Abstract
Objectives
Cone beam computed tomography (CBCT) is frequently used in treatment planning for alveolar bone grafting (ABG) and orthognathic surgery in patients with cleft lip and palate (CLP). CBCT images may depict coincident findings. The aim of this study was to assess the prevalence of incidental findings on CBCT scans in CLP patients.
Subjects and methods
Initial CBCTs taken from consecutive patients (n = 187; mean age 11.7 years, range 6.9–45) with a non-syndromic orofacial cleft from January 2006 until June 2012 were systematically evaluated. Twenty-eight patients (mean age 19.3 years, range 13.2–30.9) had been subjected to ABG before their first CBCT was taken; 61 patients had a CBCT before and after ABG. Sinuses, nasopharynx, oropharynx, throat, skull, vertebrae, temporomandibular joint (TMJ), maxilla and mandible were checked for incidental findings.
Results
On 95.1 % of the CBCTs, incidental findings were found. The most prevalent were airway/sinus findings (56.1 %), followed by dental problems, e.g. missing teeth (52 %), nasal septum deviation (34 %), middle ear and mastoid opacification, suggestive for otitis media (10 %) and (chronic) mastoiditis (9 %), abnormal TMJ anatomy (4.9 %) and abnormal vertebral anatomy (1.6 %). In the 28 patients whose first CBCT was taken at least 2 years after ABG, bone was still present in the reconstructed cleft area except in 2 out of 12 patients with a bilateral CLP. The ABG donor site (all bone grafts were taken from the chin area) was still recognizable in over 50 % of the patients. Based on the CBCT findings, 10 % of the patients were referred for further diagnosis and 9 % for further treatment related to dental problems.
Conclusion
Incidental findings are common on CBCTs. Compared with the literature, CLP patients have more dental, nasal and ear problems. Thus, whenever a CBCT is available, this scan should be reviewed by all specialists in the CLP team focusing on their specific background knowledge concerning symptoms and treatment of these patients.
Clinical relevance
The high number of findings indicates that CBCT imaging is a helpful tool in the treatment of CLP patients not only related to alveolar bone grafting and orthognathic surgery but it also provides diagnostic information for almost all specialties involved in CLP treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cone beam computed tomography (CBCT) was introduced in dentistry in 1997. Since then, CBCT has found its way for various applications within the dental field. Planning for implant treatment seems to be the major reason for CBCT scanning [1–3] followed to a lesser extent by temporomandibular joint (TMJ) diagnostics, suspicion of oral or dental pathology, orthodontics, planning of orthognathic and maxillofacial surgery [4] and impaction of teeth. Though it is expected that cleft lip and palate (CLP) patients could be subjected to a CBCT scan at some point during their treatment, no study has been published yet on incidental findings on CBCT in this particular group of patients.
CLP patients may get a CBCT for planning an alveolar bone graft procedure (ABG) as well as for planning orthognathic surgery. CLP patients concern a relatively young group of patients known to have more ear, nose and throat (ENT) problems [5–8] than children without clefts, because of different anatomy of Eustachian tubes, soft palate muscles and nose. This different anatomy gives rise to middle ear disease, nasal breathing and speech problems [5, 6, 8]. Furthermore, the prevalence of dental anomalies (agenesis, supernumerary teeth) is higher in CLP patients compared to a non-cleft population [9–11].
Recently, several studies have been published about incidental findings on CBCTs [1–3, 12–17]. Though differences exist between the reasons patients were referred for, the applied field of view (FOV) and age of the included subjects, the various studies [1, 3, 12, 13, 15] show that the percentage of incidental findings can be high. All these studies state that dentists, orthodontists and maxillofacial surgeons should study the CBCTs beyond the reason for which the patient is referred, which even may exceed their field of expertise.
