and 3D-volume using a custom-made software program. Furthermore, any associations of dimensions of NPDC with age, gender, presence/absence of maxillary incisors/canines (MI/MC), endodontic treatment of MI/MC, presenting symptoms, and postoperative complications were evaluated.
Material and Methods
The study comprised 40 patients with a histopathologically confirmed NPDC. On preoperative CBCT scans, curves delineating the cystic borders were drawn in all planes and the widest diameter (in millimeter), surface area (in square millimeter), and volume (in cubic millimeter) were calculated.
Results
The overall mean cyst diameter was 15 mm (range 7–47 mm), the mean cyst surface area 566 mm2 (84–4,516 mm2), and the mean cyst volume 1,735 mm3 (65–25,350 mm3). For 22 randomly allocated cases, a second measurement resulted in a mean absolute aberration of ±4.2 % for the volume, ±2.8 % for the surface, and ±4.9 % for the diameter. A statistically significant association was found for the CBCT determined cyst measurements and the need for preoperative endodontic treatment to MI/MC and for postoperative complications.
Conclusion
In the hands of a single experienced operator, the novel software exhibited high repeatability for measurements of cyst dimensions. Further studies are needed to assess the application of this tool for dimensional analysis of different jaw cysts and lesions including treatment planning.
Clinical relevance
Accurate radiographic information of the bone volume lost (osteolysis) due to expansion of a cystic lesion in three dimensions could help in personalized treatment planning.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The nasopalatine duct cyst (NPDC) is the most frequently encountered non-odontogenic cyst of the jaws [1]. It is a developmental cyst of the midline maxilla, most often within or at the opening of the nasopalatine canal [2]. The reported frequency of NPDC varies between 1 and 11.6 % of all jaw cysts [2–4]. It has been suggested that NPDCs arise from proliferation of epithelial remnants of the embryologic nasopalatine duct [2, 4, 5]. However, the exact cause and pathogenesis remain unknown. The literature suggests (1) any stimulation of the remnant epithelial cells within the nasopalatine canal by any irritation, due to localized trauma or infections [6–8] and (2) spontaneous proliferation [9, 10]. The NPDC appears in both genders at all ages, but is more frequently seen in men [2, 4, 11–14] and in the age range of 30 to 60 years [2, 12, 14]. Symptoms like a buccal/palatal swelling or a sinus tract visible in an intraoral location are reported in close to half of the patients [5, 12, 14]. Pain, probably due to compression of sensory endings of the nasopalatine nerve in the anterior maxilla, is also described, but is neither frequent nor considered to be a typical feature of NPDCs [10, 14]. Thus, some NPDCs are diagnosed incidentally at dental checkups during routine radiographic examinations. On two-dimensional (2D) radiographs, NPDCs often mimic other disease conditions found in the anterior maxilla such as apical periodontitis or radicular cysts, partly due to superimposition of structures in these images [15, 16].
Cone beam computed tomography (CBCT) allows an exact three-dimensional (3D) radiological image analysis of the localisation and extension of bony defects (osteolysis) in the jaws [17]. When using a small dentoalveolar field of view (FOV), a lower effective dose is applied than when using a large maxillofacial FOV or cross-sectional imaging with computed tomography (CT) [18, 19]. Linear measurements on CBCT images are possible in all three planes and directions and are employed in routine practice today. However, no established method of calculating the volume of a bony radiolucency like that of a cyst is available for routine application. Morphometry and volumetric analysis of cystic cavities could have advantages for diagnosis, treatment planning, assessment of prognosis prior to surgical intervention, and also in measuring bone healing and monitoring treatment outcomes.
The objective of the present study was to calculate the volume, widest diameter, and surface area of NPDCs on preoperative CBCT images, using a newly developed software package. Furthermore, utilizing retrospective clinical information any possible associations of the cyst dimensions to age, gender, and presence/absence of maxillary anterior teeth and endodontic treatment were systematically analyzed. Additionally, a possible correlation between the cysts’ dimensions and presenting symptoms and postoperative complications was evaluated.