Full evaluation of all structures within the FOV is obligatory according to American and European radiology guidelines [18, 19]. Because of the increased application of CBCT in dentistry, the SEDENTEXCT project (www.sedentexct.eu) was started to develop guidelines, which provide evidence and provide training for CBCT use in dentistry. According to the SEDENTEXCT guidelines, the justified use for CBCT in dentistry is limited, because in many situations, clinical evaluation and conventional 2D radiology can give as much information. However, for orthognathic surgery and CLP treatment, the use of a CBCT is justified. Whilst in the latter patients, the use of multi-slice CT scanning (MSCT) was not uncommon; nowadays, CBCT is preferred because of the lower radiation dose.
In the CLP Centre of the Radboud University Nijmegen Medical Centre, CBCT scanning is routinely performed in the planning phase for the bone graft procedure of the alveolar cleft and for the evaluation of the bone graft result (around age 9–12) as well as for the orthognathic surgery planning in these patients. As CLP team members are inclined to look at their primary field of interest, the aim of this study was to assess the occurrence of incidental findings on CBCT performed in CLP patients. This information will be helpful in developing guidelines for reading a CBCT scan in CLP patients.
Materials and methods
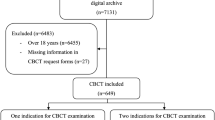
Patients
All consecutive first CBCTs of patients with non-syndromic orofacial clefts (n = 187; 65 girls, 122 boys), taken between 2006 and June 2012, were systematically evaluated. The CBCTs were made with the i-CAT® 3D imaging system (Imaging Sciences International Inc, Hatfield, PA, USA). The reason for the CBCT was planning of the alveolar bone graft procedure or orthognathic surgery. The study population (n = 187 patients; mean 11.7 ± 5 years, range 6.9–45) consisted of 33 patients with unilateral cleft lip and alveolus (UCLA); 86 with unilateral cleft lip, alveolus and palate (UCLP); 37 with bilateral cleft lip, alveolus and palate (BCLP) and 31 with other types of clefts (cleft lip, isolated cleft palate, submucous cleft palate). Of these 187 patients, 28 patients (mean age 19.3 ± 4.4 years, range 13.2–30.9) had already been subjected to an ABG before their first CBCT was taken. Sixty-one patients had a first CBCT before alveolar bone grafting (ABG) and a second one 1 year after ABG. For these patients, the CBCT before and after the ABG were analyzed. In total, 248 CBCTs were scored. The research was conducted in accordance with the Helsinki Declaration with regard to research in human subjects. Approval from the Institutional Review Board was obtained.
Radiographic assessments
All CBCTs were analysed with InVivo Dental software (Anatomage 5, Inc, San Jose, CA, USA) on a 21-in. NEC MultiSync LCD 2190UXp monitor with a resolution of 1,600 × 1,200 pixels (NEC Corp., Tokyo, Japan). The CBCTs were evaluated according to a standardized protocol, in which all structures were screened in the same order (anatomical areas): (1) frontal, ethmoid, sphenoid and maxillary sinuses; (2) nasopharynx, oropharynx, hypopharynx; (3) skull, cervical spine; (4) temporomandibular joint (TMJ); (5) maxilla and (6) mandible. All findings seen on a CBCT were scored. In cases of patients who had been subjected to the ABG procedure, the bone graft was assessed as “bone present” or “bone not present”. Findings were only based on the CBCT, scored and described, and not driven or rectified by clinical observations. After the study, all findings were reported to and verified with the relevant specialist in the CLP team.
All CBCTs were screened independently by two observers (MK and AP) who have different fields of expertise covering the entire field of view. Therefore, their readings were combined, and the final decision on the presence of incidental findings for each image was made in consensus. We repeated the same procedure 2 weeks later on a random sample of 27 CBCT images to determine the intraobserver reliability.
Statistics
Descriptive statistics were used to describe the occurrence of incidental findings. Chi-square tests were used to test if there were differences between the three distinct types of clefts with the largest sample size, i.e. UCLA (33), BCLP (37) and UCLP (86). Chi-square tests were also used to assess any seasonal correlations for sinus and ear findings.
To check for consistency in evaluating CBCTs, kappa statistics were used to measure intraobserver agreement [20].