Materials and methods
Data from 790 patients with histopathologically confirmed jaw cysts treated surgically at the Department of Oral Surgery and Stomatology of the University of Bern during the period of January 2005 to October 2013 were initially eligible. In the present study, only NPDCs confirmed by microscopy by an experienced pathologist were included. Essential histopathological features included the presence of multiple epithelial cell types, e.g., respiratory, cuboid, and squamous epithelium lining the cystic cavity [2]. Furthermore, a preoperative CBCT (3D Accuitomo 80/170, Morita Corp, Kyoto, Japan) had to be available. Based on the final diagnosis and availability of a CBCT, a total of 40 NPDC were eligible for this study. The study followed the guidelines of the declaration of Helsinki. Due to its retrospective nature, it was exempt from formal approval of the local ethical committee.
All CBCT images were taken with a small FOV (cylindrical volumes of 4 × 4 cm, 6 × 4 cm, or 6 × 6 cm) and a basic voxel size of 0.125 or 0.08 mm. Exposure settings were 5.0–7.0 mA and 80 kV with an exposure time of 17.5 s. For the assessment of the cystic volumes, a specialized software was developed in collaboration with Swissmeda AG (Zürich, Switzerland) using reconstructed CBCT slices in a DICOM format with a thickness of 0.5 mm at an interval of 0.5 mm as recommended by the manufacturer. For the analyses, the software was installed on a Dell Precision T3500 workstation (Dell, Round Rock, Texas, USA) with a 19-in. Eizo Flexscan monitor (resolution of 1,280 × 1,024 pixels; Eizo Nanao AG, Wädenswil, Switzerland). First, a planar curve delineating the cystic borders was drawn for all cases manually by the same investigator (V.S.) in the frontal, sagittal, and axial planes of each NPDC included in the study. When the cyst was irregular in shape, two or a maximum of three curves in each respective plane were drawn. Based on this information of a set of closed curves, each lying in a supporting plane, the software program estimated initial surface vectors, and the curves were regularized at interceptions. A radial basis function with compact support is used to define an implicit form of the volume as a zero set of the radial basis function. The zero set is polygonalized by marching tetrahedrons in the bounding box of the curves. The accuracy of the volume is determined by the grid size of the marching tetrahedrons, the support grid of the radial basis functions, and the sampling density of the curves.
The output was a volume (in mm3) interpolating all the given curves. In addition, the longest diameter (in mm) and the surface area (in mm2) of the cyst were calculated. The presence or absence of a root canal filling in all of the maxillary incisors and canines were also recorded. To assess the reproducibility and intra-examiner error, the measurements were repeated a few weeks later by the same observer for 22 randomly selected cases. The observer was blinded to earlier measurements. We limited repeat measurements to 22 based on a sample size calculation (calculated sample size: 20 measurements + 10 % = 22).
The medical files of the included patients were reviewed by the first author (V.S.). Presenting signs and symptoms (e.g., pain, swelling, fistula) in the region of the cyst and postoperative complications were recorded retrospectively from these files. Furthermore, preoperative endodontic treatments and any surgical interventions additional to cystectomy were documented for further analysis.
All data were first analyzed descriptively. To calculate a 95 % confidence interval (CI) of the median, the Clopper-Pearson-Method was used. Wilcoxon rank-sum tests were performed to estimate the influence of gender, age, at least one missing/no missing maxillary incisor (MI)/maxillary canine (MC), edentulous anterior maxilla, root canal filling in MI/MC, preoperative endodontic treatment (PE) in one or more MI/MC, preoperative symptoms and postoperative complications on the diameter, surface, and volume of the cyst. For analysis of age as an influencing factor, the data was divided into two groups (<50 years, ≥50 years). A p value of <0.05 was chosen as the level of significance. To evaluate intra-examiner agreement, Cohen’s kappa values with squared weights (κ) for two raters were calculated by assuming first that the measurements of the cyst dimensions are categorial. Then, by using the squared weights, the importance of the value distance between two data was considered [20]. Furthermore, correlations between diameter, surface, and volume were calculated using Pearson’s correlation coefficients. All tests were performed using the internet-based R software package (R 2.12.1; www.r-project.org).
Results
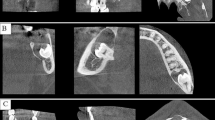
Of the 40 patients, 25 were men and 15 women, resulting in a gender ratio of 1.7:1. The sample age ranged from 7 to 80 years with a mean of 51.3 years (median of 54 years). All NPDCs included were treated by cystectomy. Figure 1 exhibits representative CBCT images of a NPDC taken at the preoperative investigation, and Fig. 2 shows the respective reconstructed 3D image of the cyst.
Preoperative cone beam computed tomography (CBCT) image of a representative NPDC. a The coronal plane showed a round-oval, well-demarcated radiolucency in the central anterior maxilla. On the left side, the nasal opening (foramen of Stenson) of the nasopalatine canal can be seen (yellow arrow). b The axial plane illustrates the well-demarcated radiolucency posterior and adjacent to the roots of the central incisors (both with root canal fillings). c The sagittal plane illustrates the radiolucency posterior to the root of tooth 21, the apex of tooth 21 not being involved in the radiolucency. A root canal filling and a crown are present on tooth 21. The cyst has perforated the cortical bone plate on the palate
Representative 3D reconstruction of a NPDC performed with the specialized software (in collaboration with Swissmeda AG, Zürich, Switzerland) after drawing a planar curve (partly represented by the small orange dots) in each CBCT plane. Both central maxillary incisors had a root canal filling and crowns present. This NPDC has the widest diameter of 14 mm, a surface area of 575 mm2, and a volume of 1,264 mm3 (same case as Fig. 1)
Cyst size, gender, and age
The mean cyst diameter of the series was 15 mm (median 13 mm, range 7–47 mm), the mean cyst surface area 566 mm2 (median 352 mm2, range 84–4,516 mm2), and the mean cyst volume 1,735 mm3 (median 536 mm3, range 65–25,350 mm3; Table 1). There was a strong correlation among the three measurements (diameter and surface area, r = 0.97; diameter and volume, r = 0.93; surface and volume, r = 0.99).
The cyst diameter, surface, and volume for both genders and age groups are shown in Table 2. For gender and age, no statistically significant correlations with the cyst diameter (gender p = 0.23, age p = 0.73), surface area (gender p = 0.38, age p = 0.77), and volume (gender p = 0.36, age p = 0.91) were found. The repeated measurements performed by the same investigator for 22 randomly allocated cases resulted in a mean absolute aberration of ±4.2 % for the volume (κ = 0.99), ±2.8 % for the surface (κ = 0.99), and ±4.9 % for the diameter (κ = 0.74).
Presence/absence of teeth and root canal filling
From a total of 240 possible teeth in the anterior maxillary sextant, 168 (70 %) maxillary incisors and canines were present in the 40 patients (Table 3). Twenty-three patients were partially and seven patients were fully edentulous in the canine to canine region. Root fillings were evident in CBCTs in 15/40 (37.5 %) patients and 25/168 (14.9 %) anterior maxillary teeth (canine to canine). The diameter, surface, and volume of the cysts were not significantly different for edentulous patients or patients with at least one missing MI/MC compared to fully dentate patients in the anterior maxilla (Tables 3 and 4). Furthermore, the presence or absence of a root canal filling in MI/MC had no influence on the cyst dimensions (Tables 3 and 4).
Preoperative endodontic treatment
In 6 patients (15 %) amounting to 10 of 168 (5.9 %) maxillary incisors or canines, an endodontic treatment was necessary before cystectomy due to the close relationship or involvement of the root apices within the cyst lumen (Table 3). In such cases, an endodontic treatment of the respective tooth is usually performed before cystectomy with the advantage of avoiding any contamination or overfilling into the healing bone cavity when performing root canal treatment after cystectomy. The need for a PE had a statistically significant correlation with the diameter (p = 0.003), surface (p = 0.001), and volume (p = 0.001) of the cyst (Table 4).
Preoperative symptoms
Of the 40 included patients, 26 (65 %) had presenting symptoms (Table 3). These being swelling/abscess (n = 7/17.5 %), pressure (n = 5/12.5 %), pain (n = 5/12.5 %), a combination of pain and swelling/abscess (n = 3/7.5 %), a sinus tract (n = 4/10 %), a rotated tooth and pain (n = 1/2.5 %), and a delayed wound healing after an extraction (n = 1/2.5 %). The data analysis resulted in no statistically significant correlation between the presence of presenting symptoms and the cyst dimensions (Table 4).