Results
Error of the method
Intraobserver reliability was good for the sinuses (κ = 0.77), fair to very good for the nasophayrnx, oropharynx and throat (κ = 0.46–1), very good for skull and cervical spine (κ = 0.91–1) and moderate (κ = 0.48) for the TMJ. Intraobserver reliability of kappa for the maxilla ranged from 0.71–1, stating good intraobserver reliability. Reliability for the mandible was moderate to very good (κ = 0.54–1).
General findings
On 95.1 % of the CBCTs, incidental findings were found. When excluding dental problems (agenesis, impaction, supernumeraries, caries), incidental findings were still found on 84.5 % of the CBCTs. Except for the number of pharyngoplasties, there were no significant differences in number and type of findings on CBCTs made in UCLA, UCLP and BCLP patients. The majority of all findings were in the sinuses. No seasonal correlation was observed for sinuses and ears (p = 0.64 and p = 0.73, respectively). Forty-seven patients had findings in only one anatomical area, 59 patients in two, 52 patients in three, 17 patients in four, 1 patient in five and 2 patients in all anatomical areas as categorized by the screening protocol.
ENT
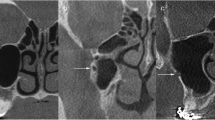
Most incidental findings were related to the sinuses, of which 56.1 %, mainly consisting of different types of mucosal thickening (polipoid, flat, air-fluid levels; Table 1). Further findings in the sinuses were one patient with signs of chronic maxillary sinusitis with alteration of bone and three patients with a hypoplastic maxillary sinus on one side together with an enlarged orbit on the same side. Three patients had mucosal thickening in all sinuses, suggestive for pansinusitis (Fig. 1).
Concerning the nasal cavity, 65 patients had a septum deviation (34 %, of which 5 % severe), 6 with concha bullosa (inflamed in one patient). One patient had a unilateral choanal atresia. Four patients had enlarged tonsils. Eighteen out of 176 (10 %) patients had middle ear opacification, suggestive for otitis media (Fig. 2), and 9 % had mastoid opacification suggestive for (chronic) mastoiditis. Middle ear ossicles were not present in one patient. Eighty-seven (49 %) patients had been treated with a pharyngoplasty; this treatment was significantly more performed in patients with BCLP and UCLP than in UCLA (p = 0.00).
Skull and cervical spine
Seven patients had a persistent metopic suture. In three (1.6 %) of all patients, fused vertebrae were observed, and in three (1.6 %) of the patients, the atlas did not have a normal shape. One patient had a remarkable size difference between the right and left zygomatic archs.
TMJ
In 13 (4.9 %) of all patients, the mandibular condylar head was either remarkably smaller condyle or a flattened compared to the other side.
Maxilla and mandible
The hard palate showed a bony cleft in seven patients, who were clinically diagnosed as having a UCLA or a cleft of the soft palate and not a (submucosal) cleft in the hard palate. With regard to the dental component, 52 % of the patients missed some permanent teeth of which the majority was the lateral incisors (43.8 %). Then, 11.2 % of the patients had supernumerary teeth. For the other incidental maxillary findings, see Table 2 (Fig. 3).
CBCT images (axial, coronal and sagittal) in a patient with a radiopacity, suggestive for an odontoma in the maxilla (arrow) and enostosis in the mandible (blue arrow). As the clinicians to whom this radiopacity was reported did not explore both radiopacities, a final histopathological diagnosis cannot be provided
Main findings in the mandible were agenesis and other dental problems (Table 3). With regard to other findings, two patients had a striking size difference between the left and right ramus. In these two patients, also the mandibular condyle had an abnormal shape which suggested a hemifacial microsomia. For both maxilla and mandible, periapical and periodontal problems only concerned patients older than 17 years of age.
Soft tissue
One patient had a calcification in the cheek at the area of the parotid gland, which could be suggestive for a trauma or a rudimentary ear.
CBCT before and after ABG
Concerning the ABG procedure, in the 28 patients who had been subjected to ABG before the first CBCT was made, in 26 (92.9 %) of them, sufficient bone was still present (for the patients in whom a CBCT before and after ABG was made, see below). Two bone grafts had failed. In all patients, bicortical bone grafts had been taken from the chin area. The mandibular donor site was still recognizable in 54 % (15/28) of the patients at the time of taking the CBCT, 2 years after grafting.