Immediate and late postoperative complications
Wound healing was uneventful in 26 patients, while 14 patients had the following postoperative complications: bleeding (n = 2/5 %), hypesthesia of the palatal anterior mucosa (n = 4/10 %), devitalisation of a maxillary incisor (n = 2/5 %), persistent sinus tract (n = 2/5 %), infection (n = 2/5 %), and wound dehiscence (n = 1/2.5 %). One late complication was due to an overfilled root canal treatment done after cystectomy necessitating apical surgery including a retrograde root canal sealing (n = 1/2.5 %). There was a statistically significant correlation of the presence of postoperative and late complications with the cyst diameter (p = 0.02), surface area (p = 0.02), and volume (p = 0.02) at the initial evaluation (Tables 3 and 4).
Discussion
CBCT imaging has been proven to be a valuable tool to localize a NPDC within the nasopalatine canal. CBCT enables the analysis of the cyst dimensions, the involvement of neighboring anatomical structures such as teeth or the nasal cavity and assists in surgical treatment planning [14]. Using the software in the present study, a calculation of the volume (mm3) provided appropriate information of the amount of bone lost (osteolysis) due to cyst formation. Our previous reported work on NPDCs was limited to linear measurements performed on CBCTs [14]. To the best of our knowledge, the present clinical study demonstrated for the first time the feasibility of the calculation of a NPDC volume obtained from CBCT images.
Recently, an in vitro study using bovine mandibles calculated the volume of periapical bone defects of different shapes and sizes with impressions made of light-body silicone and correlated these findings to volume data of CBCT images [21]. Similar to the methodology used in the present paper, the border of the radiolucency was delineated on CBCT images by an observer, and a software interpolated the demarcation providing a volume calculation (mm3). Esposito and coworkers [21] demonstrated a good accuracy in the CBCT analyses compared to the physical measurements of the casts of light-body silicone. In the present study, 22 measurements were repeated twice by the same observer for assessment of the intraobserver reproducibility of the calculations. The resulting intra-examiner agreement with a mean aberration of measurements of ±4.9 % for the diameter (κ = 0.74), ±2.8 % for the surface area (κ = 0.99), and ±4.2 % for the volume (κ = 0.99) proves a substantial to almost perfect replication of the methodology. However, there are some limitations in this feasibility study on the novel software presented as only one trained specialist did the drawings. Inter-examiner outcomes, also between general dentists and specialists are of interest for further research. Our data showed also strong correlation between the volume, surface and diameter of the NPDCs analyzed. This can be explained by the fact that many NPDC are almost round in shape (Fig. 2). Thus, the dimensional characteristics studied are clearly correlated. Using the software presented to evaluate irregularly shaped osteolytic bone lesions will be of interest for further research. As the software is calculating the longest diameter based on the defined volume, such information may be more reliable by excluding inherent bias of observers performing linear measurements [22].
Previous experimental studies demonstrated volume measurements of stimulated defects in an acrylic block and a human mandible [23] and of extraction sockets in nine dry skull specimens [24] with specialized software using segmentation techniques. We could not compare and contrast our findings with these earlier experimental studies as the technique used appears different. One recent clinical study including 71 patients with mandibular cysts compared CT- and CBCT-based methods to assess their volume: the first method involved manually outlining the cyst on every fourth axial slice and an interpolarization algorithm to determine the cyst volume. The second method involved the outlining of the cyst in axial, coronal, and sagittal orientation, what seemed to have some similarity to our method [25]. Stoetzer and colleagues [25] suggested that both methods gave similar volume results (p = 0.16). However, no volume data of the cysts were presented in their paper. Furthermore, various other groups estimated volumes of air filled spaces of the nasopharynx with different software calculations based on CBCT images [26–28]. The present methodology for volume analysis may have some limitations due to the export of the data as DICOM files with slices set at 0.5 mm thickness and interval. This standard process is not taking into account the initial pixel/voxel size of the CBCT scans, and there may be some minor inaccuracies using this current work flow. Before applying the software presented on small osteolytic lesions (<5 mm in diameter), it would be beneficial to study the effect of varying slice thicknesses and intervals of the exported DICOM files on the precision of linear and volume measurements.