In all but one of the 61 patients of whom the CBCT before and 1 year after ABG was analyzed, bone was present in the former alveolar cleft (98.3 %). In seven ABGs (11.5 %), the vertical height of the bone was limited. During the grafting procedure in about one third of the patients, lateral incisors were removed (18 patients, 29.5 %). In 47 patients (77 %), the donor area was still visible in the mandibular symphysis (in all patients, a bicortical chin bone graft was taken) 1 year post-op (Fig. 4). One enostosis was visible, and one patient had an opacity in the floor of the mouth, suggestive for a sialolith in the ductus Warthoni, one patient had a shortened root of a mandibular incisor. There were no new findings in the TMJ, cervical vertebrae and signs of sinusitis and otitis media for this group of patients when comparing the pre- and post-surgery CBCTs.
Discussion
Publications on CBCT in CLP patients showed that the majority of the CBCT scanning was mainly used in the dental field and focused on the dental/nasal area in the FOV and not on the complete FOV. The mean topics of interest were dental anomalies and the nasal abnormalities [21–30]. No mention was made of any findings outside this area of interest. The current study focused on identifying all anomalies within the complete FOV in young CLP patients. The total number of incidental findings on CBCTs in CLP patients was 95.1 %; these findings included anatomical variations as well as pathology. This high percentage has also been mentioned in other studies with a non-cleft population [1, 3, 12, 15]. The need for monitoring and referral after an incidental finding was noticed, has only been reported as 15.6 and 16.1 %, respectively [3]. After verification of the findings in our study, the majority did not need intervention: 10 % of the patients had to be referred for further diagnosis and 9 % was referred for further treatment, mainly for treatment of dental problems. The other incidental findings did not need further assessments (variations of normal anatomy), or patients were already known for this problem by other specialists.
As mentioned above, most frequent findings were in the airway (sinuses and nose). Considering the ENT problems and the deviating anatomy in CLP patients, this was as expected. Ten percent of the patients had middle ear fluid (otitis media with effusion) with no significant differences between the types of clefts. This phenomenon has not been reported in other studies assessing incidental findings on CBCTs even though other findings in the same FOV were mentioned [1–3, 12–17]. Thus, it is clinically relevant to pay special attention to this anatomical region in CLP patients. Otitis media with effusion in 10 % of the patients and opacification of the mastoid in another 9 % is a clinical relevant finding and in accordance with the study of Timmerman et al. [5], who found an incidence of 13 % otitis media with effusion in a group of 10- to 15-year-old CP patients, in contrast to a much higher incidence at younger ages. Flynn et al. [7] mentioned an even higher percentage of middle ear problems (21–32 %) in this age group, stating the importance of follow-up and indicating that follow-up may be necessary for these patients. Thus, when making a CBCT in CLP patients, attention has to be paid to this region in order to timely refer CLP patients to the ENT specialist.
The mean percentage of findings concerning the sinuses was 56.1 %. Other studies mention a similar high percentage of sinus findings in a non-cleft population [1–3, 12, 15–17], although patients in publications not dealing with clefts had on average a higher age. Though results for sinus findings in younger non-cleft populations show a large variety, 14.3 % in Cha et al. [14] versus 46.8 % in Pazera et al. [13], the percentage found in our CLP group may indicate that sinus findings in this younger age group are more common in a CLP population due to altered anatomy, especially nasal septum deviations. In general, the observed sinus pathology is usually asymptomatic [16], and for the majority of the findings, referral to an ENT specialist is even not necessary. This is in fact the same for CLP patients.
In our group of CLP patients, nasal septum deviation was present in 34 % of the cases. Percentages mentioned in other studies range from 0.1 to 56.7 % but usually concern older patients [12, 14, 15, 31–33]. One study indicates that nasal septum deviation may increase with age [33]. From this point of view, one could speculate that the 34 % found in our study in a young population is already high.