In the present investigation, the time needed for each volume analysis was not measured in a standardized way. Nevertheless, this data is of great value when applying this software in daily clinical practice. Using the present methodological approach, manual drawings of the cyst borders by a trained and experienced clinician, and application of the software to measure volume, diameter, and surface values of the NPDC took between 5 to a maximum of 20 min per case. For future studies, the variable of time spent per case on the computer needs to be evaluated in more detail.
Attempts have been made to differentiate various jaw pathologies based on CBCT gray values [29]. Especially the differentiation of dental apical lesions between cysts and granulomas has been discussed critically by several groups [30, 31], and histology has been advocated as a gold standard for establishing a final diagnosis [31]. Furthermore, because of the relatively large amount of noise in CBCT scans and because the gray values can be affected by objects outside the FOV, an accurate calibration of CBCT gray values to differentiate pathologies is not possible to date [32].
The male-to-female ratio (1.7:1) of the present case series was in line with the literature, showing ratios varying between 1.2:1 [12, 13] and 3.4:1 [4]. The mean age of 51.3 years was slightly higher than in previous case series [10–14], but there were also publications with a lower (31 years [33], 37.4 years [4]) or higher mean age (54 years [5]). Trauma is considered as a possible etiologic factor for initiating NPDC development. However, our case series showed 46 % of the included patients with no missing MI/MC, illustrating that in these patients, a severe frontal trauma to the face or jaws resulting in a tooth loss could be excluded. Furthermore, cases with at least one root canal filled tooth (37.5 % of patients, 14.9 % of teeth) were in a minority. Both factors, the presence or absence of teeth and root canal filling in MI/MC, do not seem to have an influence on the dimensions of the NPDC in the present study.
No significant correlation between presenting symptoms and the cyst diameter, surface, and volume could be found in the present study. This is in line with earlier works correlating symptoms with diameter measurements on two-dimensional radiographs [5, 12]. Also in our previous study which included 25 NPDCs, no statistically significant correlation could be found between presenting symptoms and the various linear measurement of the NPDC in the CBCT slices [14]. This is of importance to the clinician, as the absence of symptoms does not exclude the presence of a NPDC. If routine 2D radiographic images indicate any signs suspicious of a NPDC, then a CBCT may be indicated for further evaluation and eventual treatment planning.
If the root apices are located within the cyst, a PE of the involved tooth/teeth prior to cystectomy has been advocated [15]. There are clear advantages in performing the root canal filling before cystectomy. During cystectomy, a retrograde inspection is possible, and if necessary a retrograde root canal treatment can be performed. Furthermore, overfilled endodontic material can be removed form the bony lesion during the surgical intervention. In the present study, the PE correlated significantly to the cyst dimensions. That it is necessary to diagnose and treat NPDC at an early state to avoid patient morbidity was confirmed in the present study by the significant correlation of PE to the initial cyst dimension. It has been speculated that NPDCs have a limited growth potential [12]; this seems unlikely when considering the variability and also the maximal dimensions of the included cases (Table 1). Treating small NPDCs also avoids postoperative complications. In the present study, postoperative complications did significantly correlate to the cyst dimension upon initial diagnosis. Only few earlier studies have reported postoperative complications [5, 11]. These involved infections, hemorrhage, paresthesia, and pain, but no analysis of the relation of radiological 2D dimensions to the described complications were performed.
Conclusion
To avoid PE and postoperative complications, NPDCs should be diagnosed and treated at an early stage. CBCT enables analysis of preoperative cyst dimensions and involvement of neighboring anatomical structures. Diameter, surface area, and volume of NPDC can be calculated with a specialized novel software after delineating the cystic borders by planar curves. Accurate information in three dimensions of the amount of bone lost (osteolysis) due to expansion of the cyst could help in personalized treatment planning. In the hands of a single experienced operator, the novel software exhibited good repeatability for the cyst measurements. Further studies are needed to prove the feasibility of this tool for routine analysis of the jaw cyst measurements among generalists and specialists (reproducibility).