As expected, the majority of our findings in the maxillary and mandibular region concerned teeth. As in other publications, there were more missing teeth, especially lateral incisors, more impacted and supernumerary teeth than in a non-cleft population [3, 9–11]. Knowledge about missing teeth is important for the planning of the orthodontic treatment and may need to be taken into account for the planning of the bone graft procedure. However, there is no indication to make a CBCT scan only for these reasons as these findings usually can also be diagnosed on 2D radiographs.
The donor site in mandibular symphysis of the mandible was still visible in the majority of the patients that had had an ABG procedure. As it concerns a bicortical graft, this is a feature that could be expected [34].
A drawback of the current study was that no control group was available as in our clinic and no CBCT scans are made in a population younger than 11 years of age unless they have specific maxillofacial anomalies (like CLP or a syndrome). Also, the other studies on incidental findings on CBCTs reported in literature mainly included older patients (30.3–64.7 years) and concerned non-cleft populations.
The high percentage of total findings (95.1 %) in the current study was comparable to those reported in non-cleft populations by Allareddy et al. [1] (94.3 %), Price et al. [3] (90.7 %), Pette et al. [12] (93.4 %) and Cağlayan and Tozoğlu [15] (92.8 %). This observation was unexpected because the only study reported in the literature on younger non-cleft patients [14] showed a lower percentage of 21.6 %. Even though the smaller FOV used in the study of Cha et al. [14] may be an explanation for the lower percentage of findings reported in that study, the percentage of findings within the FOV used by Cha et al. [14] was still remarkably lower than the findings found in similar areas in our study. Some of the findings in the other studies showed age-related problems which one would not expect in a young population (in this study, mean age was 11.7 years). Pette et al. [12] mentioned a clear correlation between type of finding and age, showing that more degenerative problems, vascular problems and calcifications are to be expected and found at an higher age. These findings (calcifications, degenerative problems in TMJ and vertebrae, vascular problems) comprise a large number of the findings in all the studies with an older age group [1, 3, 12], whereas in our study, these problems were not seen. The main reason for the high score in our CLP population was de nasal septum deviation when compared to the other studies.
The association between the younger age group and sinus problems and cysts as mentioned by Pette et al. [12] was the same in our CLP group, except that in our CLP group, no cysts were found. The high percentage of sinus findings in a young population was also verified by Pazera et al. [13] in a non-cleft population.
One in ten patients had an ear problem, and 1 in 11 (chronic) had mastoiditis. This is of importance because CLP patients do have more ENT problems. Remarkably, none of the other studies on incidental findings on CBCTs of the head neck region reported on otitis media and (chronic) mastoiditis, while these areas will have been included in the FOV of those studies. Thus, either the researchers that studied those CBCTs were unfamiliar with the radiological signs of otitis media and (chronic) mastoiditis on CBCTs or focused themselves too much on the anatomical area of their interest. The latter supports our view that CBCTs should be reviewed by clinicians and/or radiologists with a special expertise in the areas included in the FOV.
Some problems did occur in judging the findings on the CBCT as the observers had no knowledge of the patients’ files. In some of the patients that were referred for ENT or maxillofacial pathology, e.g. chronic sinusitis and abnormal bone anatomy, the pathology appeared to be the result of surgical treatment, identifying the need for review of the CBCT by specialists familiar with the CLP patient and the treatment.
Above mentioned problems and findings specific for the CLP population indicate that thorough analysis of the CBCT by all specialists participating in the CLP team is important, because knowledge of manifestations of CLP on CBCTs and their treatment is necessary when judging the CBCT. Because of the multidisciplinary nature of these patients, the specialists in the CLP team should read the CBCT systematically according to a standardized protocol. Our findings show that in CLP patients, an extended FOV may have added value as diagnostic information becomes available that is also useful for other specialists concerned with the treatment.
Conclusions
The prevalence of incidental CBCT findings is more than three times higher in CLP patients compared to healthy youngsters. Many of these findings are related to CLP problems like middle ear and mastoid problems, agenesis of teeth, supernumerary and impacted teeth. Some of the incidental findings show that specific background knowledge of cleft related problems and effects of CLP treatment is necessary for adequate diagnosis. Thus, CBCT examination in patients with clefts asks for careful and thorough interpretation by the participating medical specialists of the CLP team.