References
Kramer IRH, Pindborg JJ, Shear M (1992) The WHO histological typing of odontogenic tumours. A commentary on the Second Edition. Cancer 70:2988–2994
Shear M, Speight P (2007) Nasopalatine duct (incisive canal) cyst. In: Shear M, Speight P (eds) Cysts of the oral and maxillofacial region, 4th edn. Blackwell Publishing Ltd., Oxford, pp 108–118
Daley TD, Wysocki GP, Pringle GA (1994) Relative incidence of odontogenic tumors and oral and jaw cysts in a Canadian population. Oral Surg Oral Med Oral Pathol 77:276–280
Vasconcelos R, de Aguiar MF, Castro W, de Araújo VC, Mesquita R (1999) Retrospective analysis of 31 cases of nasopalatine duct cyst. Oral Dis 5:325–328
Anneroth G, Hall G, Stuge U (1986) Nasopalatine duct cyst. Int J Oral Maxillofac Surg 15:572–580
Abrams AM, Howell FV, Bullock WK (1963) Nasopalatine cysts. Oral Surg Oral Med Oral Pathol 16:306–332
Mealey BL, Rasch MS, Braun JC, Fowler CB (1993) Incisive canal cysts related to periodontal osseous defects: case reports. J Periodontol 64:571–574
Tsuneki M, Maruyama S, Yamazaki M, Abé T, Adeola HA, Cheng J, Nishiyama H, Hayashi T, Kobayashi T, Takagi R, Funayama A, Saito C, Saku T (2013) Inflammatory histopathogenesis of nasopalatine duct cyst: a clinicopathological study of 41 cases. Oral Dis 19:415–424
Main DM (1970) Epithelial jaw cysts: a clinicopathological reappraisal. Br J Oral Surg 8:114–125
Allard RH, van der Kwast WA, van der Waal I (1981) Nasopalatine duct cyst. Review of the literature and report of 22 cases. Int J Oral Surg 10:447–461
Bodin I, Isacsson G, Julin P (1986) Cysts of the nasopalatine duct. Int J Oral Maxillofac Surg 15:696–706
Swanson KS, Kaugars GE, Gunsolley JC (1991) Nasopalatine duct cyst: an analysis of 334 cases. J Oral Maxillofac Surg 49:268–271
Escoda Francolí J, Almendros Marqués N, Berini Aytés L, Gay Escoda C (2008) Nasopalatine duct cyst: report of 22 cases and review of the literature. Med Oral Patol Oral Cir Bucal 13:E438–E443
Suter VG, Sendi P, Reichart PA, Bornstein MM (2011) The nasopalatine duct cyst: an analysis of the relation between clinical symptoms, cyst dimensions, and involvement of neighboring anatomical structures using cone beam computed tomography. J Oral Maxillofac Surg 69:2595–2603
Suter VG, Büttner M, Altermatt HJ, Reichart PA, Bornstein MM (2011) Expansive nasopalatine duct cysts with nasal involvement mimicking apical lesions of endodontic origin: a report of two cases. J Endod 37:1320–1326
Sirotheau Corrêa Pontes F, Paiva Fonseca F, Souza de Jesus A, Garcia Alves AC, Marques Araújo L, Silva do Nascimento L, Rebelo Pontes HA (2014) Nonendodontic lesions misdiagnosed as apical periodontitis lesions: series of case reports and review of literature. J Endod 40:16–27
Frei M, Buettner M, Perren A, Reichart PA, Bornstein MM (2014) Diagnosis and interdisciplinary treatment of a botryoid odontogenic cyst in the posterior mandible: report of a case. Quintessence Int 45:233–237
Loubele M, Bogaerts R, Van Dijck E, Pauwels R, Vanheusden S, Suetens P, Marchal G, Sanderink G, Jacobs R (2009) Comparison between effective radiation dose of CBCT and MSCT scanners for dentomaxillofacial applications. Eur J Radiol 71:461–468
Pauwels R, Beinsberger J, Collaert B, Theodorakou C, Rogers J, Walker A, Cockmartin L, Bosmans H, Jacobs R, Bogaerts R, Horner K (2012) SEDENTEXCT Project Consortium. Effective dose range for dental cone beam computed tomography scanners. Eur J Radiol 81:267–271