References
Allareddy V, Vincent SD, Hellstein JW, Qian F, Smoker WR, Ruprecht A (2012) Incidental findings on cone beam computed tomography images. Int J Dent 2012:871532. doi:10.1155/2012/871532, Epub 2012 Dec 10
Rege IC, Sousa TO, Leles CR, Mendonça EF (2012) Occurrence of maxillary sinus abnormalities detected by cone beam CT in asymptomatic patients. BMC Oral Health 10:12–30
Price JB, Thaw KL, Tyndall DA, Ludlow JB, Padilla RJ (2012) Incidental findings from cone beam computed tomography of the maxillofacial region: a descriptive retrospective study. Clin Oral Implants Res 23:1261–1268
Plooij JM, Maal TJ, Haers P, Borstlap WA, Kuijpers-Jagtman AM, Bergé SJ (2011) Digital three-dimensional image fusion processes for planning and evaluating orthodontics and orthognathic surgery. A systematic review. Int J Oral Maxillofac Surg 40:341–352
Timmerman K, Vander Poorten V, Desloovere C, Debruyne F (2006) The middle ear in cleft palate patients in their early teens: a literature study and preliminary file study. B-ENT 2(Suppl 4):95–101
Sheahan P, Miller I, Sheahan JN, Earley MJ, Blayney AW (2003) Incidence and outcome of middle ear disease in cleft lip and/or cleft palate. Int J Pediatr Otorhinolaryngol 67:785–793
Flynn T, Lohmander A, Moller C, Magnusson L (2013) A longitudinal study of hearing and middle ear status in adolescents with cleft lip and palate. Laryngoscope 23:1374–1380
Hocevar-Boltezar I, Jarc A, Kozelj V (2006) Ear, nose and voice problems in children with orofacial clefts. J Laryngol Otol 120:276–281
Polder BJ, Van ‘t Hof MA, Van der Linden FP, Kuijpers-Jagtman AM (2004) A meta-analysis of the prevalence of dental agenesis of permanent teeth. Commun Dent Oral Epidemiol 32:217–226
Tannure PN, Oliveira CA, Maia LC, Vieira AR, Granjeiro JM, de Castro CM (2012) Prevalence of dental anomalies in nonsyndromic individuals with cleft lip and palate: a systematic review and meta-analysis. Cleft Palate Craniofac J 49:194–200
Tortora C, Meazzini MC, Garattini G, Brusati R (2008) Prevalence of abnormalities in dental structure, position, and eruption pattern in a population of unilateral and bilateral cleft lip and palate patients. Cleft Palate Craniofac J 45:154–162
Pette GA, Norkin FJ, Ganeles J, Hardigan P, Lask E, Zfaz S, Parker W (2012) Incidental findings from a retrospective study of 318 cone beam computed tomography consultation reports. Int J Oral Maxillofac Implants 27:595–603
Pazera P, Bornstein MM, Pazera A, Sendi P, Katsaros C (2011) Incidental maxillary sinus findings in orthodontic patients: a radiographic analysis using cone-beam computed tomography (CBCT). Orthod Craniofacial Res 14:17–24
Cha JY, Mah J, Sinclair P (2007) Incidental findings in the maxillofacial area with 3-dimensional cone-beam imaging. Am J Orthod Dentofac Orthop 132:7–14
Cağlayan F, Tozoğlu U (2012) Incidental findings in the maxillofacial region detected by cone beam CT. Diagn Interv Radiol 18:159–163
Gracco A, Incerti Parenti S, Ioele C, Alessandri Bonetti G, Stellini E (2012) Prevalence of incidental maxillary sinus findings in Italian orthodontic patients: a retrospective cone-beam computed tomography study. Korean J Orthod 42:329–334
Ritter L, Lutz J, Neugebauer J, Scheer M, Dreiseidler T, Zinser MJ, Rothamel D, Mischkowski RA (2011) Prevalence of pathologic findings in the maxillary sinus in cone-beam computerized tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 111:634–640
Carter L, Farman AG, Geist J, Scarfe WC, Angelopoulos C, Nair MK, Hildebolt CF, Tyndall D, Shrout (2008) American Academy of Oral and Maxillofacial Radiology executive opinion statement on performing and interpreting diagnostic cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 106:561–562
Horner K, Islam M, Flygare L, Tsiklakis K, Whaites E (2009) Basic principles for use of dental cone beam computed tomography: consensus guidelines of the European Academy of Dental and Maxillofacial Radiology. Dentomaxillofac Radiol 38:187–195
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Miyamoto J, Nagasao T, Nakajima T, Ogata H (2007) Evaluation of cleft lip bony depression of piriform margin and nasal deformity with cone beam computed tomography: “retruded-like” appearance and anteroposterior position of the alar base”. Plast Reconstr Surg 120:1612–1620
Miyamoto J, Nakajima T (2010) Anthropometric evaluation of complete unilateral cleft lip nose with cone beam CT in early childhood. J Plast Reconstr Aesthet Surg 63:9–14
Nagasao T, Miyamoto J, Hikosaka M, Yoshikawa K, Ishii N, Nakajima T (2008) A new method to quantify subtle morphological deformities in nasal profile curvatures and its application for analysis of unilateral cleft lip noses. J Craniomaxillofac Surg 36:321–334
Oberoi S, Gill P, Chigurupati R, Hoffman WY, Hatcher DC, Vargervik K (2010) Three-dimensional assessment of the eruption path of the canine in individuals with bone-grafted alveolar clefts using cone beam computed tomography. Cleft Palate Craniofac J 47:507–512
Garib DG, Yatabe MS, Ozawa TO, Da Silva Filho OG (2012) Alveolar bone morphology in patients with bilateral complete cleft lip and palate in the mixed dentition: cone beam computed tomography evaluation.”. Cleft Palate Craniofac J 49:208–214
Li F, Wang JG (2011) Measurement of tooth length of upper canines in complete unilateral cleft lip and palate patients with cone-beam computed tomography. Hua Xi Kou Qiang Yi Xue Za Zhi 29(161–163):167
Padricelli G, Monsurro A, Grassia V, Perillo L (2012) The frequency of dental anomalies in subjects with cleft lip and palate. Mondo Ortodontico 37:46–55
Cheung T, Oberoi S (2012) Three dimensional assessment of the pharyngeal airway in individuals with non-syndromic cleft lip and palate. PLoS ONE 7:e43405
Yoshihara M, Terajima M, Yanagita N, Hyakutake H, Kanomi R, Kitahara T, Takahashi I (2012) Three-dimensional analysis of the pharyngeal airway morphology in growing Japanese girls with and without cleft lip and palate. Am J Orthod Dentofac Orthop 141:S92–S101
Zhou W, Li W, Lin J, Liu D, Xie X, Zhang Z (2012) Tooth lengths of the permanent upper incisors in patients with cleft lip and palate determined with cone beam computed tomography. Cleft Palate Craniofac J 50:88–95
Stefanini R, Tufik S, Soares MC, Haddad FL, Bittencourt LR, Santos-Silva R, Gregorio LC (2012) Systematic evaluation of the upper airway in the adult population of São Paulo, Brazil. Otolaryngol Head Neck Surg 146:757–763
Yiğit O, Acioğlu E, Cakir ZA, Sişman AS, Barut AY (2010) Concha bullosa and septal deviation. Eur Arch Otorhinolaryngol 267:1397–1401
Reitzen SD, Chung W, Shah AR (2011) Nasal septal deviation in the pediatric and adult populations. Ear Nose Throat J 90:112–115
Dik EA, de Ruiter AP, van der Bilt A, Koole R (2010) Effect on the contour of bone and soft tissue one year after harvesting chin bone for alveolar cleft repair. Int J Oral Maxillofac Surg 39:962–967
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kuijpers, M.A.R., Pazera, A., Admiraal, R.J. et al. Incidental findings on cone beam computed tomography scans in cleft lip and palate patients. Clin Oral Invest 18, 1237–1244 (2014). https://doi.org/10.1007/s00784-013-1095-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-013-1095-z