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Esposito SA, Huybrechts B, Slagmolen P, Cotti E, Coucke W, Pauwels R, Lambrechts P, Jacobs R (2013) A novel method to estimate the volume of bone defects using cone-beam computed tomography: an in vitro study. J Endod 39:1111–1115
Kosalagood P, Silkosessak OC, Pittayapat P, Pisarnturakit P, Pauwels R, Jacobs R (2014) Linear measurement accuracy of eight cone beam computed tomography scanners. Clin Implant Dent Relat Res. doi:10.1111/cid.12221
Pinsky HM, Dyda S, Pinsky RW, Misch KA, Sarment DP (2006) Accuracy of three-dimensional measurements using cone-beam CT. Dentomaxillofac Radiol 35:410–416
Agbaje JO, Jacobs R, Maes F, Michiels K, van Steenberghe D (2007) Volumetric analysis of extraction sockets using cone beam computed tomography: a pilot study on ex vivo jaw bone. J Clin Periodontol 34:985–990
Stoetzer M, Nickel F, Rana M, Lemound J, Wenzel D, von See C, Gellrich NC (2013) Advances in assessing the volume of odontogenic cysts and tumors in the mandible: a retrospective clinical trial. Head Face Med 9:14
Guijarro-Martínez R, Swennen GR (2011) Cone-beam computerized tomography imaging and analysis of the upper airway: a systematic review of the literature. Int J Oral Maxillofac Surg 40:1227–1237
Sears CR, Miller AJ, Chang MK, Huang JC, Lee JS (2011) Comparison of pharyngeal airway changes on plain radiography and cone-beam computed tomography after orthognathic surgery. J Oral Maxillofac Surg 69:e385–e394
Celikoglu M, Buyuk SK, Sekerci AE, Ucar FI, Cantekin K (2014) Three-dimensional evaluation of the pharyngeal airway volumes in patients affected by unilateral cleft lip and palate. Am J Orthod Dentofacial Orthop 145:780–786
Simon JH, Enciso R, Malfaz JM, Roges R, Bailey-Perry M, Patel A (2006) Differential diagnosis of large periapical lesions using cone-beam computed tomography measurements and biopsy. J Endod 32:833–837
Trope M, Pettigrew J, Petras J, Barnett F, Tronstad L (1989) Differentiation of radicular cyst and granulomas using computerized tomography. Endod Dent Traumatol 5:69–72
Rosenberg PA, Frisbie J, Lee J, Lee K, Frommer H, Kottal S et al (2010) Evaluation of pathologists (histopathology) and radiologists (cone beam computed tomography) differentiating radicular cysts from granulomas. J Endod 36:423–428
Pauwels R, Nackaerts O, Bellaiche N, Stamatakis H, Tsiklakis K, Walker A, Bosmans H, Bogaerts R, Jacobs R, Horner K (2013) SEDENTEXCT Project Consortium. Variability of dental cone beam CT grey values for density estimations. Br J Radiol 86: doi:10.1259/bjr.20120135
Nortjé CJ, Wood RE (1988) The radiologic features of the nasopalatine duct cyst. An analysis of 46 cases. Dentomaxillofac Radiol 17:129–132
Acknowledgments
This study was supported by a grant from the Swiss Association of Dentomaxillofacial Radiology (grant number 13/01). The authors thank Ms. Janine Kuratli, Institute of Mathematical Statistics and Actuarial Science, University of Bern, for her assistance during the statistical analysis.
Ethical approval
The study was reviewed by the ethical committee of the State of Bern but was exempt from formal approval due to its retrospective nature.
Conflict of interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Suter, V.G.A., Warnakulasuriya, S., Reichart, P.A. et al. Radiographic volume analysis as a novel tool to determine nasopalatine duct cyst dimensions and its association with presenting symptoms and postoperative complications. Clin Oral Invest 19, 1611–1618 (2015). https://doi.org/10.1007/s00784-014-1391-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-014-1391-2